Ciwon Daji Na Ovarian
| Ciwon Daji Na Ovarian | |
|---|---|
 | |
| Description (en) | |
| Iri |
female reproductive organ cancer (en) cuta |
| Specialty (en) | oncology |
| Genetic association (en) |
BRIP1 (en) |
| Medical treatment (en) | |
| Magani |
uracil mustard (en) |
| Identifier (en) | |
| ICD-10-CM | C56 |
| ICD-9-CM | 183.0 |
| ICD-O: | VARIED |
| OMIM | 167000 da 607893 |
| DiseasesDB | 9418 |
| MedlinePlus | 000889 |
| eMedicine | 000889 |
| Disease Ontology ID | DOID:2394 |
Ciwon daji na Ovarian ciwon daji ne wanda ke samuwa a ciki ko akan kwai .[1][2] Yana haifar da ƙananan ƙwayoyin cuta waɗanda ke da ikon mamayewa ko yada zuwa wasu sassan jiki.[3] Lokacin da wannan tsari ya fara, ba za a iya samun bayyanar cututtuka ba ko kawai.[4] Alamun suna zama ana gani yayin da ciwon daji ke ci gaba.[5][6] Wadannan bayyanar cututtuka na iya haɗawa da kumburi, zafi na pelvic, kumburi na ciki, maƙarƙashiya, da asarar ci, da sauransu.[7] Wuraren gama gari waɗanda ciwon daji zai iya yaɗuwa sun haɗa da rufin ciki, ƙwayoyin lymph, huhu, da hanta .[8]
Hadarin ciwon daji na kwai yana karuwa a cikin matan da suka fi yin kwai a tsawon rayuwarsu. Wannan ya kuma haɗa da waɗanda ba su taɓa haihuwa ba, waɗanda suka fara ovulation tun suna ƙanana da waɗanda suka kai ga al'ada tun lokacin da suka tsufa.[7] Sauran abubuwan haɗari sun haɗa da maganin hormone bayan menopause, maganin haihuwa, da kuma kiba [9][1] Abubuwan da ke rage haɗari sun haɗa da maganin hana haihuwa na hormonal, ƙwayar tubal, da shayarwa .[9] Kimanin kashi 10% na lokuta suna da alaƙa da haɗarin gadon gado; Mata masu maye gurbi a cikin kwayoyin halitta BRCA1 ko BRCA2 suna da kusan kashi 50% na damar kamuwa da cutar.[7] Ciwon daji na Ovarian shine nau'in ciwon daji na ovarian da aka fi sani, wanda ya ƙunshi fiye da kashi 95% na lokuta.[7] Akwai manyan nau'o'in nau'in ciwon daji na ovarian guda biyar, waɗanda carcinoma mai girma mai daraja (HGSC) ya fi yawa.[7] Wadannan ciwace-ciwacen ovarian an yi imanin suna farawa a cikin sel da ke rufe kwai, [10] ko da yake wasu na iya samuwa a cikin tubes na Fallopian . [11] Mafi qarancin nau'ikan ciwon daji na kwai sun haɗa da ciwace-ciwacen ƙwayoyin cuta[7] da ciwace-ciwacen jima'i . Ana tabbatar da ganewar cutar kansar kwai ta hanyar biopsy na nama, yawanci ana cirewa yayin tiyata. [4]
Ba a ba da shawarar dubawa a cikin matan da ke cikin matsakaicin haɗari ba, kamar yadda shaida ba ta goyi bayan raguwar mutuwa ba kuma yawan adadin gwaje-gwajen ƙarya na iya haifar da tiyata maras buƙata, wanda ke tare da haɗarinsa. Wadanda ke cikin hatsarin gaske na iya cire ovaries a matsayin ma'aunin rigakafi. [12] Idan an kama shi kuma a bi da shi a farkon mataki, ciwon daji na ovarian sau da yawa ana iya warkewa. [1] Jiyya yawanci ya haɗa da wasu haɗin tiyata, maganin radiation, da chemotherapy . [4] Sakamakon ya dogara da girman cutar, nau'in ciwon daji da ke da shi, da sauran yanayin kiwon lafiya.[7][13] Jimillar adadin tsira na shekaru biyar a Amurka shine kashi 49%.[14] Sakamakon ya fi muni a ƙasashe masu tasowa. [7]
A cikin 2012, sabbin maganganu sun faru a cikin kusan mata 239,000.[7] A cikin 2015 ya kasance a cikin mata miliyan 1.2 kuma ya haifar da mutuwar 161,100 a duniya.[15][16] A cikin mata shi ne na bakwai-mafi yawan kamuwa da cutar kansa kuma na takwas-mafi yawan sanadin mutuwar cutar kansa.[7] Yawan shekarun ganewar asali shine 63. Mutuwa daga ciwon daji na kwai ya fi yawa a Arewacin Amurka da Turai fiye da Afirka da Asiya. [7]
Alamomi da alamomi
[gyara sashe | gyara masomin]Alamun farko
[gyara sashe | gyara masomin]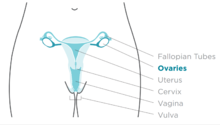
Alamun farko da alamun ciwon daji na kwai na iya zama ba a nan ko a hankali. A mafi yawan lokuta, alamun bayyanar suna wanzu na watanni da yawa kafin a gane su kuma a gano su .[17][18] Ana iya kuskuren bayyanar cututtuka kamar ciwon hanji mai fushi . [19] Matakin farko na ciwon daji na kwai yakan zama mara zafi. Alamun na iya bambanta dangane da nau'in ƙasa. [17] Ciwon daji na ovarian, wanda kuma aka sani da ƙananan ƙwayar cuta (LMP) ciwon daji na ovarian, ba sa karuwa a cikin matakan CA125 kuma ba a iya ganewa tare da duban dan tayi. Alamun alamun ciwon daji na LMP na iya haɗawa da kumburin ciki ko ciwon ƙashin ƙugu. Musamman manya-manyan talakawa sun kasance marasa kyau ko iyaka.[20][17]
Mafi yawan bayyanar cututtuka na ciwon daji na ovarian sun hada da kumburi, ciki ko pelvic zafi ko rashin jin daɗi, ciwon baya, rashin daidaituwa na al'ada ko kuma zubar da jini na al'ada postmenopausal, zafi ko zubar da jini bayan ko lokacin jima'i, asarar ci, gajiya, zawo, rashin narkewa, ƙwannafi, maƙarƙashiya . tashin zuciya, jin koshi, da yiwuwar bayyanar cututtuka na fitsari (ciki har da yawan fitsari da fitsarin gaggawa ).[18]
Daga baya alamomin
[gyara sashe | gyara masomin]Yawan girma na iya haifar da ciwo idan hargitsin kwai ya taso. Ana iya haifar da alamun ta hanyar matsi da yawa akan sauran gabobi na abdominopelvic ko daga metastases.[17][21][22] Idan waɗannan alamun sun fara faruwa sau da yawa ko mafi tsanani fiye da yadda aka saba, musamman bayan babu wani tarihin tarihi na irin wannan bayyanar cututtuka, ana la'akari da ciwon daji na ovarian.[20][17] Metastases na iya haifar da Sister Mary Joseph nodule .[22] Da wuya, teratomas na iya haifar da ci gaban teratoma ciwo ko peritoneal gliomatosis .[22] Wasu sun fuskanci menometrorrhagia da zubar da jini na al'ada na al'ada bayan menopause a mafi yawan lokuta. Sauran bayyanar cututtuka na yau da kullum sun hada da hirsutism, ciwon ciki, virilization, da kuma adnexal taro . [23]
Yara
[gyara sashe | gyara masomin]A cikin matasa ko yara masu ciwace-ciwacen ovarian, alamu na iya haɗawa da ciwon ciki mai tsanani, haushi na peritoneum, ko zubar jini . Alamun ciwon igiyar jima'i-stromal ciwace-ciwace suna samar da hormones waɗanda zasu iya shafar haɓaka halayen jima'i na biyu. Ciwon daji na jima'i-stromal a cikin yara masu tasowa na iya bayyana ta farkon balaga ; ciwon ciki da tashin hankali suma suna da yawa. Matasa masu ciwon ciwace-ciwacen jima'i na iya samun amenorrhea . Yayin da ciwon daji ke ƙara girma, yana iya haifar da tarin ruwa a cikin ciki. Idan ba a gano cutar ba ta lokacin da yake haifar da ascites, yawanci ana gano shi ba da daɗewa ba bayan haka.[17] Ciwon daji na ci gaba kuma na iya haifar da ƙwayar ciki, ƙwayar lymph nodes, ko zubar da jini .[22]
Abubuwan haɗari
[gyara sashe | gyara masomin]Ciwon daji na Ovarian yana da alaƙa da adadin lokacin da ake kashe kwai. Don haka, rashin haihuwa abu ne mai haɗari ga ciwon daji na ovarian, mai yiwuwa saboda an danne ovulation ta hanyar ciki. A lokacin ovulation, sel suna motsawa koyaushe don rarraba yayin da hawan ovulation ke ci gaba. Don haka, matan da ba su haihu ba suna fuskantar haɗarin cutar kansar kwai sau biyu fiye da waɗanda ke da. Tsawon lokacin ovulation wanda farkon hailar farko da marigayi menopause ke haifarwa shima abu ne mai haɗari.[20][24][25] Dukansu kiba da maganin maye gurbin hormone suma suna haɓaka haɗarin.[17]
Haɗarin kamuwa da ciwon daji na ovarian ya ragu ga matan da ke da ƙarancin hawan haila, babu hawan haila, shayarwa, shan maganin hana haihuwa, suna da ciki da yawa, kuma suna da ciki tun suna ƙanana. Haɗarin kamuwa da ciwon daji na kwai yana raguwa a cikin matan da suka yi fama da tubal ligation (wanda aka fi sani da suna "tubun da aka ɗaure"), duka biyun an cire su, ko kuma hysterectomy (aikin da mahaifa, da kuma wani lokacin mahaifa, ake cirewa).[18] Shekaru kuma abu ne mai haɗari. [17][13]
Hormones
[gyara sashe | gyara masomin]Yin amfani da magungunan haihuwa na iya taimakawa ga samuwar ƙwayar ƙwayar cuta ta ovarian, amma alaƙar da ke tsakanin su biyu tana da sabani kuma tana da wuyar yin nazari. Magungunan haihuwa na iya haɗawa da haɗarin ciwace-ciwacen kan iyaka. Wadanda aka yi wa jinyar rashin haihuwa amma sun kasance marasa amfani suna cikin haɗari mafi girma ga ciwon daji na ovarian epithelial; duk da haka, wadanda aka yi nasarar yi musu maganin rashin haihuwa kuma daga baya suka haihu ba su da wani hadari. Wannan na iya zama saboda zubar da ƙwayoyin da ke da riga-kafi a lokacin daukar ciki, amma har yanzu ba a san dalilin ba.[20] Matsalolin haɗari na iya zama rashin haihuwa da kanta, ba magani ba.[24]
Yanayin hormone kamar ciwon ovary polycystic da endometriosis suna da alaƙa da ciwon daji na ovarian, amma ba a tabbatar da haɗin gwiwa gaba ɗaya ba.[19] Maganin maye gurbin hormone na postmenopausal (HRT) tare da isrogen yana iya ƙara haɗarin ciwon daji na ovarian. Ba a tabbatar da ƙungiyar ba a cikin wani babban bincike,[20][26] amma sanannun binciken ciki har da Nazarin Mata Miliyan sun goyi bayan wannan haɗin gwiwa. Postmenopausal HRT tare da haɗin estrogen da progesterone na iya ƙara haɗarin zamani idan aka yi amfani da shi sama da shekaru 5, amma wannan haɗarin ya dawo al'ada bayan an daina jinya.[24] Estrogen HRT tare da ko ba tare da progestins yana ƙara haɗarin endometrioid da ciwace-ciwacen daji ba amma yana rage haɗarin ciwace-ciwacen mucinous. Yawan adadin isrogen yana haɓaka wannan haɗarin.[22] Endometriosis wani abu ne mai haɗari ga ciwon daji na ovarian,[24] kamar yadda yake jin zafi tare da haila. Endometriosis yana da alaƙa da bayyanannun tantanin halitta da ƙananan nau'ikan endometrioid, ƙananan ciwace-ciwacen ƙwayar cuta, ciwace-ciwacen mataki na I da II, ciwace-ciwacen sa na 1, da ƙananan mace-mace.[22]
Kafin al'ada, kiba na iya ƙara haɗarin kamuwa da ciwon daji na ovarian, amma wannan haɗarin ba ya samuwa bayan al'ada. Wannan haɗarin kuma yana da alaƙa ga waɗanda ke da kiba kuma ba su taɓa amfani da HRT ba. Irin wannan haɗin gwiwa tare da ciwon daji na ovarian yana bayyana a cikin mata masu tsayi.[24]
Genetics
[gyara sashe | gyara masomin]
Tarihin iyali na ciwon daji na ovarian abu ne mai haɗari ga ciwon daji na ovarian. Mata masu ciwon daji marasa polyposis na gado (Lynch Syndrome), da waɗanda ke da BRCA-1 da BRCA-2 suna cikin haɗarin haɗari.
Babban haɗarin kwayoyin halitta don ciwon daji na ovarian shine maye gurbi a cikin kwayoyin halittar BRCA1 ko BRCA2, ko a cikin kwayoyin gyara rashin daidaituwa na DNA, wanda ke cikin kashi 10% na cututtukan daji na ovarian. Allele guda ɗaya kawai ake buƙatar mutated don sanya mutum cikin haɗari mai girma. Za a iya gadon kwayar halittar ta hanyar layin uwa ko na uba, amma yana da matsananciyar shiga .[17][20] Ko da yake maye gurbi a cikin waɗannan kwayoyin halitta yawanci yana da alaƙa da haɓakar cutar kansar nono, suna kuma ɗaukar haɗarin ciwon daji na ovarian na rayuwa, haɗarin da ke kai kololuwa a cikin 40s da 50s. Mafi ƙarancin haɗarin da aka ambata shine 30% kuma mafi girman 60%.[17][19][20] Maye gurbi a cikin BRCA1 suna da haɗarin rayuwa na haɓaka ciwon daji na ovarian na 15-45%.[22] Maye gurbi a cikin BRCA2 ba su da haɗari fiye da waɗanda ke tare da BRCA1, tare da haɗarin rayuwa na 10% (mafi ƙarancin haɗari) zuwa 40% (mafi girman haɗari da aka ambata).[17][22] A matsakaita, cututtukan daji masu alaƙa da BRCA suna tasowa shekaru 15 kafin takwarorinsu na lokaci-lokaci saboda mutanen da suka gaji maye gurbi a kwafin kwayar halittarsu guda ɗaya kawai suna buƙatar maye gurbinsu don fara aiwatar da cutar sankara, yayin da mutanen da ke da kwayoyin halitta guda biyu na al'ada zasu buƙaci samun maye gurbi biyu.[20]
A Amurka, biyar daga cikin 100 mata masu dan uwan digiri na farko masu ciwon daji na kwai daga ƙarshe za su sami kansar kwai da kansu, wanda ke sanya waɗanda ke da dangin da abin ya shafa cikin haɗarin matan da ba su da lafiya. Bakwai daga cikin 100 mata masu dangi biyu ko fiye da ciwon daji na kwai za su sami kansar kwai.[20][27] Gabaɗaya, 5-10% na cututtukan daji na ovarian suna da sanadin kwayoyin halitta.[20] Maye gurbi na BRCA yana da alaƙa da babban matakin serous mara cin nama na ciwon daji na kwai.[22]
Ƙarfafa tarihin iyali na ciwon daji na endometrial, ciwon daji na hanji, ko wasu cututtuka na gastrointestinal na iya nuna kasancewar ciwon da aka sani da ciwon daji na nonpolyposis colorectal cancer (wanda kuma aka sani da Lynch syndrome), wanda ke ba da haɗari mafi girma don bunkasa yawan ciwon daji, ciki har da ovarian. ciwon daji. Ciwon daji na Lynch yana haifar da maye gurbi a cikin ƙwayoyin gyare-gyaren rashin daidaituwa, ciki har da MSH2, MLH1, MLH6, PMS1, da PMS2 .[17] Hadarin ciwon daji na ovarian ga mutumin da ke da cutar Lynch yana tsakanin kashi 10 zuwa 12.[17] Matan zuriyar Icelandic, zuriyar Yahudawa Yahudawa / Ashkenazi zuriyar Yahudawa, da zuriyar Hungarian suna cikin haɗari mafi girma ga ciwon daji na ovarian epithelial.[20] Estrogen receptor beta gene ( ESR2 ) alama ya zama mabuɗin don pathogenesis da amsawa ga farfadowa.[28] Sauran kwayoyin halittar da aka danganta da ciwon daji na ovarian sune BRIP1, MSH6, RAD51C da RAD51D .[29] CDH1, CHEK2, PALB2 da RAD50 kuma an danganta su da ciwon daji na ovarian.[30]
Cututtukan ƙwayoyin cuta da ba kasafai da yawa suna da alaƙa da takamaiman nau'ikan ciwon daji na kwai. Peutz-Jeghers ciwo, cuta ce mai wuyar gaske, kuma tana sa mata su kamu da cutar ta hanyar jima'i tare da tubules na annular .[17][19] Cutar Ollier da Ciwon Maffucci suna da alaƙa da ciwace-ciwacen ƙwayoyin cuta na granulosa a cikin yara kuma ana iya haɗa su da ciwace-ciwacen Sertoli-Leydig. Benign fibromas suna hade da ciwon basal cell carcinoma nevoid .[17]
Abinci
[gyara sashe | gyara masomin]Shaye-shaye ba ya da alaƙa da ciwon daji na kwai.[22][31]
Ƙungiyar Ciwon daji ta Amirka ta ba da shawarar tsarin cin abinci mai kyau wanda ya haɗa da yalwar 'ya'yan itatuwa, kayan lambu, dukan hatsi, da kuma abincin da ke kaucewa ko iyakance ja da nama da aka sarrafa da kuma sarrafa sukari. [32] Yawan amfani da jimillar jimillar kitse da kitsen mai yana kara haɗarin ciwon daji na kwai. [33] Wani bita na laima na 2021 ya gano cewa kofi, kwai, da cin mai yana ƙara haɗarin cutar kansar kwai.[34] Akwai gaurayawan shaida daga bincike kan hadarin kansar kwai da kuma amfani da kayan kiwo .[35][36]
Abubuwan muhalli
[gyara sashe | gyara masomin]Kasashe masu ci gaban masana'antu, ban da Japan, suna da yawan ciwon daji na ovarian na epithelial, wanda zai iya kasancewa saboda abinci a waɗannan ƙasashe. Matan farar fata suna cikin 30-40% mafi girman haɗari ga ciwon daji na ovarian idan aka kwatanta da matan Black da matan Hispanic, mai yiwuwa saboda dalilai na zamantakewa; Mata farare suna da karancin yara da nau'ikan aikin tiyata na gynecology daban-daban waɗanda ke shafar haɗarin kansar kwai.[20]
Shaidu na yau da kullun sun nuna cewa talc, magungunan kashe qwari, da magungunan ciyawa suna ƙara haɗarin ciwon daji na ovarian.[37] Cibiyar Cancer ta Amurka ta lura cewa, ya zuwa yanzu, babu wani bincike da ya iya danganta duk wani sinadari guda daya a cikin muhalli, ko kuma a cikin abincin dan Adam, kai tsaye ga maye gurbi da ke haifar da ciwon daji na kwai. [38]
Sauran
[gyara sashe | gyara masomin]Sauran abubuwan da aka bincika, irin su shan taba, ƙananan matakan bitamin D a cikin jini, kasancewar shigar da cysts na ovarian, da kamuwa da kwayar cutar papilloma na mutum (dalilin wasu lokuta na ciwon daji na mahaifa), an musanta su a matsayin abubuwan haɗari. ciwon daji na kwai. Ciwon daji na perineal talc yana da rigima, saboda yana iya zama mai ban sha'awa idan yana tafiya ta hanyar haihuwa zuwa ovaries. Nazarin kula da shari'ar ya nuna cewa amfani da perineal talc yana ƙara haɗarin ciwon daji na ovarian, amma yin amfani da talc sau da yawa ba ya haifar da haɗari mafi girma. Amfani da talc a wani wuri a jiki baya da alaƙa da ciwon daji na kwai. Zauna akai-akai na tsawon lokaci yana da alaƙa da yawan mace-mace daga ciwon daji na ovarian epithelial. Ba a kawar da haɗarin ta hanyar motsa jiki na yau da kullum, kodayake an saukar da shi.
Ƙara yawan shekaru (har zuwa 70s) abu ne mai haɗari ga ciwon daji na ovarian epithelial saboda yawancin maye gurbi a cikin sel na iya tarawa kuma a ƙarshe ya haifar da ciwon daji. Wadanda suka haura 80 suna cikin dan karamin hadari.
Shan taba yana da alaƙa da haɗari mafi girma na ciwon daji na ovarian mucinous ; bayan daina shan taba, haɗarin ƙarshe ya koma al'ada. Matsayi mafi girma na furotin C-reactive yana da alaƙa da haɗarin haɓakar ciwon daji na ovarian. [39]
Abubuwan kariya
[gyara sashe | gyara masomin]Rushewar ovulation, wanda in ba haka ba zai haifar da lalacewa ga epithelium na ovarian kuma, saboda haka, kumburi, yana da kariya gabaɗaya. Ana iya samun wannan tasiri ta hanyar samun yara, shan hadewar maganin hana haihuwa, da kuma ciyar da nono, duk waɗannan abubuwan kariya ne. Tsawon lokacin shayarwa yana da alaƙa da raguwa mai girma a cikin haɗarin ciwon daji na ovarian. Kowace haihuwa tana rage haɗarin ciwon daji na kwai, kuma ana ganin wannan tasirin tare da haihuwa har biyar. Haɗaɗɗen maganin hana haihuwa na baka yana rage haɗarin ciwon daji na ovarian har zuwa kashi 50%, kuma tasirin kariya na haɗe-haɗe na baka zai iya ɗaukar shekaru 25-30 bayan an daina su. Yin amfani da aspirin na yau da kullun ko acetaminophen (paracetamol) na iya haɗuwa da ƙananan haɗarin ciwon daji na ovarian; sauran NSAIDs ba su da irin wannan tasirin kariya.
Tubal ligation yana da kariya saboda carcinogens ba sa iya kaiwa ga ovary da fimbriae ta farji, mahaifa, da tubes na fallopian. Tubal ligation kuma yana da kariya ga mata masu maye gurbin BRCA1, amma ba maye gurbin BRCA2 ba. Hysterectomy yana rage haɗari, da kuma cire duka tubes na fallopian da ovaries ( salpingo-oophorectomy na biyu) yana rage haɗarin ba kawai ciwon daji na ovarian ba amma ciwon nono. Wannan har yanzu batu ne na bincike, kamar yadda haɗin kai tsakanin hysterectomy da ƙananan ciwon daji na ovarian yana da rikici. Dalilin da cewa hysterectomy na iya zama kariya ba a bayyana su ba kamar na 2015.
Abincin da ya haɗa da adadin carotene, fiber, da bitamin tare da ƙananan kitse-musamman, abinci tare da kayan lambu marasa sitaci (misali broccoli da albasa ) na iya zama kariya. Fiber na abinci yana da alaƙa da raguwar haɗarin ciwon daji na ovarian. Wani bita na 2021 ya gano cewa kayan lambu masu ganye, kayan lambu na allium, fiber, flavanoids da shan shayi na iya rage haɗarin cutar kansar kwai.
Pathophysiology
[gyara sashe | gyara masomin]| Gene mutated | Mutation type | Subtype | Prevalence |
|---|---|---|---|
| AKT1 | amplification | 3% | |
| AKT2 | amplification/mutation | 6%,[40] 20%[42] | |
| ARID1A | point mutation | endometrioid and clear cell | |
| BECN1 | deletion | ||
| BRAF | point mutation | low-grade serous | 0.5% |
| BRCA1 | nonsense mutation | high-grade serous | 5% |
| BRCA2 | frameshift mutation | high-grade serous | 3% |
| CCND1 | amplification | 4% | |
| CCND2 | upregulation | 15% | |
| CCNE1 | amplification | 20% | |
| CDK12 | high-grade serous | ||
| CDKN2A | downregulation (30%) and deletion (2%) | 32% | |
| CTNNB1 | clear cell | ||
| DICER1 | missense mutation (somatic) | nonepithelial | 29% |
| DYNLRB1 (km23) | mutation | 42% | |
| EGFR | amplification/overexpression | 20% | |
| ERBB2 (Her2/neu) | amplification/overexpression | mucinous and low-grade serous | 30% |
| FMS | coexpression with CSF-1 | 50% | |
| FOXL2 | point mutation (402 C to G) | adult granulosa cell | ~100% |
| JAG1 | amplification | 2% | |
| JAG2 | amplification | 3% | |
| KRAS | amplification | mucinous and low-grade serous | 11% |
| MAML1 | amplification and point mutation | 2% | |
| MAML2 | amplification and point mutation | 4% | |
| MAML3 | amplification | 2% | |
| MLH1 | 1% | ||
| NF1 | deletion (8%) and point mutation (4%) | high-grade serous | 12% |
| NOTCH3 | amplification and point mutation | 11% | |
| NRAS | low-grade serous | ||
| PIK3C3 (PI3K3) | amplification/mutation | 12–20% | |
| PIK3CA | amplification | endometrioid and clear cell | 18% |
| PPP2R1A | endometrioid and clear cell | ||
| PTEN | deletion | endometrioid and clear cell | 7% |
| RB1 | deletion (8%) and point mutation (2%) | 10% | |
| TGF-β | mutation/overexpression | 12% | |
| TP53 | mutation/overexpression | high-grade serous | 20–50% |
| TβRI | mutation | 33% | |
| TβRII | mutation | 25% | |
| USP36 | overexpression |
Ciwon daji na Ovarian yana samuwa lokacin da kurakurai a cikin ci gaban kwayoyin ovarian na al'ada ya faru. Yawancin lokaci, lokacin da sel suka tsufa ko suka lalace, suna mutuwa, kuma sabbin sel suna zama wurinsu. Ciwon daji yana farawa ne lokacin da sabbin sel suka yi ba tare da buƙata ba, kuma tsofaffi ko ƙwayoyin da suka lalace ba su mutu kamar yadda ya kamata. Ƙirƙirar ƙarin sel sau da yawa yakan haifar da tarin nama da ake kira ƙwayar ƙwayar ovarian ko girma. Wadannan kwayoyin cutar kansa marasa al'ada suna da nakasu na kwayoyin halitta da yawa wadanda ke sa su girma da yawa. Lokacin da ovary ya saki kwai, ƙwayar kwai ya buɗe kuma ya zama corpus luteum . Wannan tsarin yana buƙatar gyara ta hanyar rarraba sel a cikin kwai. Ci gaba da ovulation na dogon lokaci yana nufin ƙarin gyaran ovary ta hanyar rarraba kwayoyin halitta, wanda zai iya samun maye gurbi a kowane bangare.
Gabaɗaya, yawancin maye gurbi a cikin ciwon daji na ovarian yana faruwa a cikin NF1, BRCA1, BRCA2, da CDK12 . Nau'in I ciwon daji na ovarian, wanda ya kasance ba shi da karfi, yana da rashin zaman lafiya na microsatellite a cikin kwayoyin halitta da yawa, ciki har da duka oncogenes (mafi mahimmanci BRAF da KRAS ) da kuma ciwon daji (mafi mahimmanci PTEN ). Mafi yawan maye gurbi a cikin nau'in ciwon daji na Nau'in I sune KRAS, BRAF, ERBB2, PTEN, PIK3CA, da ARID1A. Nau'in ciwon daji na II, nau'in nau'i mai tsanani, suna da nau'i-nau'i daban-daban da suka canza, ciki har da p53, BRCA1, da BRCA2 . Ƙananan ciwon daji suna da maye gurbi a cikin KRAS, yayin da ciwon daji na kowane nau'i wanda ke tasowa daga ƙananan ƙwayoyin cuta masu haɗari suna da maye gurbi a cikin p53. Nau'in I na ciwon daji yakan tasowa daga raunuka na farko, yayin da Nau'in ciwon daji na II na iya tasowa daga ciwon daji na intraepithelial carcinoma . Ciwon daji masu rauni waɗanda ke da maye gurbi na BRCA suma babu makawa suna da maye gurbi na p53, wanda ke nuna cewa kawar da ƙwayoyin halittar aiki guda biyu yana da mahimmanci don haɓakar kansa.
A cikin kashi 50 cikin 100 na manyan cututtukan daji na serous, gyaran DNA na haɗin gwiwar haɗin gwiwa ba shi da aiki, kamar yadda manyan hanyoyin sigina da FOXM1 suke . Hakanan kusan koyaushe suna da maye gurbi na p53. Baya ga wannan, maye gurbi a cikin ƙwayar cutar sankara mai girma yana da wuyar ganewa fiye da babban matakin rashin kwanciyar hankali . BRCA1 da BRCA2 suna da mahimmanci don gyaran DNA na sake haɗe da juna, kuma ana samun maye gurbin ƙwayoyin cuta a cikin waɗannan kwayoyin halitta a kusan kashi 15% na mata masu ciwon daji na ovarian. Mafi yawan maye gurbi a cikin BRCA1 da BRCA2 sune sauye-sauyen sauye- sauyen da suka samo asali a cikin ƙaramin adadin Yahudawan Ashkenazi.
Kusan 100% na carcinomas na mucinous da ba kasafai suna da maye gurbi a cikin KRAS da haɓakawa na ERBB2 (wanda kuma aka sani da Her2/neu ). Gabaɗaya, 20% na ciwon daji na ovarian suna da maye gurbi a cikin Her2/neu .
Ciwon daji na iya tasowa daga serous tubal intraepithelial carcinoma, maimakon tasowa kwatsam daga naman kwai. Sauran carcinomas suna tasowa daga ƙwayoyin cuta na cortical inclusion cysts, waɗanda ƙungiyoyi ne na sel na ovarian epithelial a cikin stroma .
Bincike
[gyara sashe | gyara masomin]
jarrabawa
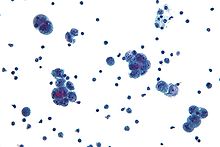
[gyara sashe | gyara masomin]Binciken ciwon daji na ovarian yana farawa tare da gwajin jiki (ciki har da jarrabawar pelvic ), gwajin jini (ga CA-125 da wasu lokuta wasu alamomi), da kuma duban dan tayi na transvaginal . Wani lokaci ana amfani da jarrabawar rectovaginal don taimakawa tsara aikin tiyata. Dole ne a tabbatar da ganewar asali tare da tiyata don duba kogon ciki, ɗaukar biopsies (samfurin nama don nazarin microscopic ), da kuma neman kwayoyin ciwon daji a cikin ruwan ciki. Wannan yana taimakawa wajen sanin ko adadin ovarian yana da kyau ko m.
Matakan farko na ciwon daji na Ovarian (I/II) suna da wuyar ganewa saboda yawancin alamun bayyanar cututtuka ba su da takamaiman kuma don haka ba su da amfani sosai wajen ganewar asali; a sakamakon haka, ba kasafai ake gano ta ba har sai ta yadu kuma ta ci gaba zuwa mataki na gaba (III/IV). Bugu da ƙari, alamun ciwon daji na ovarian na iya bayyana kama da ciwon hanji mai ban haushi . A cikin matan da ciki zai iya yiwuwa, ana iya auna matakin BHCG yayin tsarin ganewar asali. Serum alpha-fetoprotein, neuron-specific enolase, da kuma lactate dehydrogenase za a iya auna a cikin matasa 'yan mata da matasa da ake zargi da ciwon ciwace-ciwacen daji kamar yadda ƙananan mata masu ciwon daji na ovarian suna iya samun ciwon ƙwayar ƙwayar ƙwayar cuta.
Binciken jiki, ciki har da jarrabawar pelvic, da kuma duban dan tayi (transvaginal ko in ba haka ba) duka suna da mahimmanci don ganewar asali: jarrabawar jiki na iya nuna ƙarar girth na ciki da / ko ascites (ruwa a cikin rami na ciki), yayin da jarrabawar pelvic na iya bayyana wani ovarian. ko yawan ciki. Matsakaicin adnexal wani muhimmin bincike ne wanda sau da yawa yana nuna ciwon daji na ovarian, musamman ma idan an gyara shi, nodular, wanda ba daidai ba, mai ƙarfi, da/ko biyu. 13-21% na adnexal talakawa suna lalacewa ta hanyar malignancy; duk da haka, akwai wasu m dalilai na adnexal talakawa, ciki har da ovarian follicular cyst, leiomyoma, endometriosis, ectopic ciki, hydrosalpinx, tuboovarian abscess, ovarian torsion, dermoid cyst, cystadenoma (serous ko mucinous), diverticular ko appendice jijiya ciwon daji . koda pelvic, urethra ko mafitsara diverticulum, benign cystic mesothelioma na peritoneum, peritoneal tarin fuka, ko paraovarian cyst . Ovaries da za a iya ji su ma alama ce ta kansar kwai a cikin matan da suka shude. Sauran sassan gwajin jiki don zargin ciwon daji na ovarian na iya haɗawa da gwajin nono da jarrabawar duburar dijital . Palpation na supraclavicular, axillary, da inguinal lymph nodes na iya bayyana lymphadenopathy, wanda zai iya zama alamar metastasis. Wani mai nuna alama na iya kasancewa kasancewar kumburin pleural, wanda za'a iya lura dashi akan auscultation .
Lokacin da aka haɗa rashin lafiyar kwai a cikin jerin yuwuwar ganowa, ana nuna iyakataccen adadin gwaje-gwajen dakin gwaje-gwaje. Ana samun cikakken ƙididdigar jini da gwajin jini na electrolyte yawanci; lokacin da ciwon daji na ovarian ya kasance, waɗannan gwaje-gwajen suna nuna yawan adadin platelets (20-25% na marasa lafiya) da ƙananan matakan sodium na jini saboda siginar sinadarai da ƙwayar cuta ta ɓoye. Gwaji mai kyau na inhibin A da inhibin B na iya nuna ƙwayar ƙwayar ƙwayar ƙwayar cuta ta granulosa.
Gwajin jini don ƙwayar ƙwayar cuta mai suna CA-125 yana da amfani a cikin ganewar asali daban-daban da kuma bibiyar cutar, amma shi da kansa ba a nuna shi ya zama hanya mai mahimmanci don nunawa ga ciwon daji na ovarian na farko ba saboda rashin yarda da shi. hankali da kuma takamaiman. Matakan CA-125 a cikin matan da suka riga sun wuce 200 U / ml na iya nuna ciwon daji na ovarian, kamar yadda kowane girma a CA-125 sama da 35 U / mL a cikin mata bayan mazaopausal. Matakan CA-125 ba daidai ba ne a farkon matakin ciwon daji na ovarian, kamar yadda rabin mataki na masu ciwon daji na ovarian suna da matakin CA-125 na al'ada. CA-125 kuma za a iya haɓakawa a cikin yanayi mara kyau (marasa ciwon daji), ciki har da endometriosis, ciki, mahaifa fibroids, haila, ovarian cysts, tsarin lupus erythematosus, cututtuka na hanta, cututtuka na ƙwayar cuta, cututtuka na pelvic, da leiomyoma. HE4 wani ɗan takara ne don gwajin cutar kansar kwai, kodayake ba a gwada shi sosai ba. Sauran alamun ciwon daji na ciwon daji na ovarian sun hada da CA19-9, CA72-4, CA15-3, immunosuppressive acidic protein, haptoglobin-alpha, OVX1, mesothelin, lysophosphatidic acid, osteopontin, da fibroblast girma factor 23 .
Amfani da sassan gwajin jini na iya taimakawa wajen gano cutar. Ƙungiyar OVA1 ta ƙunshi CA-125, beta-2 microglobulin, transferrin, apolipoprotein A1, da transthyretin . OVA1 da ke sama da 5.0 a cikin matan da suka rigaya kafin haihuwa da 4.4 a cikin matan da suka shude suna nuna babban haɗarin ciwon daji. Ana amfani da saitin gwaje-gwaje daban-daban don gano ciwace-ciwacen jima'i-stromal. Babban matakan testosterone ko dehydroepiandrosterone sulfate, haɗe tare da sauran alamun bayyanar cututtuka da matakan inhibin A da inhibin B na iya zama alamar SCST na kowane nau'i.
Binciken na yanzu yana duba hanyoyin da za a yi la'akari da ƙwayoyin cuta masu alamar ƙari a hade tare da wasu alamun cututtuka (watau rediyo da/ko alamun cututtuka) don inganta daidaiton bincike. Kalubalen da ke cikin irin wannan tsarin shi ne yadda cutar sankarar mahaifa ke yaduwa yana nufin cewa ko da gwaji tare da kulawa mai zurfi da takamaiman aiki zai haifar da sakamako mai kyau na ƙarya, wanda hakan na iya haifar da al'amura kamar yin hanyoyin tiyata da kansa. ba a samun shi a ciki.[ana buƙatar hujja]Har yanzu ba a samar da hanyoyin nazarin halittu don ciwon daji .
An fi son yin sikanin CT don tantance girman ƙwayar ƙwayar cuta a cikin rami na ciki, kodayake ana iya amfani da hoton maganadisu . Binciken CT kuma yana iya zama da amfani don gano caking omental ko bambance ruwa daga ƙaƙƙarfan ƙari a cikin ciki, musamman a cikin ƙananan ciwace-ciwacen ƙwayar cuta. Koyaya, bazai iya gano ƙananan ciwace-ciwacen ƙwayoyi ba. Wani lokaci, ana amfani da x-ray na ƙirji don gano metastases a cikin ƙirji ko zubar da jini . Wani gwaji don cututtukan ƙwayar cuta, ko da yake ba a yi amfani da shi akai-akai ba, shine barium enema, wanda zai iya nuna idan ciwon rectosigmoid yana cikin cutar. Positron emission tomography, sikanin kashi, da paracentesis suna da iyakacin amfani; a gaskiya ma, paracentesis na iya haifar da metastases don samuwa a wurin saka allura kuma bazai samar da sakamako mai amfani ba. Duk da haka, ana iya amfani da paracentesis a lokuta inda babu ƙwayar pelvic kuma ascites yana nan. Likitan da ke zargin kansar kwai yana iya yin mammography ko biopsy na endometrial (a yanayin zubar jini mara kyau) don tantance yiwuwar cutar ƙirjin nono da ciwon daji na endometrial, bi da bi. Ultrasonography na farji sau da yawa shine binciken hoton layi na farko da aka yi lokacin da aka sami taro na adnexal. Yawancin halaye na yawan adadin adnexal suna nuna rashin lafiyar ovarian; yawanci suna da ƙarfi, marasa daidaituwa, masu yawa, da/ko babba; kuma yawanci suna da siffofi na papillary, tasoshin tsakiya, da/ko ɓarna na ciki marasa daidaituwa. Koyaya, SCST ba shi da takamaiman halaye akan binciken rediyo.
Don tantance ainihin ciwon daji na ovarian, ana buƙatar hanyar tiyata don duba ciki. Wannan na iya zama hanyar buɗewa ( laparotomy, incision ta bangon ciki ) ko tiyatar maɓalli ( laparoscopy ). A lokacin wannan hanya, ana cire nama da ake tuhuma kuma an aika da shi don nazarin microscopic . Yawancin lokaci, wannan ya haɗa da salpingo-oophorectomy ɗaya, cire kwai guda ɗaya da ya shafa da tube na fallopian. Hakanan za'a iya bincikar ruwa daga rami na ciki don ƙwayoyin kansa. Idan an sami ciwon daji, wannan hanya kuma za a iya amfani da ita don sanin iyakar yaduwarsa (wanda shine nau'i na ciwon daji ).
An nuna Pafolacianine don amfani a cikin manya da ciwon daji na ovarian don taimakawa wajen gano ciwon daji a lokacin tiyata. Wani ma'aikacin bincike ne wanda ake gudanarwa ta hanyar allurar cikin jijiya kafin a yi masa tiyata.
Hadari
[gyara sashe | gyara masomin]A widely recognized method of estimating the risk of malignant ovarian cancer is the risk of malignancy index (RMI), calculated based on an initial workup. An RMI score of over 200 or 250 is generally felt to indicate high risk for ovarian cancer.
Ana ƙididdige RMI kamar:
- RMI = makin duban dan tayi × maki menopause x matakin CA-125 a U/ml. [43]
- Ana iya amfani da hanyoyi guda biyu don tantance ƙimar duban dan tayi da maki menopause, tare da sakamakon sakamakon da ake kira RMI 1 da RMI 2, bi da bi, ya danganta da wace hanya ake amfani da ita.
Manazarta
[gyara sashe | gyara masomin]- ↑ 1.0 1.1 1.2 "Ovarian Cancer Prevention". NCI. December 6, 2013. Archived from the original on 6 July 2014. Retrieved 1 July 2014.
- ↑ Seiden, Michael (2015). "Gynecologic Malignancies, Chapter 117". MGraw-Hill Medical. Archived from the original on September 10, 2017. Retrieved June 24, 2017.
- ↑ "Defining Cancer". National Cancer Institute. 2007-09-17. Archived from the original on 25 June 2014. Retrieved 10 June 2014.
- ↑ 4.0 4.1 4.2 "Ovarian Epithelial Cancer Treatment". NCI. 2014-05-12. Archived from the original on 5 July 2014. Retrieved 1 July 2014.
- ↑ "Ovarian Epithelial Cancer Treatment". NCI. 2014-05-12. Archived from the original on 5 July 2014. Retrieved 1 July 2014.
- ↑ Ebell MH, Culp MB, Radke TJ (March 2016). "A Systematic Review of Symptoms for the Diagnosis of Ovarian Cancer". American Journal of Preventive Medicine. 50 (3): 384–394. doi:10.1016/j.amepre.2015.09.023. PMID 26541098.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 "Ovarian Epithelial Cancer Treatment". NCI. 2014-05-12. Archived from the original on 5 July 2014. Retrieved 1 July 2014.
- ↑ Ruddon RW (2007). Cancer Biology (4th ed.). Oxford: Oxford University Press. p. 223. ISBN 9780195175431. Archived from the original on 2015-09-15.
- ↑ 9.0 9.1 Ruddon RW (2007). Cancer Biology (4th ed.). Oxford: Oxford University Press. p. 223. ISBN 9780195175431. Archived from the original on 2015-09-15.
- ↑ Piek JM, van Diest PJ, Verheijen RH (2008). "Ovarian carcinogenesis: an alternative hypothesis". Ovarian Cancer. Adv. Exp. Med. Biol. Advances in Experimental Medicine and Biology. 622. pp. 79–87. doi:10.1007/978-0-387-68969-2_7. ISBN 978-0-387-68966-1. PMID 18546620.Samfuri:Closed access
- ↑ Maoz, Asaf; Matsuo, Koji; Ciccone, Marcia A.; Matsuzaki, Shinya; Klar, Maximilian; Roman, Lynda D.; Sood, Anil K.; Gershenson, David M. (2020-05-29). "Molecular Pathways and Targeted Therapies for Malignant Ovarian Germ Cell Tumors and Sex Cord-Stromal Tumors: A Contemporary Review". Cancers. 12 (6): 1398. doi:10.3390/cancers12061398. ISSN 2072-6694. PMC 7353025. PMID 32485873.
- ↑ Grossman DC, Curry SJ, Owens DK, Barry MJ, Davidson KW, Doubeni CA, et al. (February 2018). "Screening for Ovarian Cancer: US Preventive Services Task Force Recommendation Statement". JAMA. 319 (6): 588–594. doi:10.1001/jama.2017.21926. PMID 29450531.
- ↑ 13.0 13.1 Gibson SJ, Fleming GF, Temkin SM, Chase DM (2016). "The Application and Outcome of Standard of Care Treatment in Elderly Women with Ovarian Cancer: A Literature Review over the Last 10 Years". Frontiers in Oncology. 6: 63. doi:10.3389/fonc.2016.00063. PMC 4805611. PMID 27047797.
- ↑ "SEER Stat Fact Sheets: Ovary Cancer". NCI. Archived from the original on 6 July 2014. Retrieved 18 June 2014.
- ↑ GBD 2015 Mortality and Causes of Death Collaborators (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ↑ GBD 2015 Disease and Injury Incidence and Prevalence Collaborators (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- ↑ 17.00 17.01 17.02 17.03 17.04 17.05 17.06 17.07 17.08 17.09 17.10 17.11 17.12 17.13 17.14 Seiden MV (2012). "Gynecologic Malignancies". In Longo DL, Kasper DL, Jameson JL, Fauci AS, Hauser SL, Loscalzo J (eds.). Harrison's Principles of Internal Medicine (18th ed.). McGraw-Hill. ISBN 978-0-07-174889-6.
- ↑ 18.0 18.1 18.2 "Ovarian Cancer, Inside Knowledge, Get the Facts about Gynecological Cancer" (PDF). Centers for Disease Control and Prevention. September 2016. Archived (PDF) from the original on June 16, 2017. Retrieved June 17, 2017.Samfuri:CDC
- ↑ 19.0 19.1 19.2 19.3 Jayson GC, Kohn EC, Kitchener HC, Ledermann JA (October 2014). "Ovarian cancer". Lancet. 384 (9951): 1376–88. doi:10.1016/S0140-6736(13)62146-7. PMID 24767708. S2CID 205971030.
- ↑ 20.00 20.01 20.02 20.03 20.04 20.05 20.06 20.07 20.08 20.09 20.10 20.11 Hoffman BL, Schorge JO, Schaffer JI, Halvorson LM, Bradshaw KD, Cunningham FG (2012). "Epithelial Ovarian Cancer". Williams Gynecology (2nd ed.). McGraw Hill Medical. pp. 853–878. ISBN 978-0-07-171672-7.
- ↑ "Ovarian cancer symptoms". www.cancerresearchuk.org. Archived from the original on 2015-05-12. Retrieved 2015-05-16.
- ↑ 22.00 22.01 22.02 22.03 22.04 22.05 22.06 22.07 22.08 22.09 "Ovarian cancer". DynaMed. June 18, 2015. Archived from the original on June 21, 2015.
- ↑ Williams Gynecology 2012
- ↑ 24.0 24.1 24.2 24.3 24.4 "Ovarian cancer risks and causes". Cancer Research UK. 15 January 2014. Archived from the original on 21 February 2015. Retrieved 29 January 2015.
- ↑ "Ovarian cancer risks and causes". Cancer Research UK. 15 January 2014. Archived from the original on 21 February 2015. Retrieved 29 January 2015.
- ↑ Manson JE, Bassuk SS (2012). "The Menopause Transition and Postmenopausal Hormone Therapy". In Longo DL, Kasper DL, Jameson JL, Fauci AS, Hauser SL, Loscalzo J (eds.). Harrison's Principles of Internal Medicine (18th ed.). McGraw-Hill. ISBN 978-0-07-174889-6.
- ↑ Empty citation (help)
- ↑ Kyriakidis I, Papaioannidou P (2016). "Estrogen receptor beta and ovarian cancer: a key to pathogenesis and response to therapy". Arch Gynecol Oncol. 293 (6): 1161–8. doi:10.1007/s00404-016-4027-8. PMID 26861465. S2CID 25627227.
- ↑ Norquist BM, Harrell MI, Brady MF, Walsh T, Lee MK, Gulsuner S, Bernards SS, Casadei S, Yi Q, Burger RA, Chan JK, Davidson SA, Mannel RS, DiSilvestro PA, Lankes HA, Ramirez NC, King MC, Swisher EM, Birrer MJ (2015). "Inherited mutations in women With ovarian carcinoma". JAMA Oncol. 30 (4): 1–9. doi:10.1001/jamaoncol.2015.5495. PMC 4845939. PMID 26720728.
- ↑ Kuusisto KM, Bebel A, Vihinen M, Schleutker J, Sallinen SL (2011). "Screening for BRCA1, BRCA2, CHEK2, PALB2, BRIP1, RAD50, and CDH1 mutations in high-risk Finnish BRCA1/2-founder mutation-negative breast and/or ovarian cancer individuals". Breast Cancer Res. 13 (1): R20. doi:10.1186/bcr2832. PMC 3109589. PMID 21356067.
- ↑ Hjartåker A, Meo MS, Weiderpass E (January 2010). "Alcohol and gynecological cancers: an overview". European Journal of Cancer Prevention. 19 (1): 1–10. doi:10.1097/CEJ.0b013e328333fb3a. PMID 19926999. S2CID 27570587.
- ↑ "Ovarian Cancer Risk Factors". cancer.org. Retrieved 2 January 2021.
- ↑ Qiu W, Lu H, Qi Y, Wang X. (2016). "Dietary fat intake and ovarian cancer risk: a meta-analysis of epidemiological studies". Oncotarget. 7 (24): 37390–37406. doi:10.18632/oncotarget.8940. PMC 5095084. PMID 27119509.CS1 maint: multiple names: authors list (link)
- ↑ Tanha, K., Mottaghi, A., Nojomi. (2021). "Investigation on factors associated with ovarian cancer: an umbrella review of systematic review and meta-analyses". Journal of Ovarian Research. 14 (1): 153. doi:10.1186/s13048-021-00911-z. PMC 8582179 Check
|pmc=value (help). PMID 34758846 Check|pmid=value (help).CS1 maint: multiple names: authors list (link) - ↑ Liao, Min-Qi (2020). "Effects of dairy products, calcium and vitamin D on ovarian cancer risk: A meta-analysis of twenty-nine epidemiological studies". British Journal of Nutrition. 124 (10): 1001–1012. doi:10.1017/S0007114520001075. PMID 32189606. S2CID 213181277.
- ↑ Sun H, Gong TT, Xia Y, Wen ZY, Zhao LG, Zhao YH, Wu QJ (2021). "Diet and ovarian cancer risk: An umbrella review of systematic reviews and meta-analyses of cohort studies". Clinical Nutrition. 40 (4): 1682–1690. doi:10.1016/j.clnu.2020.11.032. PMID 33308841. S2CID 229175041.CS1 maint: multiple names: authors list (link)
- ↑ Salehi F, Dunfield L, Phillips KP, Krewski D, Vanderhyden BC (March 2008). "Risk factors for ovarian cancer: an overview with emphasis on hormonal factors". Journal of Toxicology and Environmental Health Part B: Critical Reviews. 11 (3–4): 301–21. doi:10.1080/10937400701876095. PMID 18368558. S2CID 5589506.
- ↑ "Do we know what causes ovarian cancer?". www.cancer.org. Archived from the original on 2016-11-10.
- ↑ Empty citation (help)
- ↑ 40.0 40.1 Cite error: Invalid
<ref>tag; no text was provided for refs namedJayson - ↑ Cite error: Invalid
<ref>tag; no text was provided for refs named:74 - ↑ 42.0 42.1 Odunsi K, Pejovic T, Anderson ML (2011). Molecular Biology of Gynecologic Cancers. DeVita, Hellman, and Rosenberg's Cancer: Principles and Practice of Oncology. Wolters Kluwer/Lippincott Williams & Wilkins. pp. 1302–1310. ISBN 978-1-4511-0545-2.
- ↑ Empty citation (help)
- Pages with reference errors
- Harv and Sfn multiple-target errors
- Pages with empty citations
- CS1 maint: multiple names: authors list
- CS1 errors: PMC
- CS1 errors: PMID
- All articles with unsourced statements
- Articles with unsourced statements from March 2018
- Articles with invalid date parameter in template
- Shafuka masu fassarorin da ba'a duba ba
- Cutar daji
