Ciwon ciki
| Ciwon ciki | |
|---|---|
 | |
| Description (en) | |
| Iri |
pain (en) abdominal symptom (en) |
| Medical treatment (en) | |
| Magani |
cajeput oil (en) |
| Identifier (en) | |
| ICD-10 | R10 |
| ICD-9 | 789.0 |
| DiseasesDB | 14367 |
| MedlinePlus | 003120 |
| eMedicine | 003120 |
| MeSH | D015746 |
Ciwon ciki kokuma ciwon mara. Alamu da bayyanar cututtuka sun haɗa da ciwon ciki, taushi, rigidity, da kunnuwan ciki na waje. Matsalolin na iya haɗawa da asarar jini da kamuwa da cuta.
Ganowa na iya haɗawa da ultrasonography, lissafin lissafi, da lavage peritoneal, kuma jiyya na iya haɗawa da tiyata.[1] Ya kasu zuwa nau'i biyu a hankali ko shiga kuma yana iya haɗawa da lalacewa ga sassan ciki.[2] Raunin ƙananan ƙirji na iya haifar da rauni na splenic ko hanta[3].
Alamomi
[gyara sashe | gyara masomin]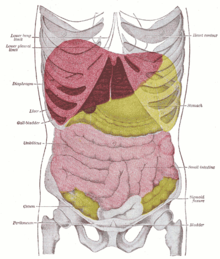
Ba a ganin alamun bayyanar cututtuka a farkon kwanakin kuma bayan wasu kwanaki ana ganin zafi na farko. Mutanen da suka ji rauni a karon abin hawa na iya kasancewa tare da "alamar bel din wurin zama", rauni a cikin ciki tare da wurin bangaren cinya na bel din aminci; wannan alamar tana da alaka da yawan rauni ga gabobin ciki [4]. Wurin zama na iya haifar da abrasions da hematomas; kusan kashi 30 cikin 100 na mutanen da ke da irin wadannan alamun sun hadu da raunin ciki [5]. Alamun farko na ciwon ciki sun hada da tashin zuciya, amai, jini a cikin fitsari, da zazzabi.[4][6] Raunin na iya kasancewa tare da ciwo na ciki, taushi, [7] distension, ko rigidity ga tabawa, kuma sautin hanji na iya raguwa ko babu. Tsaron ciki shine taurin tsokar bangon ciki don kiyaye gabobin da ke cikin ciki.
Pneumoperitoneum, iska ko iskar gas a cikin rami na ciki, na iya zama alamar fashewar gabar gaba. A cikin raunuka masu shiga, fitar (fitowar gabobin ciki daga rauni) na iya kasancewa.[8]
Raunin da ke tattare da raunin ciki a ciki ya hada da karaya na hakarkari, raunin kashin baya, raunin kwankwasa, da raunin bangon ciki.[9]
Dalilai
[gyara sashe | gyara masomin]Hadarin ababen hawa abu ne na yau da kullun na raunin raunin ciki. Belin kujeru yana rage yawan raunuka kamar raunin kai da raunin kirji, amma suna ba da barazana ga gabobin ciki kamar su pancreas da hanji, wadanda za a iya raba su ko kuma a matse su a kan kashin baya. Yara suna da rauni musamman ga raunin ciki daga bel din kujera, saboda suna da yankuna masu laushi na ciki kuma ba a tsara bel din kujera don dacewa da su ba. A cikin yara kuma, hatsabibin kekuna yakan zama sanadin raunin ciki, musamman lokacin da abin hannu ya bugi ciki. Raunin wasanni na iya shafar gabobin ciki irin su sawa da koda.[4] Faduwa da wasanni suma hanyoyi ne na yawan raunin ciki a cikin yara.[4] Raunin ciki na iya haifar da cin zarafin yara kuma shine na biyu mafi girma na sanadin mutuwar yara dangane da cin zarafin yara, bayan raunin da ya ji rauni a kwakwalwa. Raunin harbin bindiga, wanda ya fi karfin wuka, yawanci ya fi na baya lalacewa.
Raunin harbin bindiga da ya ratsa cikin peritoneum yana haifar da babbar illa ga manyan sifofin ciki a wasu kashi 90 na lokuta.[5]
Pathophysiology
[gyara sashe | gyara masomin]Ciwon ciki na iya zama barazana ga rayuwa saboda gabobin ciki, musamman wadanda ke cikin sararin sama, na iya zubar da jini mai yawa, kuma sararin samaniya yana iya daukarjini mai yawa. Gabobin ciki masu kauri, kamar hanta da koda, suna zubar da jini da yawa idan an yanke ko tsagewa, kamar yadda manyan hanyoyin jini kamar su aorta da vena cava suke yi. Gabobin gabobi kamar ciki, yayin da ba zai iya haifar da firgita daga yawan zubar jini ba, suna ba da hadarin kamuwa da cuta mai tsanani, musamman idan irin wannan rauni ba a Yi gaggawar magance shi ba.[6] Gabobin ciki irin su hanji na iya zubar da abin da ke cikin su zuwa cikin kogon ciki. Zubarjini da kamuwa da cuta a cikin jiki sune manyan abubuwan da ke haifar da mace-mace da ke haifar da rauni a cikin ciki.
Daya ko fiye daga cikin gabobin ciki na iya samun rauni a raunin ciki. An kayyade halayen raunin da ya faru a wani bangare na abin da gabobin jiki ko gabobin suka ji rauni.
Hanta
[gyara sashe | gyara masomin]Hanta, wadda ita ce mafi raunin gabobin ciki ga kowane nau'i na rauni saboda girmanta da wurin da take (a cikin kusurwar dama ta sama na cikin ciki), ta ji rauni a kusan kashi biyar cikin dari na duk mutanen da aka kwantar da su a asibiti saboda rauni.[7] Raunin hanta yana haifar da mummunar hadari ga girgiza saboda hanta yana da laushi kuma yana da wadataccen jini da iya aiki. Hanta na iya zama tsinke ko tashe, kuma hematoma na iya tasowa[13]. Yana iya zubar da bile, yawanci ba tare da wani mummunan sakamako ba.[13] Idan an ji rauni mai tsanani, hanta na iya haifar da exsanguination (jini har mutuwa), yana bukatar tiyatar gaggawa don dakatar da jinin.[9]
Saifa
[gyara sashe | gyara masomin]Saifa shine mafi yawan sanadin zubar da jini mai yawa a cikin rauni mara kyau na ciki zuwa ga tafsirin gaba. Sofa ita ce gabobin da aka fi samun rauni. Ana iya haduwa da laceration na splin tare da hematoma.[13] Saboda iyawar da majiyar ke iya zubar da jini mai yawa, tsautsayi na iya zama barazana ga rayuwa, yana haifar da firgita. Koyaya, ba kamar hanta ba, shiga cikin rauni ga barna, pancreas da koda ba sa haifar da barazanar firgita nan da nan sai dai idan sun lalata babban jigon jini da ke ba da gabobin jiki, kamar jijiyar koda.[5] Karaya na kananan hakarkari na hagu yana da alaka da laceration na splin a cikin kashi 20 na lokuta.[9]
Pancreas
[gyara sashe | gyara masomin]Ana iya raunata kwayar cuta na pancreas a cikin rauni na ciki, misali ta laceration ko tashewa.[4] Raunin pancreatic, wanda aka fi sani da hadarin keke (musamman ta hanyar tasiri tare da sanduna) a cikin yara da kuma hadarin mota a cikin manya, yawanci suna faruwa a kebe a cikin yara kuma tare da wasu raunuka a cikin manya. [4] Alamun da ke nuna cewa pancreas ya sami rauni sun hada da habakawa da kasancewar ruwa a kusa da pancreas.
koda
[gyara sashe | gyara masomin]
Hakanan ana iya ji rauni a kodan; suna da dan kadan amma ba hakarkarinsu ya kare su gaba daya ba[6]. Hakanan ana iya samun raunin koda da tashin hankali.[13]. Raunin koda, abin da aka saba gani a yara masu rauni a ciki, na iya hadawa da fitsari mai jini.[13] Ana iya haduwa da raunin koda da fitsari ko zubar fitsari a cikin ciki. [4] Koda da aka karye ita ce wadda ke da lacers da yawa da kuma abin da ke da alaka da guguwar kwayar koda.[4]
Hanji
[gyara sashe | gyara masomin]Karamin hanji yana daukar wani bangare mai yawa na ciki kuma ana iya lalacewa ta hanyar rauni.[5]. Ana iya toshe hanji[4]. Ana fahimtar iskar gas a cikin rami na ciki da aka gani akan CT alama ce ta gano hudar hanji; duk da haka ana iya haifar da iskar cikin ciki ta hanyar pneumothorax (iska a cikin rami mai zurfi a waje da huhu wanda ya tsere daga tsarin numfashi) ko pneumomediastinum (iska a cikin mediastinum, tsakiyar kogin kirji).[4]. Ba za a iya gano raunin akan CT ba.[4] Raunin hanji yana iya hadawa da rikitarwa kamar kamuwa da cuta, kumburin ciki, toshe hanji, da samuwar yoyon fitsari.[4] Hurar hanji na bukatar tiyata.[4]
Bincike
[gyara sashe | gyara masomin]Kashi goma cikin dari na mutanen da ke da polytrauma wadanda ba su da alamun raunin ciki sun sami shaidar irin wannan raunin ta hanyar amfani da hoton rediyo.[l] Dabarun bincike da aka yi amfani da su sun hada da duban CT, duban dan tayi, [1] da Xray.[7] X-ray na iya taimakawa wajen tantance hanyar abu mai ratsawa da gano duk wani abu na waje da ya rage a cikin rauni, amma maiyuwa ba zai taimaka wajen raunin da ya faru ba.[7] Hakanan za'a iya yin laparoscopy na bincike ko binciken laparotomy idan wasu hanyoyin bincike ba su ba da sakamako na karshe ba.[5]
Ultrasound
[gyara sashe | gyara masomin]Ultrasound na iya gano ruwa kamarjini ko abun ciki na ciki a cikin kogon ciki, [1] kuma hanya ce mara lalacewa kuma tana da lafiya.[4] Binciken CT shine dabarar da aka fi so ga mutanen da ba su cikin hadarin girgiza kai tsaye, amma tun da ana iya yin duban dan tayi daidai a cikin dakin gaggawa, ana ba da shawarar na karshen ga mutanen da ba su da kwanciyar hankali don matsawa zuwa duba CT.[I]. Na'urar duban dan tayi na aľada baya kawar da duk raunuka.[8]
CT
[gyara sashe | gyara masomin]Mutanen da ke fama da ciwon ciki akai-akai suna bukatar gwajin CT don wasu rauni (misali, CT kai ko kirji); a cikin wadannan lokuta ana iya yin CT na ciki a lokaci guda ba tare da bata lokaci ba a kulawar majiyyaci.[4]
CT yana iya gano kashi 76% na raunukan da ba a iya gani ba don haka ana Iura da mutanen da ba su da kyau kuma a sake duba su idan sun lalace.[15] Duk da haka, an nuna CT yana da amfani wajen tantance mutanen da ke da wasu nau'o'in ciwon ciki don guje wa laparotomy mara amfani, wanda zai iya kara yawan farashi da tsawon lokacin asibiti.[1 6]. Meta-bincike na amfani da CT a cikin shiga cikin raunin ciki ya nuna hankali, kayyadaddun kayyadaddun bayanai da daidaito>= 95%, tare da PPV na 85 0/0 da NPV na Wannan yana nuna cewa CT yana da kyau don guje wa laparotomy mara amfani amma dole ne a kara shi ta wasu ka'idodin asibiti don kayyade bukatar binciken tiyata (23.37 tabbataccen ra'ayi mai yiwuwa, 0.05 rashin yiwuwar rabo mai kyau).
Peritoneal lavage
[gyara sashe | gyara masomin]Ciwon bacin rai wata dabara ce mai jayayya amma ana iya amfani da ita don gano rauni ga gabobin ciki: ana sanya catheter a cikin kogon peritoneal, kuma idan akwai ruwa a ciki, sai a nemi jini ko shaidar fashewar gabobi.[l] Idan wannan bai bayyana shaidar rauni ba, ana shigar da salin bakararre a cikin rami kuma a kwashe a duba jini ko wani abu.[l ] Yayin da lavage peritoneal hanya ce madaidaiciya don gwada zubar jini, yana dauke da hadarin cutar da gabobin ciki, yana iya zama da wahala a yi, kuma yana iya haifar da tiyata ba dole ba; don haka an maye gurbinsa da duban dan tayi a Turai da Arewacin Amurka.
Rabewa
[gyara sashe | gyara masomin]Ciwon ciki ya kasu kashi-kashi da nau'in shiga. Yayin da ake gano ciwon ciki (PAT) yawanci bisa la'akari da alamun asibiti, ganewar ciwon ciki mara kyau yana iya yiwuwa a jinkirta ko kuma a rasa gaba daya saboda alamun asibiti ba su da yawa.[l] Raunin da ba a iya gani ba ya fi yawa a yankunan karkara, yayin da masu shiga suka fi yawa a cikin birane.[5] Ciwon raunin da ya faru ya kasu kashi biyu zuwa raunukan wuka da raunin harbin bindiga, wadanda ke bukatar hanyoyin magani daban-daban.[7]
Magani
[gyara sashe | gyara masomin]Ciwon ciki yana bukatar kulawar gaggawa ta likita kuma wani lokaci yana bukatar asibiti. Magani na farko ya kunshi daidaitawa mutum isa don tabbatar da isassun iskar iska, numfashi, da zagayawa, da gano wasu raunuka.[7] Ana iya bukatar tiyata don gyara sassan da suka ji rauni. Binciken tiyata na iya zama larura ga mutanen da ke da raunin shiga da kuma alamun peritonitis ko girgiza.[5] Ana Yin laparotomy sau da yawa a cikin raunin ciki mara kyau, kuma ana bukatar gaggawa idan raunin ciki ya haifar da babban jini mai yuwuwar mutuwa.[1][5]. Babban manufar ita ce dakatar da duk wata hanyar zub da jini kafin a matsa zuwa ga wani tabbataccen abin da aka gano da kuma gyara duk wani rauni da aka samu.[18] Saboda yanayin kula da lokaci, wannan hanya kuma tana ba da fifiko ta fuskar samun dama da sarrafa zubarjini, don haka yana ba da fifikon tsinkayar tsaka mai tsayi[19]. Har ila yau ana samun nasarar magance raunin da ke cikin ciki ba tare da tiyata ba saboda babu wani fa'ida kadan da aka nuna idan babu wani sanannen jini mai aiki ko yiwuwar kamuwa da cuta.[7][4][20] Yin amfani da CT scan yana ba masu ba da kulawa damar yin amfani da kananan tiyata saboda suna iya gano raunin da za a iya sarrafa su ta hanyar ra'ayin mazan jiya da kuma kawar da wasu raunin da zai bukaci tiyata.[7] Dangane da raunin da ya faruy mutum yana iya ko baya bukatar kulawa mai zurfi[4].
Idan ba a gano raunin ciki da sauri bay ana danganta sakamako mafi muni.[l ] Jinkirin jinkiri yana da alaka da kamuwa da cuta ta musamman da kuma mace-mace idan an shiga cikin hudar kwayar cuta.[13]
Manazarta
[gyara sashe | gyara masomin]- ↑ Jansen JO, Yule SR, Loudon MA (April 2008). "Investigation of blunt abdominal trauma". BMJ. 336 (7650): 938–42. doi:10.1136/bmj.39534.686192.80. PMC 2335258. PMID 18436949.
- ↑ Fitzgerald, J.E.F.; Larvin, Mike (2009). "Chapter 15: Management of Abdominal Trauma". In Baker, Qassim; Aldoori, Munther (eds.). Clinical Surgery: A Practical Guide. CRC Press. pp. 192–204. ISBN 9781444109627.
- ↑ Wyatt, Jonathon; Illingworth, RN; Graham, CA; Clancy, MJ; Robertson, CE (2006). Oxford Handbook of Emergency Medicine. Oxford University Press. p. 346. ISBN 978-0-19-920607-0.
- ↑ Bixby SD, Callahan MJ, Taylor GA (January 2008). "Imaging in pediatric blunt abdominal trauma". Semin Roentgenol. 43 (1): 72–82. doi:10.1053/j.ro.2007.08.009. PMID 18053830.
- ↑ Lichtenstein R, Suggs AH (2006). "Child abuse/assault". In Olshaker JS, Jackson MC, Smock WS (eds.). Forensic Emergency Medicine: Mechanisms and Clinical Management (Board Review Series). Hagerstown, MD: Lippincott Williams & Wilkins. pp. 157–9. ISBN 978-0-7817-9274-5. Archived from the original on 2017-11-06. Retrieved 2008-06-21.
- ↑ Blank-Reid C (September 2006). "A historical review of penetrating abdominal trauma". Crit Care Nurs Clin North Am. 18 (3): 387–401. doi:10.1016/j.ccell.2006.05.007. PMID 16962459.
- ↑ Fabian TC, Bee TK (2004). "Liver and biliary trauma". In Moore EJ, Feliciano DV, Mattox KL (eds.). Trauma. New York: McGraw-Hill, Medical Pub. Division. p. 637. ISBN 978-0-07-137069-1. Archived from the original on 2017-11-06. Retrieved 2008-06-21.
- ↑ Stengel, D; Leisterer, J; Ferrada, P; Ekkernkamp, A; Mutze, S; Hoenning, A (12 December 2018). "Point-of-care ultrasonography for diagnosing thoracoabdominal injuries in patients with blunt trauma". The Cochrane Database of Systematic Reviews. 12 (12): CD012669. doi:10.1002/14651858.CD012669.pub2. PMC 6517180. PMID 30548249.
