Ciwace Ciwacen daji Surface epithelial-stromal
| Ciwace Ciwacen daji Surface epithelial-stromal | |
|---|---|
| Description (en) | |
| Iri |
ovarian neoplasm (en) carcinoma (en) |
| Specialty (en) | oncology |
| Identifier (en) | |
| ICD-9-CM | 239.5 |
| ICD-10 | C56 da D27 |
| ICD-9 | 183 da 220 |
| MeSH | C538090 |
| Disease Ontology ID | DOID:2152 |
Surface epithelial-stromal ciwace-ciwacen daji rukuni ne na neoplasms na ovarian wanda zai iya zama mara kyau ko m . Neoplasms a cikin wannan rukuni ana tsammanin an samo su ne daga epithelium na ovarian (gyaran peritoneum ) ko daga ectopic endometrial ko tube na fallopian (tubal). Ciwon daji na irin wannan kuma ana kiransa ovarian adenocarcinoma .[1] Wannan rukuni na ciwace-ciwacen daji yana da kashi 90% zuwa 95% na duk lokuta na ciwon daji na ovarian ; duk da haka ana samun su ne kawai a cikin matan da suka shude amma ban da Amurka inda kashi 7% na al'amuran ke faruwa a mata 'yan kasa da shekaru 40.[2][3][4][5][6][7]Serum CA-125 sau da yawa yana haɓaka amma yana da daidai 50% kawai don haka ba alamar ƙwayar cuta ba ce mai amfani don tantance ci gaban jiyya. 75% na mata masu ciwon daji na ovarian suna samuwa a cikin matakan ci gaba; duk da haka ƙananan marasa lafiya suna iya samun kyakkyawan tsinkaye fiye da tsofaffi marasa lafiya. [8] [9] [10] [11] [12]
Rabewa
[gyara sashe | gyara masomin]
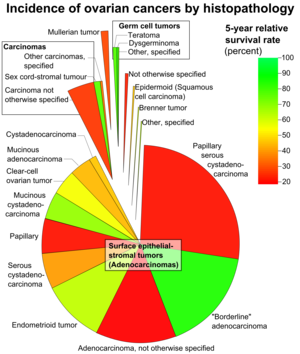
Epithelial - stromal ciwace -ciwacen daji an rarraba su akan nau'in Siffofin ƙwayoyin cuta na ƙananan ƙwayoyin cuta suna ƙayyade ko ƙwayar cuta ta epithelial-stromal ba ta da kyau, ƙwayar iyaka, ko m (shaida ta malignancy da stromal mamayewa). Ciwon daji na kan iyaka yana da yuwuwar rashin tabbas.
Wannan rukuni ya ƙunshi serous, mucinous, endometrioid, fili cell, da kuma brenner (transitional cell) ciwace-ciwacen daji, ko da yake akwai 'yan gauraye, undifferentiated da unclassified iri.
Ciwon daji mai tsanani
[gyara sashe | gyara masomin]
- Wadannan ciwace-ciwacen sun bambanta da girma daga ƙanana kuma kusan ba a iya gane su zuwa babba, suna cika rami na ciki.
- iyaka, da kuma nau'in ciwon daji na ciwon daji suna da kimanin kashi 30% na dukan ciwace-ciwacen daji na ovarian.
- Kashi 75% na marasa lafiya ne ko kuma na iyakoki, kuma kashi 25% na mugunya ne
- Mummunan nau'i na wannan ƙwayar cuta, serous cystadenocarcinoma, yana da kimanin kashi 40 cikin dari na dukkanin carcinomas na ovary kuma sune mafi yawan ciwon daji na ovarian.
- Ciwon daji mara kyau da kan iyakoki sun fi yawa a tsakanin shekaru 20 zuwa 50.
- M serous ciwace-ciwacen daji faruwa daga baya a rayuwa a kan matsakaita, ko da yake da ɗan a baya a cikin iyali lokuta.
- 20% na benign, 30% na kan iyaka, da 66% na m ciwace-ciwacen daji ne na biyu (shafi duka ovaries).
Abubuwan da zasu iya haɗawa da:
- wuraren cystic
- wuraren cystic da fibrous
- galibin wuraren fibrous
Damar mummunan ciwon ƙwayar cuta yana ƙaruwa tare da adadin wurare masu ƙarfi da ke samuwa, ciki har da tsarin papillary da duk wani nau'i na necrotic.
Pathology
[gyara sashe | gyara masomin]- an yi layi da tsayi, columnar, sel epithelial ciliated
- cike da ruwa mai tsabta
- Kalmar serous wadda ta samo asali a matsayin bayanin ruwan cyst ya zo da bayanin irin nau'in kwayar halitta na epithelial da aka gani a cikin wadannan ciwace-ciwace.
- na iya haɗawa da saman ovary
- Ana tabbatar da rarrabuwa tsakanin benign, iyaka, da m ta hanyar tantancewa:
- cellular atypia (ko sel guda ɗaya ba su da kyau)
- mamayewa na kewayen stroma na ovarian (ko sel suna kutsawa kewayen nama)
- Ciwon daji na iyaka yana iya samun atypia ta salula amma ba su da shaidar mamayewa
- kasancewar jikin psammoma wani yanayi ne na ganowar cystadenocarcinomas[15]
Hasashen
[gyara sashe | gyara masomin]Hasashen ƙwayar ƙwayar cuta, kamar yawancin neoplasms, ya dogara da
- mataki na bambanci
- wannan shine yadda ƙwayoyin tumor suka yi kama da ƙananan ƙwayoyin cuta
- kumburin da ya bambanta da kyau yayi kama da ciwace-ciwacen daji
- ƙwayar cuta mara kyau ba zata iya kama da nau'in tantanin halitta kwata-kwata ba
- Ciwon daji mai matsakaicin matsakaici yakan yi kama da nau'in tantanin halitta, amma ya bayyana a fili.
- tsawo na ƙari zuwa wasu sifofi
- musamman tare da m malignancies, kasancewar m yada zuwa ga peritoneum yana da muhimmanci game da tsinkaya.
Adadin rayuwa na shekaru biyar na ciwace-ciwacen kan iyaka da muggan ciwace- ciwacen da ke tsare a cikin ovaries sune 100% da 70% bi da bi. Idan peritoneum yana da hannu, waɗannan ƙimar sun zama 90% da 25%.
Yayin da shekarun rayuwa na shekaru 5 na ciwace-ciwacen kan iyaka suna da kyau, bai kamata a ga wannan a matsayin shaida na magani ba, saboda sake dawowa zai iya faruwa shekaru da yawa bayan haka.
Mucinous ciwace-ciwacen daji
[gyara sashe | gyara masomin]
Ciwon daji na mucinous :
- Yi kama da takwarorinsu masu kama da juna amma da wuya su kasance na bangarorin biyu
- Da ɗan ƙasa na kowa, yana lissafin kusan kashi 25% na duk neoplasms na ovarian
- A wasu lokuta, ciwace-ciwacen daji na mucinous suna da alaƙa da ƙarin cysts masu girma dabam da ƙarancin sa hannu idan aka kwatanta da ciwace-ciwacen daji.
- Hakanan idan aka kwatanta da ciwace-ciwacen ciwace-ciwacen daji, ciwace-ciwacen mucinous ba su da yawa akai-akai, kusan kashi 5% na ciwace-ciwacen mucinous na farko na biyu ne.
- Zai iya haifar da manyan ƙwayoyin cystic, tare da rikodin nauyi sama da 25 kg
Pathology
[gyara sashe | gyara masomin]Ciwace-ciwacen ciwace-ciwacen daji suna da alaƙa da rufin sel masu tsayi na columnar tare da apical mucin da rashin cilia, kama da bayyanarsa tare da ƙananan mahaifa ko epithelia na hanji. Siffar na iya kama da ciwon daji ko ciwon daji na ovarian, amma yawanci ya samo asali ne daga appendix (duba mucinous adenocarcinoma tare da yanayin asibiti Pseudomyxoma peritonei ). Ana amfani da mamayewar stromal bayyananne don bambance ciwace-ciwacen kan iyaka da ciwace-ciwacen daji.
Hasashen
[gyara sashe | gyara masomin]Yawan rayuwa na shekaru 10 don ciwace-ciwacen kan iyaka da ke ƙunshe a cikin ovary, ƙwayar cuta mara kyau ba tare da mamayewa ba, da ciwace-ciwacen ƙwayar cuta masu haɗari sun fi 95%, 90%, da 66% bi da bi. Wani yanayin da ba kasafai ba amma abin lura da ke da alaƙa da mucinous ovarian neoplasms shine pseudomyxoma peritonei . Kamar yadda ciwace-ciwacen mucinous na ovarian na farko yawanci ba su da alaƙa (a cikin kwai ɗaya), gabatar da ciwace-ciwacen ƙwayoyin cuta na biyu yana buƙatar keɓance asalin wanda ba na ovarian ba, yawanci ƙari.
Ciwon daji na endometrioid
[gyara sashe | gyara masomin]Ciwon daji na endometrioid yana da kusan kashi 20% na duk cututtukan daji na ovarian kuma galibi suna da muni (carcinomas endometrioid). An yi su da glandan tubular masu kama da kamanni ko m endometrium. 15-30% na ciwon daji na endometrioid yana faruwa a cikin mutane masu ciwon daji na endometrium, kuma waɗannan marasa lafiya suna da kyakkyawan ganewa. Suna bayyana kama da sauran ciwace-ciwacen daji na epithelial-stromal, tare da wurare masu ƙarfi da cystic. Kashi 40% na waɗannan ciwace-ciwace suna da alaƙa da juna, lokacin da bangarorin biyu, metastases galibi suna nan.
Pathology
[gyara sashe | gyara masomin]- Glandan da ke da kamanceceniya da nau'in glandon endometrial
- Ciwace-ciwacen ciwace-ciwace suna da glandan da suka balaga da suka bayyana a cikin stroma fibrous
- Ciwon daji na kan iyaka yana da hadaddun tsarin reshe ba tare da mamayewar stromal ba
- Carcinomas (mummunan ciwace-ciwacen ciwace-ciwacen ciwace-ciwacen daji) suna da glandon da ke mamayewa tare da cunkoson sel, ƙwayoyin cuta, mitoses akai-akai. Tare da mafi ƙarancin bambance-bambance, ƙari ya zama mai ƙarfi.
Hasashen
[gyara sashe | gyara masomin]Hasashen sake yana dogara ne akan yaduwar ƙwayar cuta, da kuma yadda bambance-bambancen ciwon ya bayyana. Hasashen gabaɗaya ya ɗan fi muni fiye da ciwace-ciwacen daji ko mucinous, kuma adadin rayuwa na shekaru 5 ga marasa lafiya da ciwace-ciwacen da ke cikin ovary kusan 75%.
Share ciwace-ciwacen ƙwayoyin cuta
[gyara sashe | gyara masomin]
Bayyanannun ciwace-ciwacen ƙwayoyin cuta suna da manyan sel epithelial tare da ɗimbin fayyace cytoplasm kuma ana iya gani tare da haɗin gwiwa tare da endometriosis ko ciwon daji na endometrioid na ovary, yana da kama da share carcinoma cell na endometrium. Suna iya zama mai ƙarfi ko cystic. Idan daskararru, sel bayyanannun sun kasance ana shirya su cikin zanen gado ko tubules. A cikin nau'in cystic, ƙwayoyin neoplastic suna yin rufin cyst.
Hasashen
[gyara sashe | gyara masomin]Wadannan ciwace-ciwacen daji sun kasance masu tayar da hankali, tsawon shekaru biyar na rayuwa don ciwace-ciwacen da ke cikin ovaries kusan 65%. Idan ciwace-ciwacen ya yadu fiye da ovary a ganewar asali, tsinkayen ba shi da kyau
Brenner ciwon daji
[gyara sashe | gyara masomin]
Ciwon daji na Brenner su ne ciwace-ciwacen kwayoyin halitta-epithelial stromal cell ciwace-ciwacen daji wanda kwayar epithelial (wanda ke bayyana wadannan ciwace-ciwacen daji) wani tantanin halitta ne na wucin gadi. Waɗannan suna kama da kamannin epithelia na mafitsara. Ciwon daji na iya zama ƙanana zuwa manya sosai, kuma yana iya zama da ƙarfi ko cystic. A ilimin tarihi, kumburin ya ƙunshi ƙuƙuka na sel na tsaka-tsakin da aka ambata a baya a cikin nama da ke kewaye da su wanda yayi kama da kwai na yau da kullun. Ciwon daji na Brenner na iya zama mara kyau ko mara kyau, dangane da ko ƙwayoyin tumor sun mamaye nama da ke kewaye.
Ƙananan ciwace-ciwacen ƙwayoyin cuta
[gyara sashe | gyara masomin]Kananan ciwon daji na kwai (SCCO) Archived 2019-02-14 at the Wayback Machine gabaɗaya ana rarraba su cikin ciwace-ciwacen epithelial [16] masu alaƙa da keɓantattun siffofi na endocrin.[17]
Hukumar Lafiya ta Duniya (WHO) ta amince da SCCO a matsayin nau'ikan nau'ikan nau'ikan nau'in huhu guda biyu: Small Cell Ovarian Cancer of Hypercalcemic Type (SCCOHT) Archived 2019-02-14 at the Wayback Machine da Small Cell Ovarian Cancer of Pulmonary Type (SCCOPT). [17]
Ƙananan ciwace-ciwacen ƙwayoyin cuta ba safai ba ne kuma masu tayar da hankali, suna ba da gudummawa ga kasa da 2% na duk cututtukan gynecologic.[17] Matsakaicin shekarun ganewar asali shine shekaru 24, kuma yawancin marasa lafiya kuma suna da hypercalcemia (62%).[18] Yawanci yana kasancewa tare da babban ƙari ɗaya ɗaya.[18] Yawancin mata suna mutuwa a cikin shekara guda da ganewar asali.[18]
Magani
[gyara sashe | gyara masomin]Don ƙarin bayani na gaba ɗaya, duba ciwon daji na ovarian .
Bincike ya nuna cewa a layin farko na maganin Ciwon daji na Ovarian Ovarian (EOC), Pegylated Liposomal Doxorubicin tare da Carboplatin wani zaɓi mai gamsarwa ga Paclitaxel tare da Carboplatin.[19] A cikin mutanen da ke da EOC mai saurin dawowa, bincike ya gano cewa Pegylated Liposomal Doxorubicin tare da Carboplatin shine mafi kyawun magani fiye da Paclitaxel tare da Carboplatin.[20]
Don ci-gaban ciwon daji na wannan tarihin tarihi, Cibiyar Ciwon daji ta Amurka ta ba da shawarar hanyar chemotherapy wanda ya haɗu da intravenous gudanarwa (IV) da intraperitoneal (IP).[21] Abubuwan da aka fi so na chemotherapeutic sun haɗa da maganin platinum tare da haraji .
Metastases
[gyara sashe | gyara masomin]Don ciwace-ciwacen daji na epithelial-stromal, wuraren da aka fi sani da metastasis sune kogon pleural (33%), hanta (26%), da huhu (3%).[22]
Tasiri akan haihuwa
[gyara sashe | gyara masomin]Haihuwa bayan jiyya na ciwace-ciwacen daji na epithelial-stromal ya dogara ne akan ilimin tarihi da matakin farko don raba shi zuwa farkon kan iyaka (ko fiye da mara kyau) tare da matakan ci gaba na kan iyaka (ko mafi muni).[23] Gudanar da ra'ayin mazan jiya (ba tare da oophorectomy na biyu ba) na farkon matakan ciwace-ciwacen kan iyaka an kiyasta cewa zai haifar da damar sama da 50% na ciki na kwatsam tare da ƙarancin haɗarin sake dawowar ƙwayar cuta (0.5%).[23] A gefe guda kuma, a lokuta masu ra'ayin mazan jiya a cikin ciwace-ciwacen ciwace-ciwacen ciwace-ciwacen daji, an kiyasta yawan masu juna biyu da aka yi ba zato ba tsammani ya kai kashi 35 cikin ɗari kuma haɗarin sake dawowa mai mutuwa 2%.[23]
Manazarta
[gyara sashe | gyara masomin]- ↑ 1.0 1.1 Kosary CL (2007). "Chapter 16: Cancers of the Ovary" (PDF). In Baguio RN, Young JL, Keel GE, Eisner MP, Lin YD, Horner MJ (eds.). SEER Survival Monograph: Cancer Survival Among Adults: US SEER Program, 1988-2001, Patient and Tumor Characteristics. SEER Program. NIH Pub. No. 07-6215. Bethesda, MD: National Cancer Institute. pp. 133–144.
- ↑ Centers for Disease Control and Prevention, CDC WONDER. United States and Puerto Rico cancer statistics, 1999–2013 inci- dence incidence request.Available at: http://wonder.cdc.gov/ cancer-v2013.html. Retrieved December 1, 2016.
- ↑ Kashima K, Yahata T, Fujita K, Tanaka K. Outcomes of fertility-sparing surgery for women of reproductive age with FIGO stage IC epithelial ovarian cancer. Int J Gynaecol Obstet 2013;121:53–5.
- ↑ Rauh-Hain JA, Foley O, Winograd D, Andrade C, Clark RM, Vargas RJ, et al. Clinical characteristics and outcomes of pa- tients with stage I epithelial ovarian cancer compared to fallo- pian tube cancer. Am J Obstet Gynecol 2015;212:600.e1–8.
- ↑ Wright JD, Shah M, Mathew L, Burke WM, Culhane J, Gold- man N, et al. Fertility preservation in young women with epi- thelial ovarian cancer. Cancer 2009;115:4118–26.
- ↑ Melamed A., Rizzo A.E., Nitecki R., et al All-cause mortality after fertility-sparing surgery for stage i epithelial ovarian cancer. Obstet. Gynecol.. 2017;130(1):71-79. doi:10.1097/AOG.0000000000002102
- ↑ Bradshaw KD, Schorge JO, Schaffer J, Lisa M H, Hoffman BG (2008). Williams' Gynecology. McGraw-Hill Professional. ISBN 978-0-07-147257-9.
- ↑ Smedley H, Sikora K. Age as a prognostic factor in epithelial ovarian carcinoma. Br J Obstet Gynaecol 2016;92:839–42.
- ↑ Ghezzi F, Cromi A, Fanfani F, Malzoni M, Ditto A, De Iaco P, et al. Laparoscopic fertility-sparing surgery for early ovarian epithelial cancer: a multi-institutional experience. Gynecol On- col 2016;141:461–5.
- ↑ Melamed A, Keating NL, Clemmer JT, Bregar AJ, Wright JD, Boruta DM, et al. Laparoscopic staging for apparent stage I epithelial ovarian cancer. Am J Obstet Gynecol 2017;216:50. e1–50.e12.
- ↑ Kashima K, Yahata T, Fujita K, Tanaka K. Outcomes of fertility-sparing surgery for women of reproductive age with FIGO stage IC epithelial ovarian cancer. Int J Gynaecol Obstet 2013;121:53–5.
- ↑ Melamed A., Rizzo A.E., Nitecki R., et al All-cause mortality after fertility-sparing surgery for stage i epithelial ovarian cancer. Obstet. Gynecol.. 2017;130(1):71-79. doi:10.1097/AOG.0000000000002102
- ↑ - Vaidya, SA; Kc, S; Sharma, P; Vaidya, S (2014). "Spectrum of ovarian tumors in a referral hospital in Nepal". Journal of Pathology of Nepal. 4 (7): 539–543. doi:10.3126/jpn.v4i7.10295. ISSN 2091-0908. - Minor adjustment for mature cystic teratomas (0.17 to 2% risk of ovarian cancer): Mandal, Shramana; Badhe, Bhawana A. (2012). "Malignant Transformation in a Mature Teratoma with Metastatic Deposits in the Omentum: A Case Report". Case Reports in Pathology. 2012: 1–3. doi:10.1155/2012/568062. ISSN 2090-6781. PMC 3469088. PMID 23082264.
- ↑ 14.0 14.1 Baradwan, Saeed; Alalyani, Haneen; Baradwan, Amira; Baradwan, Afnan; Al-Ghamdi, Maram; Alnemari, Jameel; Al-Jaroudi, Dania (2018). "Bilateral ovarian masses with different histopathology in each ovary". Clinical Case Reports. 6 (5): 784–787. doi:10.1002/ccr3.1466. ISSN 2050-0904. PMC 5930217. PMID 29744056.- Creative Commons Attribution 4.0 International (CC BY 4.0) license
- ↑ Cotran RS, Kumar V, Nelson F, Robbins SL, Abbas AK (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. ISBN 978-0-7216-0187-8.
- ↑ Atlas of Genetics and Cytogenetics in Oncology and Haematology - Ovary: Epithelial tumors. Retrieved June 2014. By Lee-Jones, L. Atlas Genet Cytogenet Oncol Haematol. 2004;8(2):115-133.
- ↑ 17.0 17.1 17.2 Kaphan AA, Castro CM (2014-01-01). MPH rG, FRCPATH RH, MD JO, MD MJ (eds.). Small Cell and Neuroendocrine Cancers of the Ovary (in Turanci). John Wiley & Sons, Ltd. pp. 139–147. doi:10.1002/9781118655344.ch12. ISBN 9781118655344.
- ↑ 18.0 18.1 18.2 Bakhru A, Liu JR, Lagstein A (2012). "A case of small cell carcinoma of the ovary hypercalcemic variant in a teenager". Gynecologic Oncology Case Reports. 2 (4): 139–42. doi:10.1016/j.gynor.2012.09.001. PMC 3861231. PMID 24371647.
- ↑ Lawrie TA, Rabbie R, Thoma C, Morrison J, et al. (The Cochrane Collaboration) (October 2013). Lawrie TA (ed.). "Pegylated liposomal doxorubicin for first-line treatment of epithelial ovarian cancer". The Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd (10): CD010482. doi:10.1002/14651858.cd010482.pub2. PMC 6457824. PMID 24142521.
- ↑ Lawrie TA, Bryant A, Cameron A, Gray E, Morrison J (July 2013). "Pegylated liposomal doxorubicin for relapsed epithelial ovarian cancer". The Cochrane Database of Systematic Reviews (7): CD006910. doi:10.1002/14651858.cd006910.pub2. PMC 6457816. PMID 23835762.
- ↑ "NCI Issues Clinical Announcement for Preferred Method of Treatment for Advanced Ovarian Cancer". National Cancer Institute. January 2006. Archived from the original on 13 January 2009.
- ↑ Kolomainen DF, Larkin JM, Badran M, A'Hern RP, King DM, Fisher C, et al. (February 2002). "Epithelial ovarian cancer metastasizing to the brain: a late manifestation of the disease with an increasing incidence". Journal of Clinical Oncology. 20 (4): 982–6. doi:10.1200/JCO.2002.20.4.982. PMID 11844820.
- ↑ 23.0 23.1 23.2 Daraï E, Fauvet R, Uzan C, Gouy S, Duvillard P, Morice P (2012). "Fertility and borderline ovarian tumor: a systematic review of conservative management, risk of recurrence and alternative options". Human Reproduction Update. 19 (2): 151–66. doi:10.1093/humupd/dms047. PMID 23242913.
