Ciwon daji mai launi
| Ciwon daji mai launi | |
|---|---|
 | |
| Description (en) | |
| Iri |
colorectal neoplasm (en) cuta |
| Specialty (en) | oncology |
| Physical examination (en) |
colonoscopy (en) blood test (en) |
| Genetic association (en) |
TCF7L2 (en) |
| Medical treatment (en) | |
| Magani |
irinotecan (en) |
| Identifier (en) | |
| ICD-10 | C18, C20 da C21 |
| ICD-9 | 153.0 da 154.1 |
| ICD-O: | 8140 |
| OMIM | 114500 |
| DiseasesDB | 2975 |
| MedlinePlus | 000262 |
| eMedicine | 000262 |
| Disease Ontology ID | DOID:9256 |
Ciwon daji mai launi (CRC), wanda kuma aka sani da ciwon hanji, ciwon hanji, ko kansar dubura, shine ci gaban kansa daga hanji ko dubura (sassan babban hanji).[1] Ciwon daji shine rashin girma na sel wadanda ke da ikon mamayewa ko yada zuwa wasu sassan jiki.[2] Alamomi da alamomi na iya haɗawa da jini a cikin bayan gari, canjin hanji, raguwar nauyi, da jin gajiya koyaushe.[3]
Yawancin ciwon daji na launin fata suna faruwa ne saboda tsufa da kuma yau da kullum na rayuwar dan adam, tare da kananan adadin lokuta kawai saboda rashin lafiyar kwayoyin halitta.[4][5] Sauran abubuwan haɗari sun haɗa da abinci, kiba, shan taba, da rashin motsa jiki.[4] Abubuwan da ake ci waɗanda ke ƙara haɗarin sun haɗa da jan nama, naman da aka sarrafa, da barasa.[4][6] Wani abu mai haɗari shine cututtukan hanji mai kumburi, wanda kuma ya haɗa da cutar Crohn da ulcerative colitis.[4] Wasu daga cikin cututtukan da aka fada wadanda ke haifar da ciwon daji na launin fata sun hada da polyposis na iyali adenomatous polyposis da ciwon daji mara polyposis na hanji; duk da haka, wadannan suna wakiltar ƙasa da 5% na lokuta.[4][5] Yawanci yana farawa ne azaman ƙwayar cuta mara kyau, sau da yawa a cikin nau'in polyp, wanda bayan lokaci ya zama cutar kansa.[4]
Ana iya gano kansar hanji ta hanyar samun samfurin hanji a lokacin sigmoidoscopy ko colonoscopy.[3] Daga nan sai a yi hoton likita don sanin ko cutar ta yadu. Bincike yana da tasiri don hanawa da rage mace-mace daga ciwon daji na launin fata.[7] Ana ba da shawarar yin nuni, ta ɗayan hanyoyin da yawa, farawa daga shekaru 45 zuwa 75.[8] A lokacin colonoscopy, ana iya cire ƙananan polyps idan an same su.[4] Idan an sami babban polyp ko ƙari, ana iya yin biopsy don bincika ko ciwon daji ne. Aspirin da sauran magungunan anti-inflammatory marasa steroidal suna rage haɗarin.[4][9] Ba a ba da shawarar amfani da su gabaɗaya don wannan dalili ba, duk da haka, saboda illa.[10]
Magungunan da ake amfani da su don ciwon daji na launin fata na iya hadawa da wasu hadin tiyata, maganin radiation, chemotherapy da maganin da aka yi niyya.[1] Ciwon daji da ke tsare a bangon hanji na iya warkewa ta hanyar tiyata, yayin da ciwon daji da ya yaɗu a ko'ina ba zai iya warkewa ba, tare da kulawa da kulawa don inganta rayuwa da alamomi.[1] Yawan rayuwa na shekaru biyar a Amurka yana kusa da 65%.[11] Yiwuwar rayuwa ta mutum ya dogara da yadda ciwon daji ya ci gaba, ko za a iya kawar da kansa ko a'a tare da tiyata da kuma lafiyar mutum gaba ɗaya.[3] A duniya baki daya, ciwon daji na colorectal shine nau'in ciwon daji na uku da aka fi sani, wanda ke da kusan kashi 10% na dukkan cututtukan.[12] A cikin 2018, an sami sabbin mutane miliyan 1.09 da mutuwar 551,000 daga cutar.[13] Ya fi zama ruwan dare a kasashen da suka ci gaba, inda sama da kashi 65% na masu kamuwa da cutar ake samu.[4] Ba shi da yawa a cikin mata fiye da maza.[4]
Alamomi Cutar Daji
[gyara sashe | gyara masomin]Alamu da alamun ciwon daji na launi sun dogara ne akan wurin da ciwon daji ke cikin hanji, da kuma ko ya yada wani wuri a cikin jiki ( metastasis ). Alamomin faɗakarwa na yau da kullun sun haɗa da: ƙaran maƙarƙashiya, jini a cikin stool, raguwar stool caliber (kauri), asarar ci, asarar nauyi, da tashin zuciya ko amai a cikin wanda ya haura shekaru 50. [14] Kusan kashi 50 cikin 100 na mutanen da ke fama da ciwon daji ba sa bayar da rahoton wata alama. [15]
Zubar da jini na dubura ko anemia alamun haɗari ne a cikin mutane sama da shekaru 50. [16] Rage nauyi da canje-canje a al'adar hanjin mutum yawanci sun shafi kawai idan suna da alaƙa da zubar jini na dubura.[16][17]
Dalili
[gyara sashe | gyara masomin]Kashi 75-95% na cututtukan ciwon daji na launin fata suna faruwa a cikin mutanen da ba su da ƙarancin haɗarin kwayoyin halitta.[18][19] Abubuwan haɗari sun haɗa da tsufa, jima'i na maza, yawan cin mai, sukari, barasa, jan nama, naman da aka sarrafa, kiba, shan taba, da rashin motsa jiki .[18][20] Kusan kashi 10% na lokuta suna da alaƙa da rashin isasshen aiki.[21] Haɗarin barasa yana bayyana yana ƙaruwa fiye da abin sha ɗaya kowace rana.[22] Shan gilashin ruwa 5 a rana yana da alaƙa da raguwa a cikin haɗarin ciwon daji na launin fata da adenomatous polyps. [23] Streptococcus gallolyticus yana da alaƙa da ciwon daji na launi.[24] Miliyoyin mutane ne ke cinye wasu nau'ikan nau'ikan Streptococcus bovis/Streptococcus equinus a kullum don haka na iya zama lafiya.[25] 25 zuwa 80% na mutanen da ke da Streptococcus bovis/gallolyticus bacteremia suna da ciwace-ciwacen launin fata.[26] Seroprevalence na Streptococcus bovis/gallolyticus ana ɗaukarsa azaman ɗan takara alama mai amfani don farkon hasashen raunin hanji mai fa'ida a cikin haɗarin yawan jama'a. An ba da shawarar cewa kasancewar ƙwayoyin rigakafi ga Streptococcus bovis/gallolyticus antigens ko antigens da kansu a cikin jini na iya zama alamomi ga carcinogenesis a cikin hanji.
Pathogenic Escherichia coli na iya ƙara haɗarin ciwon daji na launi ta hanyar samar da kwayoyin halitta na genotoxic, colibactin .[27]
Ciwon ciki mai kumburi
[gyara sashe | gyara masomin]Mutanen da ke da cututtukan hanji mai kumburi ( ulcerative colitis da cutar Crohn ) suna cikin haɗarin kamuwa da ciwon daji na hanji. [28][29] Haɗarin yana ƙaruwa tsawon lokacin da mutum ke da cutar, kuma mafi muni da tsananin kumburi.[30] A cikin waɗannan ƙungiyoyi masu haɗari masu haɗari, ana ba da shawarar rigakafin aspirin da na yau da kullun . [30] Sa ido na Endoscopic a cikin wannan yawan mutanen da ke da haɗari na iya rage haɓakar ciwon daji na launin fata ta hanyar ganewar asali da wuri kuma yana iya rage yiwuwar mutuwa daga ciwon daji na hanji. Mutanen da ke da cututtukan hanji mai kumburi suna lissafin ƙasa da 2% na cututtukan daji na hanji kowace shekara. A cikin wadanda ke da cutar Crohn, kashi 2 cikin 100 suna samun kansar launin fata bayan 10 8% bayan shekaru 20 shekaru, da kuma 18% bayan shekaru 30. A cikin mutanen da ke da ulcerative colitis, kimanin kashi 16 cikin dari suna tasowa ko dai ciwon daji ko ciwon daji na hanji fiye da 30. shekaru.
Genetics
[gyara sashe | gyara masomin]Wadanda ke da tarihin iyali a cikin dangi biyu ko fiye da na farko (kamar iyaye ko 'yan'uwa) suna da haɗarin kamuwa da cuta sau biyu zuwa uku kuma wannan rukunin yana da kusan kashi 20% na duk lokuta. Yawan cututtukan cututtukan ƙwayoyin cuta kuma suna da alaƙa da haɓakar cutar kansar launin fata. Mafi na kowa daga cikin waɗannan shine ciwon daji marasa polyposis colorectal (HNPCC ko Lynch syndrome) wanda ke cikin kusan kashi 3% na mutanen da ke fama da ciwon daji. Sauran cututtukan da ke da alaƙa da ciwon daji mai ƙarfi sun haɗa da ciwon Gardner da adenomatous polyposis na iyali (FAP).[31] Ga mutanen da ke da waɗannan cututtukan, ciwon daji kusan koyaushe yana faruwa kuma yana da kashi 1% na cututtukan daji.[32] Ana iya ba da shawarar jimlar proctocolectomy ga mutanen da ke da FAP a matsayin ma'aunin rigakafi saboda babban haɗarin malignancy. Colectomy, cire hanji, bazai isa a matsayin ma'aunin rigakafi ba saboda babban haɗarin ciwon daji na dubura idan duburar ta kasance.[33] Mafi yawan ciwon polyposis da ke shafar hanji shine serrated polyposis syndrome,[34] wanda ke da alaƙa da haɗarin 25-40% na CRC.[35]
Maye gurbi a cikin nau'ikan kwayoyin halitta ( POLE da POLD1 ) an haɗa su da ciwon daji na iyali.[36]
Yawancin mace-mace saboda ciwon daji na hanji suna da alaƙa da cutar metastatic. Halin da ke bayyana yana taimakawa wajen yiwuwar cutar cututtuka, metastasis da ke hade da ciwon daji na hanji 1 ( MACC1 ), an ware shi.[37] Wani abu ne na rubutun da ke tasiri ga bayanin haɓakar haɓakar hanta . Wannan jinsin yana da alaƙa da yaduwa, mamayewa da watsar da ƙwayoyin cutar kansar hanji a cikin al'adar tantanin halitta, da haɓakar ƙari da metastasis a cikin mice. MACC1 na iya zama manufa mai yuwuwa don shiga tsakani na kansa, amma ana buƙatar tabbatar da wannan yuwuwar tare da nazarin asibiti. [38]
Abubuwan Epigenetic, irin su methylation na DNA mara kyau na masu haɓaka ƙari, suna taka rawa wajen haɓaka ciwon daji na launin fata. [39]
Yahudawan Ashkenazi suna da kashi 6% na hadarin kamuwa da adenoma sannan kuma ciwon daji na hanji saboda maye gurbi a cikin kwayar halittar APC da ya fi yawa.[40]
Pathogenesis
[gyara sashe | gyara masomin]Ciwon daji mai launi cuta ce da ta samo asali daga sel epithelial da ke rufe hanji ko dubura na gastrointestinal tract, galibi sakamakon maye gurbi a cikin hanyar siginar Wnt wanda ke haɓaka ayyukan sigina. Ana iya gada ko samun maye gurbin, kuma galibi yana faruwa ne a cikin kwayar cutar ta hanji .[41][42][43] Mafi yawan rikitattun kwayoyin halitta a cikin dukkan ciwon daji na launin fata shine kwayar halittar APC, wanda ke samar da furotin na APC. Protein na APC yana hana tarin furotin β-catenin . Ba tare da APC ba, β-catenin yana tarawa zuwa manyan matakan kuma ya canza (motsi) zuwa cikin tsakiya, yana ɗaure zuwa DNA, kuma yana kunna fassarar proto -oncogenes . Waɗannan kwayoyin halitta galibi suna da mahimmanci don sabuntawa da bambance-bambancen kwayar halitta, amma idan aka bayyana rashin dacewa a manyan matakan, suna iya haifar da ciwon daji. Yayin da APC ke canzawa a yawancin ciwon daji na hanji, wasu ciwon daji sun karu da β-catenin saboda maye gurbi a cikin β-catenin (CTNNB1) wanda ke toshe rushewar kansa, ko kuma yana da maye gurbi a cikin wasu kwayoyin halitta masu aiki irin na APC kamar AXIN1, AXIN2, TCF7L2 ., ko NKD1 .[44]
Bayan lahani a cikin hanyar siginar Wnt, wasu maye gurbi dole ne su faru don tantanin halitta ya zama mai cutar kansa. Sunan furotin p53, wanda aka samar ta hanyar TP53 gene, yawanci yana lura da rarrabuwar tantanin halitta kuma yana haifar da tsarin mutuwar su idan suna da lahani na hanyar Wnt. Daga ƙarshe, layin tantanin halitta ya sami maye gurbi a cikin kwayar halittar TP53 kuma yana canza nama daga ƙwayar ƙwayar cuta mara kyau zuwa ciwon daji na sel na epithelial . Wani lokaci kwayar halittar p53 ba ta canza ba, amma wani furotin mai kariya mai suna BAX an canza shi a maimakon haka. [45]
Sauran sunadaran da ke da alhakin mutuwar kwayar cutar da aka yi amfani da su da yawa a cikin ciwon daji na colorectal sune TGF-β da DCC ( An share a cikin Ciwon daji na Colorectal ). TGF-β yana da maye gurbi mai kashewa a cikin aƙalla rabin ciwon daji na launin fata. Wani lokaci TGF-β ba a kashe shi ba, amma ana kashe furotin na ƙasa mai suna SMAD . [45] DCC yawanci yana da share ɓangaren chromosome a cikin ciwon daji mai launi. [45]
Kusan kashi 70 cikin 100 na dukkanin kwayoyin halittar dan adam ana bayyana su a cikin ciwon daji na launin fata, tare da kusan kashi 1% na yawan bayyanar cututtuka a cikin ciwon daji idan aka kwatanta da sauran nau'in ciwon daji. [45] Wasu kwayoyin halitta su ne oncogenes : suna da yawa a cikin ciwon daji na colorectal. Alal misali, kwayoyin halittar da ke ɓoye sunadaran KRAS, RAF, da PI3K, waɗanda yawanci ke motsa tantanin halitta don rarrabawa don amsawa ga abubuwan haɓaka, na iya samun maye gurbin da ke haifar da haɓakar haɓakar kwayar halitta. Tsarin lokaci na maye gurbi yana da mahimmanci a wasu lokuta. Idan maye gurbin APC na baya ya faru, maye gurbin KRAS na farko sau da yawa yakan ci gaba zuwa ciwon daji maimakon cutar hawan jini mai iyakancewa ko raunin iyaka. [45] PTEN, mai hana ƙari, yawanci yana hana PI3K, amma wani lokaci yana iya zama rikiɗewa kuma yana kashewa. [45]
M, bincike-bincike-genome ya bayyana cewa za a iya rarraba carcinomas masu launin launin fata zuwa nau'in ciwon daji da marasa hawan jini. [46] Bugu da ƙari, maye gurbi na oncogenic da inactivating da aka kwatanta don kwayoyin halitta a sama, samfurori marasa hypermutated sun ƙunshi CTNNB1, FAM123B, SOX9, ATM, da ARID1A . Ci gaba ta hanyar wani nau'i na abubuwan da suka faru na kwayoyin halitta, hypermutated ciwace-ciwacen daji suna nuna nau'i na ACVR2A, TGFBR2, MSH3, MSH6, SLC9A9, TCF7L2, da BRAF . Maganar gama gari tsakanin waɗannan kwayoyin halitta, a duk nau'in ciwon daji, shine shigar da su a cikin hanyoyin siginar Wnt da TGF-β, wanda ke haifar da ƙara yawan aiki na MYC, dan wasa na tsakiya a cikin ciwon daji na launi. [46]
Rashin haɓakar ciwace- ciwacen ciwace-ciwace (MMR) ana siffanta shi da ɗan ƙaramin adadin maimaita tandem na poly-nucleotide.[47] Wannan yana faruwa ne ta hanyar rashi a cikin sunadaran MMR - waɗanda yawanci ke haifar da su ta hanyar shiru na epigenetic da ko maye gurbi (misali. Lynch ciwo ). [48] 15 zuwa 18 bisa dari na ciwace-ciwacen daji na launin launi suna da raunin MMR, tare da kashi 3 cikin dari suna tasowa saboda ciwo na Lynch. [45] Matsayin tsarin gyare-gyaren rashin daidaituwa shine kare mutuncin kwayoyin halitta a cikin sel (watau: gano kuskure da gyarawa). Sakamakon haka, rashi a cikin sunadaran MMR na iya haifar da rashin iya ganowa da gyara lalacewar kwayoyin halitta, yana ba da damar ci gaba da haifar da maye gurbi da ciwon daji na launin fata ya ci gaba.
Polyp zuwa jeri na ci gaban kansa shine samfurin gargajiya na cututtukan ciwon daji na colorectal. [49] Tsarin polyp zuwa jerin ciwon daji yana bayyana matakan sauye-sauye daga ciwace-ciwacen daji zuwa ciwon daji na launin fata tsawon shekaru masu yawa. Tsakanin polyp zuwa jerin CRC sune maye gurbi, sauye-sauyen epigenetic da canje-canje masu kumburi na gida. Za a iya amfani da jerin polyp zuwa CRC azaman tushen tsarin don kwatanta yadda takamaiman canje-canjen kwayoyin ke haifar da nau'ikan ciwon daji daban-daban.
Lalacewar filin
[gyara sashe | gyara masomin]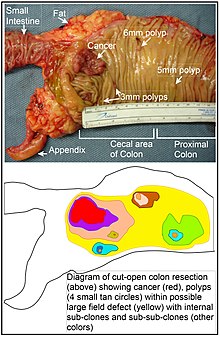
An fara amfani da kalmar "ciwon daji na filin" a cikin 1953 don bayyana wani yanki ko "filin" na epithelium wanda aka riga aka tsara (ta hanyar abubuwan da ba a san su ba a lokacin) don ƙaddamar da shi zuwa ci gaban ciwon daji. Tun daga wannan lokacin, an yi amfani da kalmomin "ciwon daji na filin", "carcinogenesis filin", "lalacewar filin", da " tasirin filin " don bayyana cutar da ta rigaya ko riga-kafin neoplastic wanda sabon ciwon daji zai iya tasowa.
Lalacewar filin suna da mahimmanci wajen ci gaba zuwa kansar hanji. [50]
Duk da haka, kamar yadda Rubin ya nuna, "Yawancin binciken da aka yi a cikin binciken ciwon daji an yi shi ne akan ciwace-ciwacen ciwace-ciwacen ƙwayoyi a cikin vivo, ko kuma a kan ƙananan ƙwayoyin neoplastic foci in vitro . Amma duk da haka akwai shaidar cewa fiye da kashi 80 cikin 100 na maye gurbi da aka samu a cikin mutator phenotype ɗan adam ciwace-ciwacen ciwace-ciwacen ciwace-ciwacen ciwace-ciwacen ciwace-ciwacen ciwace-ciwace na faruwa ne kafin farkon haɓakawar haɓakar clonal na ƙarshe." [45] [45] Hakanan, Vogelstein et al. [45] ya nuna cewa fiye da rabin maye gurbi da aka gano a cikin sun faru ne a wani lokaci na pre-neoplastic (a cikin wani lahani na fili), yayin haɓakar sel na zahiri. Hakanan, sauye-sauyen epigenetic da ke cikin ciwace-ciwace na iya faruwa a cikin lahani na filin pre-neoplastic. [45]
An faɗaɗa ra'ayi game da tasirin filin "tasirin filin etiologic", wanda ya ƙunshi ba wai kawai kwayoyin halitta da canje-canjen pathologic a cikin sel pre-neoplastic ba har ma da tasirin abubuwan muhalli na waje da canje-canjen ƙwayoyin cuta a cikin ƙananan ƙwayoyin cuta na gida akan juyin halitta na neoplastic daga farkon ƙari zuwa mutuwa. . [51]
Epigenetics
[gyara sashe | gyara masomin]Canje-canjen Epigenetic sun fi yawa a cikin ciwon daji na hanji fiye da sauye-sauyen kwayoyin halitta (mutational). Kamar yadda aka bayyana ta Vogelstein et al., [45] matsakaicin ciwon daji na hanji yana da maye gurbi na 1 ko 2 na oncogene kawai da 1 zuwa 5 na maye gurbi (tare da "canza maye gurbin direba"), tare da ƙarin maye gurbin "fasinja" kusan 60. An yi nazarin kwayoyin halittar oncogenes da ƙwayoyin cuta masu hana ƙari kuma an kwatanta su a sama a ƙarƙashin Pathogenesis .[52][53]
Bugu da ƙari, canjin epigenetic na magana na miRNAs, sauran nau'ikan sauye-sauye na epigenetic na yau da kullun a cikin cututtukan daji waɗanda ke canza matakan maganganu na kwayar halitta sun haɗa da hypermethylation kai tsaye ko hypomethylation na tsibiran CpG na ƙwayoyin halittar furotin da sauye-sauye a cikin tarihin tarihi da gine-ginen chromosomal waɗanda ke yin tasiri ga bayyanar halittar. [54] A matsayin misali, 147 hypermethylations da 27 hypomethylations na furotin codeing genes aka akai-akai hade da colorectal cancers. Daga cikin kwayoyin hypermethylated, 10 sun kasance hypermethylated a cikin 100% na ciwon daji na hanji, kuma wasu da yawa sun kasance hypermethylated a cikin fiye da 50% na ciwon daji na hanji. [55] Bugu da ƙari, 11 hypermethylations da 96 hypomethylations na miRNAs suma suna da alaƙa da ciwon daji na launi. methylation mara kyau (aberrant) yana faruwa ne a sakamakon al'ada na al'ada na al'ada kuma haɗarin ciwon daji na launin fata yana ƙaruwa yayin da mutum ya tsufa. [45] Ba a san tushen da abin da ke haifar da wannan methylation mai alaƙa da shekaru ba. [45] [45] Kusan rabin kwayoyin halittar da ke nuna sauye-sauyen methylation masu alaka da shekaru su ne kwayoyin halittar da aka gano suna da hannu wajen haifar da ciwon sankarar launi. [45] Wadannan binciken na iya ba da shawarar dalilin shekaru da ke hade da haɗarin haɓakar ciwon daji na launin fata. [45]
Ragewar Epigenetic na maganan gyaran enzyme na DNA na iya haifar da rashin zaman lafiyar kwayoyin halitta da na epigenomic na ciwon daji. [56][57][58] Kamar yadda aka taƙaita a cikin articles Carcinogenesis da Neoplasm, don ciwon daji na lokaci-lokaci a gaba ɗaya, ƙarancin gyare-gyare na DNA yana faruwa lokaci-lokaci saboda maye gurbi a cikin kwayar gyaran DNA, amma yana da yawa akai-akai saboda sauye-sauye na epigenetic wanda ke rage ko yin shiru na maganganun gyaran DNA. .[59]
Canje-canjen Epigenetic da ke cikin haɓakar ciwon daji na launin fata na iya shafar martanin mutum ga ilimin chemotherapy.[60]
Genomics | Epigenomics
[gyara sashe | gyara masomin]Ijma'i na kwayoyin subtypes (CMS) na rarrabuwar kansar launin fata an fara gabatar da shi a cikin 2015. Rarraba CMS ya zuwa yanzu an yi la'akari da mafi ƙaƙƙarfan tsarin rarrabawa da ake da shi don CRC wanda ke da fassarorin fassarar ilimin halitta da tushe don rarrabuwa na asibiti a nan gaba da kuma matakan da aka yi niyya na tushen nau'in.[61]
Wani labari na tushen Epigenome (EpiC) na kansar launin fata an gabatar da shi a cikin 2021 yana gabatar da nau'ikan haɓakawa 4 a cikin mutanen da ke da CRC. Jihohin Chromatin da ke amfani da alamomin tarihi guda 6 ana siffanta su don gano ƙananan nau'ikan EpiC. Hanyar haɗakarwa ta hanyar warkewa dangane da abubuwan da aka gabatar da ijma'i a baya (CMSs) da EpiCs na iya haɓaka dabarun jiyya na yanzu. [45]
Bincike
[gyara sashe | gyara masomin]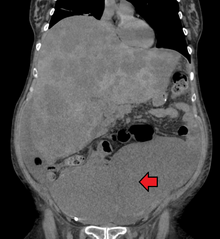
Ana yin ganewar cutar kansar launin fata ta hanyar yin samfuri na wuraren da ake zargin hanji don yuwuwar ci gaban ƙari, yawanci a lokacin colonoscopy ko sigmoidoscopy, ya danganta da wurin da raunin ya kasance. An tabbatar da shi ta hanyar duban ɗan adam na samfurin nama.[ana buƙatar hujja]
Hoto na likita
[gyara sashe | gyara masomin]Wani lokaci ana gano ciwon daji mai launin fata akan CT scan . [62]
Ana tabbatar da kasancewar metastases ta hanyar CT scan na ƙirji, ciki da ƙashin ƙugu. Wasu yuwuwar gwajin hoto kamar PET da MRI ana iya amfani da su a wasu lokuta. Ana amfani da na ƙarshen sau da yawa don raunukan dubura don tantance matakin sa na gida da kuma sauƙaƙe shirye-shiryen riga-kafi.
Histopathology
[gyara sashe | gyara masomin]

Ana ba da rahoton halayen tarihin tarihin ƙwayar cuta daga nazarin nama da aka ɗauka daga biopsy ko tiyata. Rahoton ilimin cututtuka yana ƙunshe da bayanin halayen ƙananan ƙwayoyin ƙwayar ƙwayar cuta, ciki har da ƙwayoyin tumor guda biyu da kuma yadda ciwon daji ke shiga cikin kyallen takarda masu lafiya kuma a ƙarshe idan ciwon ya bayyana an cire shi gaba daya. Mafi yawan nau'in ciwon daji na hanji shine adenocarcinoma, wanda ya ƙunshi tsakanin kashi 95% [63] zuwa 98% [64] na duk cututtukan daji na colorectal. Sauran, nau'ikan da ba su da yawa sun haɗa da lymphoma, adenosquamous da carcinoma cell squamous . An gano wasu nau'ikan nau'ikan suna da ƙarfi [65] Ana iya amfani da Immunohistochemistry a lokuta marasa tabbas.[66]
Tsayawa
[gyara sashe | gyara masomin]Matsayin ciwon daji ya dogara ne akan binciken rediyo da ilimin cututtuka. Kamar yadda yake tare da sauran nau'o'in ciwon daji, ciwon daji yana dogara ne akan tsarin TNM wanda yayi la'akari da yadda ƙwayar farko ta yada da kuma kasancewar metastases a cikin nodes na lymph da sauran gabobin da ke nesa. An buga bugu na AJCC na 8 a cikin 2018.[67]
Rigakafi
[gyara sashe | gyara masomin]An yi kiyasin cewa kusan rabin cututtukan da suka kamu da cutar sankarar launin fata suna faruwa ne saboda abubuwan rayuwa, kuma kusan kashi ɗaya bisa huɗu na duk ana iya yin rigakafinsu.[68] Ƙara yawan sa ido, yin motsa jiki, cin abinci mai yawan fiber, da rage shan taba da shan barasa yana rage haɗarin.[69][70]
salon rayuwa
[gyara sashe | gyara masomin]Abubuwan haɗari na rayuwa tare da shaida mai ƙarfi sun haɗa da rashin motsa jiki, shan taba sigari, barasa, da kiba. [71][72] Ana iya rage haɗarin ciwon daji na hanji ta hanyar kiyaye nauyin jiki na yau da kullun ta hanyar haɗuwa da isasshen motsa jiki da cin abinci mai kyau .[73]
Binciken da ake yi a yanzu yana danganta cin jan nama da naman da aka sarrafa zuwa babban haɗarin cutar. [74] Tun daga shekarun 1970s, shawarwarin abinci don hana ciwon daji na launin fata sau da yawa sun haɗa da ƙara yawan amfani da hatsi, 'ya'yan itatuwa da kayan marmari, da rage cin nama da nama da aka sarrafa . Wannan ya dogara ne akan nazarin dabba da nazarin duban baya. Duk da haka, babban binciken da ake tsammani ya kasa nuna wani tasiri mai mahimmanci na kariya, kuma saboda dalilai masu yawa na ciwon daji da kuma rikitarwa na nazarin dangantaka tsakanin abinci da lafiya, ba shi da tabbas ko wani takamaiman tsarin abinci na abinci (a waje da cin abinci mai kyau) zai sami tasiri mai mahimmanci na kariya. [75] :432–433[75] :125–126A cikin 2018 Cibiyar Ciwon daji ta Kasa ta bayyana cewa "Babu wani tabbataccen shaida cewa abincin da aka fara a lokacin balagagge wanda ba shi da kitse da nama da yawan fiber, 'ya'yan itatuwa, da kayan lambu yana rage haɗarin CRC ta hanyar digiri mai mahimmanci na asibiti." [74] [74]
A cewar Asusun Binciken Ciwon daji na Duniya, shan barasa da kuma cinye naman da aka sarrafa duka suna kara haɗarin ciwon daji na colorectal [76]
Game da fiber na abinci, rahoton ciwon daji na Hukumar Lafiya ta Duniya na 2014 ya lura cewa an yi hasashen cewa fiber na iya taimakawa wajen hana ciwon daji na colorectal, amma yawancin binciken ba su fitar da wannan ba, kuma matsayin kimiyya ya kasance ba a sani ba tun daga 2014. [77] Wani bita na 2019, duk da haka, ya sami shaidar fa'ida daga fiber na abinci da dukan hatsi. [78] Asusun Binciken Ciwon daji na Duniya ya lissafa fa'idar fiber don rigakafin ciwon daji a matsayin "mai yiwuwa" kamar na 2017.
Ana ba da shawarar aikin motsa jiki mafi girma. Motsa jiki yana da alaƙa da raguwar raguwar hanji amma ba haɗarin kansar dubura ba. [79][80] Babban matakan motsa jiki yana rage haɗarin ciwon daji na hanji da kusan kashi 21%. [81] Zauna akai-akai na tsawon lokaci yana da alaƙa da yawan mace-mace daga ciwon daji na hanji. Ba a kawar da haɗarin ta hanyar motsa jiki na yau da kullum, kodayake an saukar da shi.
Magunguna da kari
[gyara sashe | gyara masomin]Aspirin da celecoxib sun bayyana suna rage haɗarin ciwon daji na launin fata a cikin waɗanda ke cikin haɗari mai girma. [82][83] Ana ba da shawarar aspirin ga waɗanda ke da shekaru 50 zuwa 60, ba su da haɗarin zubar jini, kuma suna cikin haɗarin kamuwa da cututtukan zuciya don hana ciwon daji na launin fata.[84] Ba a ba da shawarar ba a cikin waɗanda ke cikin matsakaicin haɗari.[85]
Akwai sheda na ƙayyadaddun ƙayyadaddun ƙwayar calcium, amma bai isa ba don ba da shawara. [86] Shan bitamin D da matakan jini suna da alaƙa da ƙarancin haɗarin ciwon daji na hanji. [87][88]
Nunawa
[gyara sashe | gyara masomin]Kamar yadda fiye da 80% na ciwon daji na colorectal ya tashi daga adenomatous polyps, nunawa ga wannan ciwon daji yana da tasiri don ganowa da wuri da kuma rigakafi. [89] Ganewar cututtukan ciwon daji na launin fata ta hanyar yin gwaje-gwaje yana nuna yakan faru shekaru 2-3 kafin ganewar asali na lokuta masu alamun bayyanar. Ana iya cire duk wani polyps da aka gano, yawanci ta hanyar colonoscopy ko sigmoidoscopy, don haka ya hana su juya zuwa ciwon daji. Nunawa yana da yuwuwar rage mutuwar cutar kansar launin fata da kashi 60%. [90]
Babban gwaje-gwajen gwaji guda uku sune colonoscopy, gwajin jini na gabobin ciki, da sigmoidoscopy mai sassauƙa . Daga cikin ukun, sigmoidoscopy kawai ba zai iya bincika gefen dama na hanji ba inda aka sami kashi 42% na ciwon daji. [91] Sigmoidoscopy mai sauƙi, duk da haka, yana da mafi kyawun shaida don rage haɗarin mutuwa daga kowane dalili.[92]
Gwajin jini na ɓoyayyiya (FOBT) na stool yawanci ana ba da shawarar kowace shekara biyu kuma yana iya zama tushen guaiac ko immunochemical . [45] Idan an sami sakamako na FOBT mara kyau, yawanci ana tura mahalarta don gwajin colonoscopy na gaba. Lokacin da aka yi sau ɗaya a kowace shekara 1-2, gwajin FOBT yana rage yawan mutuwar ciwon daji da kashi 16 cikin 100 kuma daga cikin waɗanda ke shiga cikin tantancewa, za a iya rage yawan mutuwar ciwon daji har zuwa 23%, ko da yake ba a tabbatar da rage yawan mace-mace ba. [93] Gwaje-gwajen rigakafi daidai ne kuma baya buƙatar canjin abinci ko magani kafin gwaji. [94]
Sauran zaɓuɓɓukan sun haɗa da kama-da -wane colonoscopy da gwajin gwajin DNA (FIT-DNA). Ƙwararren ƙwayar cuta ta hanyar CT scan ya bayyana yana da kyau kamar daidaitaccen colonoscopy don gano ciwon daji da manyan adenoma amma yana da tsada, yana da alaƙa da bayyanar radiation, kuma ba zai iya cire duk wani ci gaban da aka gano na al'ada ba kamar yadda daidaitaccen colonoscopy zai iya. [45] Gwajin gwajin DNA na Stool yana neman alamomin halittu masu alaƙa da ciwon daji na launin fata da raunukan da suka rigaya, gami da canza DNA da haemoglobin na jini . Kyakkyawan sakamako yakamata a bi shi ta hanyar colonoscopy . FIT-DNA yana da mafi ƙarancin inganci fiye da FIT kuma don haka yana haifar da ƙarin sakamako mara kyau. Ana buƙatar ƙarin bincike kamar na 2016 don sanin ko tazarar gwajin shekaru uku daidai ne.
Shawarwari
[gyara sashe | gyara masomin]A Amurka, ana ba da shawarar yin gwajin tsakanin shekaru 50 zuwa 75 shekaru. Ƙungiyar Ciwon daji ta Amirka ta ba da shawarar farawa tun yana da shekaru 45. [45] Ga waɗanda ke tsakanin shekaru 76 zuwa 85, yanke shawarar tantancewa ya kamata a keɓance shi. Ga waɗanda ke cikin haɗarin haɗari, yawanci ana farawa da kusan 40.[95]
Ana ba da shawarar hanyoyin dubawa da yawa ciki har da gwajin tushen stool kowane shekaru 2, sigmoidoscopy kowace shekara 10 tare da gwajin rigakafi na fecal a kowace shekara biyu, da colonoscopy kowace shekara 10. [45] Ba a san wanne daga cikin waɗannan hanyoyi biyu ba ne mafi kyau. Colonoscopy na iya samun ƙarin ciwon daji a ɓangaren farko na hanji, amma yana da alaƙa da farashi mai girma da ƙarin rikitarwa. [96] Ga mutanen da ke da matsakaicin haɗari waɗanda suka sami babban ingancin colonoscopy tare da sakamako na al'ada, Ƙungiyar Gastroenterological Association ta Amirka ba ta ba da shawarar kowane nau'i na nunawa a cikin shekaru 10 bayan colonoscopy ba.[97][98] Ga mutane sama da 75 ko waɗanda ke da tsawon rayuwar ƙasa da 10 shekaru, ba a ba da shawarar dubawa ba. [99] Yana ɗaukar kimanin shekaru 10 bayan an gwada ɗaya daga cikin mutane 1000 don amfana. [100] USPSTF ta lissafta dabaru guda bakwai masu yuwuwa don tantancewa, tare da mafi mahimmancin abu shine cewa aƙalla ɗaya daga cikin waɗannan dabarun ana amfani da su yadda ya kamata.
A Kanada, daga cikin waɗanda ke da shekaru 50 zuwa 75 a cikin haɗarin al'ada, ana ba da shawarar gwajin rigakafi na fecal ko FOBT kowace shekara biyu ko sigmoidoscopy kowace shekara 10. [45] Colonoscopy ba shi da fifiko.
Wasu ƙasashe suna da shirye-shiryen tantance launin launi na ƙasa waɗanda ke ba da gwajin FOBT ga duk manya a cikin wani rukunin shekaru, yawanci farawa tsakanin shekaru 50 zuwa 60. Misalan ƙasashen da ke da tsarin tantancewa sun haɗa da United Kingdom, [101] Australia, [102] Netherlands, [103] Hong Kong da Taiwan. [104]
Magani
[gyara sashe | gyara masomin]Maganin ciwon daji na launin fata na iya zama da nufin warkarwa ko ragewa. Shawarar abin da ake son ɗauka ya dogara da abubuwa daban-daban, ciki har da lafiyar mutum da abubuwan da ake so, da kuma matakin ƙwayar cuta. [105] Ƙididdiga a cikin ƙungiyoyi masu yawa shine muhimmin sashi na ƙayyade ko majiyyaci ya dace da tiyata ko a'a. [106] Lokacin da aka kama kansar launin fata da wuri, tiyata na iya zama magani. Duk da haka, lokacin da aka gano shi a matakai na gaba (wanda metastases ke samuwa), wannan yana da wuyar gaske kuma sau da yawa ana ba da magani ga palliation, don kawar da bayyanar cututtuka da ciwon daji ke haifar da shi kuma ya sa mutum ya ji dadi sosai.
Tiyata
[gyara sashe | gyara masomin]

Idan an sami ciwon daji a farkon mataki, ana iya cire shi a lokacin colonoscopy ta amfani da daya daga cikin fasaha da yawa, ciki har da endoscopic mucosal resection ko endoscopic submucosal dissection . Ga mutanen da ke da ciwon daji na gida, abin da aka fi so shine cikakken cirewar tiyata tare da isassun tazara, tare da ƙoƙarin samun magani. Hanyar zaɓin ita ce partel colectomy (ko proctocolectomy don raunukan duburar) inda aka cire ɓangaren hanji ko duburar da abin ya shafa tare da sassan mesocolon da samar da jini don sauƙaƙe cire ƙwayoyin lymph nodes . Ana iya yin wannan ko dai ta hanyar buɗewar laparotomy ko laparoscopically, dangane da abubuwan da suka shafi mutum ɗaya da abubuwan raunuka. Ana iya sake haɗa hanjin ko kuma mutum ya sami colostomy .
Idan akwai 'yan metastases a cikin hanta ko huhu, ana iya cire su. Ana iya amfani da chemotherapy kafin tiyata don rage ciwon daji kafin yunƙurin cire shi. Wurare guda biyu da aka fi samun yawaitar cutar kansar launin fata sune hanta da huhu . Ga peritoneal carcinomatosis cytoreductive tiyata, wani lokacin a hade tare da HIPEC za a iya amfani da a yunƙurin cire ciwon daji. [107]
Chemotherapy
[gyara sashe | gyara masomin]A cikin duka ciwon daji na hanji da dubura, ana iya amfani da chemotherapy ban da tiyata a wasu lokuta. Shawarar da za a ƙara chemotherapy a kula da ciwon hanji da dubura ya dogara da matakin cutar. [108]
A Stage I ciwon daji na hanji, ba a bayar da chemotherapy, kuma tiyata shine tabbataccen magani. Matsayin ilimin chemotherapy a cikin Stage II ciwon daji na hanji yana da muhawara, kuma yawanci ba a ba da shi ba sai an gano abubuwan haɗari kamar ƙwayar cutar T4, ciwon daji mara bambanci, mamayewar jijiyoyin jini da na perineural ko rashin isasshen samfurin node na lymph. [109] Hakanan an san cewa mutanen da ke ɗauke da abubuwan da ba su da kyau na ƙwayoyin gyaran gyare-gyaren da ba su dace ba ba su amfana da ilimin chemotherapy. Don mataki na III da Stage IV ciwon daji, chemotherapy wani bangare ne na jiyya.
Idan ciwon daji ya yada zuwa ga ƙwayoyin lymph ko gabobin da ke nesa, wanda shine yanayin da mataki na III da mataki na IV ciwon daji na ciwon hanji, ƙara magungunan chemotherapy fluorouracil, capecitabine ko oxaliplatin yana ƙara tsawon rai. Idan nodes na lymph ba su ƙunshi ciwon daji ba, amfanin chemotherapy yana da rikici. Idan ciwon daji yana da yawa ko kuma ba a sake shi ba, to magani yana da lafiya. Yawanci a wannan saitin, ana iya amfani da adadin magungunan chemotherapy daban-daban. Magungunan chemotherapy don wannan yanayin na iya haɗawa da capecitabine, fluorouracil, irinotecan, oxaliplatin da UFT . [110] Magungunan capecitabine da fluorouracil suna canzawa, tare da capecitabine kasancewar maganin baka da fluorouracil shine maganin jijiya. Wasu ƙayyadaddun ƙayyadaddun tsarin da ake amfani da su don CRC sune CAPOX, FOLFOX, FOLFOXIRI, da FOLFIRI . [111] Magungunan Antiangiogenic kamar su bevacizumab ana yawan ƙara su a cikin layin farko. Wani nau'i na kwayoyi da aka yi amfani da su a cikin layi na biyu sune masu hana masu karɓan haɓakar haɓakar haɓakar epidermal, waɗanda FDA ta amince da su guda uku suna aflibercept, cetuximab da panitumumab . [112][113]
Bambanci na farko a cikin kusanci zuwa ƙananan ciwon daji na dubura shine haɗa maganin radiation. Sau da yawa, ana amfani da shi tare da chemotherapy a cikin yanayin neoadjuvant don ba da damar aikin tiyata, ta yadda a ƙarshe ba a buƙatar colostomy . Koyaya, bazai yuwu a cikin ƙananan ciwace-ciwacen daji ba, a cikin wannan yanayin, ana iya buƙatar colostomy na dindindin. Ana kula da ciwon daji na dubura mataki na IV kama da mataki na IV ciwon daji.
Sashe na IV ciwon daji na launin fata saboda ciwon peritoneal carcinomatosis za a iya bi da shi ta amfani da HIPEC tare da tiyata na cytoreductive, a wasu mutane.[114][115][116]
Radiation therapy
[gyara sashe | gyara masomin]Duk da yake haɗuwa da radiation da chemotherapy na iya zama da amfani ga ciwon daji na dubura, [45] ga wasu mutanen da ke buƙatar magani, chemoradiotherapy na iya ƙara yawan ƙwayar cuta mai tsanani, kuma ba a nuna shi don inganta yawan rayuwa ba idan aka kwatanta da radiotherapy kadai, ko da yake yana da alaƙa. tare da ƙaramar maimaitawar gida. Amfani da radiotherapy a cikin ciwon daji na hanji ba na yau da kullun ba ne saboda ji na hanji zuwa radiation. [117] Kamar yadda yake tare da chemotherapy, ana iya amfani da radiotherapy azaman neoadjuvant don matakan asibiti T3 da T4 don ciwon daji na dubura. [118] Wannan yana haifar da raguwa ko raguwar ƙwayar ƙwayar cuta, shirya shi don aikin tiyata, kuma yana rage yawan maimaitawar gida. Don ciwon daji na dubura na gida, neoadjuvant chemoradiotherapy ya zama daidaitaccen magani.[119] Bugu da ƙari, lokacin da tiyata ba zai yiwu ba, an ba da shawarar maganin radiation don zama magani mai mahimmanci game da ƙwayoyin cuta na CRC, wanda kashi 10-15% na mutanen da ke da CRC suka haɓaka. [120]
Immunotherapy
[gyara sashe | gyara masomin]Immunotherapy tare da masu hana wuraren bincike na rigakafi yana da amfani ga nau'in ciwon daji na launin fata tare da rashin daidaituwa na gyaran gyare-gyare da rashin kwanciyar hankali na microsatellite.[121][122] An amince da Pembrolizumab don ciwace-ciwacen ciwace-ciwacen ciwan CRC waɗanda ba su da ƙarancin MMR kuma sun kasa jiyya na yau da kullun. Yawancin mutanen da suka inganta, duk da haka, har yanzu suna tabarbarewa bayan watanni ko shekaru. Sauran nau'in ciwon daji na colorectal kamar na 2017 har yanzu ana nazarin su.
Kulawar jin daɗi
[gyara sashe | gyara masomin]Ana ba da shawarar kula da jin daɗi ga duk mutumin da ya sami ci gaba da ciwon daji na hanji ko kuma yana da alamun bayyanar cututtuka. [123]
Shiga cikin kulawar jin daɗi na iya zama da amfani don inganta rayuwar mutum da danginsa, ta hanyar inganta alamun cututtuka, damuwa da hana shiga asibiti. [124]
A cikin mutanen da ke fama da ciwon daji na launi maras magani, kulawar jin daɗi na iya ƙunshi hanyoyin da ke kawar da alamun cututtuka ko rikitarwa daga ciwon daji amma kada ku yi ƙoƙarin warkar da ciwon daji, don haka inganta rayuwar rayuwa . Zaɓuɓɓukan fiɗa na iya haɗawa da cirewar wasu ƙwayar cutar kansa ta hanyar tiyata marasa magani, ƙetare wani ɓangaren hanji, ko sanya stent. Ana iya la'akari da waɗannan hanyoyin don inganta alamun bayyanar cututtuka da kuma rage rikitarwa kamar zubar jini daga ciwace-ciwacen ƙwayoyi, ciwon ciki da kuma toshewar hanji. [125] Hanyoyin da ba a yi amfani da su ba na maganin bayyanar cututtuka sun haɗa da maganin radiation don rage girman ƙwayar ƙwayar cuta da magungunan ciwo. [126]
Bibiya
[gyara sashe | gyara masomin]Cibiyar Cutar Cutar Kasa ta Amurka da kuma al'adar Clinical ta Amurka ta samar da jagorori saboda masu lalata cutar ta bakin ciki.[127][128] Ana ba da shawarar tarihin likita da duba lafiyar jiki kowane watanni 3 zuwa 6 na tsawon shekaru 2, sannan kowane watanni 6 har tsawon shekaru 5. Ma'aunin matakin jini na Carcinoembryonic antigen yana bin lokaci guda, amma ana ba da shawarar kawai ga mutanen da ke da T2 ko raunuka mafi girma waɗanda ke takarar shiga tsakani. Ana iya yin la'akari da CT-scan na ƙirji, ciki da ƙashin ƙugu a kowace shekara don shekaru 3 na farko ga mutanen da ke cikin haɗarin sake dawowa (misali, waɗanda suka sami bambance-bambancen ciwace-ciwacen daji ko venous ko lymphatic mamayewa) kuma su ne 'yan takara don maganin warkewa. tiyata (da nufin warkewa). Ana iya yin ƙwanƙwaran ƙwayar ƙwayar cuta bayan shekara 1, sai dai idan ba za a iya yin shi ba a lokacin da aka fara farawa saboda yawan abin da ya hana, wanda ya kamata a yi bayan watanni 3 zuwa 6. Idan an sami polyp mai wutsiya, polyp> 1 centimita ko dysplasia mai girma, ana iya maimaita shi bayan shekaru 3, sannan a kowace shekara 5. Don wasu abubuwan da ba su da kyau, ana iya maimaita colonoscopy bayan shekara 1.
PET na yau da kullun ko duban duban dan tayi, X-rays na kirji, cikakken adadin jini ko gwajin aikin hanta ba a ba da shawarar ba.
Ga mutanen da aka yi wa tiyatar warkewa ko maganin jin daɗi (ko duka biyu) don magance ciwon daji na colorectal wanda ba na metastatic ba, ba a nuna tsananin sa ido da bin kusanci ba don samar da ƙarin fa'idodin rayuwa.
Motsa jiki
[gyara sashe | gyara masomin]Ana iya ba da shawarar motsa jiki a nan gaba azaman magani na biyu ga waɗanda suka tsira daga cutar kansa. A cikin nazarin cututtukan cututtuka, motsa jiki na iya rage takamaiman mace-mace-cancer na launin fata da kuma yawan mace-mace. Sakamako na takamaiman adadin motsa jiki da ake buƙata don lura da fa'ida sun yi karo da juna. Waɗannan bambance-bambancen na iya nuna bambance-bambance a cikin ilmin halitta na ƙari da kuma bayyana alamun halittu. Mutanen da ke da ciwace-ciwacen da ba su da maganganun CTNNB1 (β-catenin), suna shiga cikin hanyar siginar Wnt, sun buƙaci fiye da 18 Metabolic daidai (MET) sa'o'i a kowane mako, ma'auni na motsa jiki, don lura da raguwa a cikin mutuwar ciwon daji na launi. Hanyar yadda motsa jiki ke amfanar rayuwa na iya shiga cikin sa ido na rigakafi da hanyoyin kumburi. A cikin nazarin asibiti, an sami amsa mai kumburi a cikin mutanen da ke da ciwon daji na launi na II-III waɗanda suka yi makonni 2 na matsakaicin motsa jiki bayan sun kammala aikin farko. Ma'aunin Oxidative na iya zama wata hanya mai yuwuwa don amfanin da aka lura. An sami raguwa mai yawa a cikin 8-oxo-dG a cikin fitsarin mutanen da suka yi makonni 2 na matsakaicin motsa jiki bayan farfaɗo na farko. Sauran hanyoyin da za a iya amfani da su na iya haɗawa da hormone na rayuwa da jima'i-steroid hormones, ko da yake waɗannan hanyoyi na iya shiga cikin wasu nau'in ciwon daji [129][130]
Wani m biomarker iya zama p27 . Wadanda suka tsira tare da ciwace-ciwacen da suka bayyana p27 kuma sun yi girma kuma sun yi daidai da 18 MET hours a mako daya an gano sun rage yawan mutuwar ciwon daji na launin fata idan aka kwatanta da wadanda ke da kasa da 18 MET hours a mako guda. Wadanda suka tsira ba tare da maganganun p27 waɗanda suka yi motsa jiki an nuna su suna da sakamako mafi muni ba. Ƙaddamar da kunnawa ta hanyar PI3K/AKT/mTOR na iya yin bayanin asarar p27 da ma'auni mai yawa na makamashi na iya daidaita tsarin p27 don dakatar da kwayoyin cutar kansa daga rarrabuwa.
Ayyukan jiki suna ba da fa'ida ga mutanen da ke da ciwon daji mara ci gaba. An ba da rahoton haɓakawa a cikin motsa jiki na motsa jiki, gajiya mai alaƙa da ciwon daji da ingancin rayuwa mai alaƙa da lafiya a cikin ɗan gajeren lokaci. Duk da haka, ba a lura da waɗannan gyare-gyaren a matakin lafiyar kwakwalwa da ke da alaka da cututtuka, kamar damuwa da damuwa.
Hasashen
[gyara sashe | gyara masomin]Kasa da kwayoyin halitta 600 suna da alaƙa da sakamako a cikin ciwon daji mai launi. Waɗannan sun haɗa da duka nau'ikan kwayoyin da ba su da kyau, inda babban magana ke da alaƙa da sakamako mara kyau, misali girgizar zafi 70 kDa furotin 1 (HSPA1A), da kyawawan ƙwayoyin cuta inda babban magana ke da alaƙa da rayuwa mafi kyau, misali furotin mai ɗaure RNA mai ɗorewa. RBM3) .
Yawan maimaitawa
[gyara sashe | gyara masomin]Matsakaicin yawan dawowa na shekaru biyar a cikin mutanen da aikin tiyata ya yi nasara shine 5% na ciwon daji na mataki na, 12% a mataki na II da 33% a mataki na III. Duk da haka, dangane da adadin abubuwan haɗari ya tashi daga 9-22% a mataki na II da 17-44% a mataki na III.
Yawan tsira
[gyara sashe | gyara masomin]A Turai, tsawon shekaru biyar na rayuwa na ciwon daji na launin fata bai wuce 60% ba. A cikin kasashen da suka ci gaba kusan kashi uku na mutanen da ke kamuwa da cutar suna mutuwa daga cutar.
Rayuwa yana da alaƙa kai tsaye da ganowa da kuma nau'in ciwon daji da ke tattare da shi, amma gabaɗaya ba shi da kyau ga cututtukan daji masu alama, saboda galibi sun ci gaba sosai. Adadin tsira don gano matakin farko ya ninka sau biyar fiye da na ciwon daji a ƙarshen mataki. Mutanen da ke da ciwon daji wanda bai keta mucosa na mucosa ba (TNM matakin Tis, N0, M0) suna da adadin rayuwa na shekaru biyar na 100%, yayin da wadanda ke da ciwon daji na T1 (a cikin submucosal Layer) ko T2 (a cikin muscular). Layer) suna da matsakaicin adadin rayuwa na shekaru biyar kusan 90%. Waɗanda ke da ƙari mai ɓarna duk da haka ba tare da shigar kumburi ba (T3-4, N0, M0) suna da matsakaicin ƙimar rayuwa na shekaru biyar kusan 70%. Mutanen da ke da ƙananan ƙwayoyin lymph na yanki (kowane T, N1-3, M0) suna da matsakaicin matsakaicin shekaru biyar na rayuwa kusan 40%, yayin da waɗanda ke da metastases mai nisa (kowane T, kowane N, M1) suna da rashin fahimta da biyar. Rayuwar shekara ta bambanta daga <5 bisa dari zuwa kashi 31. [131][132][133][134][135] Hasashen ya dogara da abubuwa da yawa waɗanda suka haɗa da matakin lafiyar jiki na mutum, girman metastases, da ƙimar ƙari.[ana buƙatar hujja]
Duk da yake tasirin ciwon daji na launin fata akan waɗanda suka tsira ya bambanta sosai, sau da yawa za a sami buƙatar daidaitawa ga sakamakon jiki da tunani na rashin lafiya da maganinta. [136] Misali, ya zama ruwan dare ga mutane su fuskanci rashin natsuwa, [137] tabarbarewar jima'i, [138] matsaloli tare da kula da stoma [139] da kuma tsoron sake dawowar ciwon daji [140] bayan an kammala maganin farko.
Wani ingantaccen tsarin bita da aka buga a cikin 2021 ya nuna cewa akwai manyan abubuwa guda uku da ke haifar da daidaitawa ga rayuwa tare da kuma bayan cutar kansa ta launi: hanyoyin tallafi, tsananin tasirin ƙarshen jiyya da daidaitawar zamantakewa. Don haka yana da mahimmanci a ba mutane tallafin da ya dace don taimaka musu su dace da rayuwa bayan jiyya.
Epidemiology
[gyara sashe | gyara masomin]Duniya fiye da 1 Miliyoyin mutane suna kamuwa da cutar kansar launin fata a kowace shekara wanda ya haifar da mutuwar kusan 715,000 a cikin 2010 daga 490,000 a 1990. [141]
As of 2012[update], it is the second most common cause of cancer in women (9.2% of diagnoses) and the third most common in men (10.0%):16 with it being the fourth most common cause of cancer death after lung, stomach, and liver cancer. It is more common in developed than developing countries. Globally incidences vary 10-fold with highest rates in Australia, New Zealand, Europe and the US and lowest rates in Africa and South-Central Asia.[142]
Amurka
[gyara sashe | gyara masomin]Ciwon daji na launin fata shine na biyu mafi girma na sanadin kamuwa da cutar kansa da kuma mutuwa ga maza da mata a Amurka a hade. An kiyasta cutar 141,210 a cikin 2011. [143]
Dangane da farashin daga 2007 zuwa 2009, kashi 5.0% na maza da matan Amurka da aka haifa a yau za su kamu da ciwon daji a lokacin rayuwarsu. [144] Daga 2005 zuwa 2009, matsakaicin shekarun da aka gano don ciwon daji na hanji da dubura a Amurka yana da shekaru 69. Kusan 0.1% an gano su a ƙarƙashin shekaru 20; 1.1% tsakanin 20 da 34; 4.0% tsakanin 35 da 44; 13.4% tsakanin 45 da 54; 20.4% tsakanin 55 da 64; 24.0% tsakanin 65 da 74; 25.0% tsakanin 75 da 84; da 12.0% 85+ shekaru. Farashin ya fi girma a tsakanin maza (54 a cikin 100,000 cf 40 cikin 100,000 na mata).[ana buƙatar hujja]
Ƙasar Ingila
[gyara sashe | gyara masomin]A Burtaniya kimanin mutane 41,000 ne ke kamuwa da cutar kansar hanji a shekara wanda ya zama nau'i na hudu da aka fi yawan samu. [145]
Ostiraliya
[gyara sashe | gyara masomin]Ɗaya daga cikin maza 19 da ɗaya a cikin 28 mata a Ostiraliya za su kamu da ciwon daji na launin fata kafin shekaru 75; daya daga cikin maza 10 da daya a cikin 15 mata za su ci gaba da cutar ta hanyar shekaru 85. [146]
Papua New Guinea
[gyara sashe | gyara masomin]A cikin ƙasashe masu tasowa kamar Papua New Guinea da sauran Jihohin tsibirin Pacific da suka haɗa da tsibirin Solomon, cutar kansar launin fata cuta ce da ba a taɓa samunta ba a tsakanin mutane, wacce ba ta fi yawa ba idan aka kwatanta da huhu, ciki, hanta ko kansar nono. An kiyasta cewa aƙalla kashi 8 cikin 100,000 na mutane suna iya kamuwa da cutar kansar launin fata a kowace shekara, wanda ba kamar huhu ko kansar nono ba, inda na ƙarshe kawai 24 a cikin 100,000 na mata kawai. [147]
Tarihi
[gyara sashe | gyara masomin]An gano ciwon daji na dubura a cikin tsohuwar mummy ta Masar wacce ta rayu a cikin Dakhleh Oasis a lokacin Ptolemaic . [148]
Al'umma da al'adu
[gyara sashe | gyara masomin]A Amurka, watan Maris shine watan wayar da kan jama'a game da ciwon daji . [90]
Bincike
[gyara sashe | gyara masomin]Shaida ta farko ta in-vitro tana nuna kwayoyin lactic acid (misali, lactobacilli, streptococci ko lactococci ) na iya zama kariya daga ci gaba da ci gaba da ciwon daji na launi ta hanyar hanyoyi da yawa kamar aikin antioxidant, immunomodulation, inganta shirin mutuwar kwayar halitta, antiproliferative effects, da epigenetic gyare-gyare. na kwayoyin cutar daji.
Mouse model na colorectal da ciwon daji na hanji an haɓaka kuma ana amfani dashi a cikin bincike. [149][150][151]
- The Cancer Genome Atlas
- Colourectal Cancer Atlas wanda ya haɗa bayanan kwayoyin halitta da na kariya da suka shafi kyallen kansar launin launi da layin salula an haɓaka su. [152]
Hanyoyin haɗi na waje
[gyara sashe | gyara masomin]Manazarta
[gyara sashe | gyara masomin]- ↑ 1.0 1.1 1.2 "Colon Cancer Treatment (PDQ®)". NCI. May 12, 2014. Archived from the original on July 5, 2014. Retrieved June 29, 2014.
- ↑ "Defining Cancer". National Cancer Institute. September 17, 2007. Archived from the original on June 25, 2014. Retrieved June 10, 2014.
- ↑ 3.0 3.1 3.2 "General Information About Colon Cancer". NCI. May 12, 2014. Archived from the original on July 4, 2014. Retrieved June 29, 2014.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 Bosman, Frank T. (2014). "Chapter 5.5: Colorectal Cancer". In Stewart, Bernard W.; Wild, Christopher P (eds.). World Cancer Report. the International Agency for Research on Cancer, World Health Organization. pp. 392–402. ISBN 978-92-832-0443-5.
- ↑ 5.0 5.1 "Colorectal Cancer Prevention (PDQ®)". National Cancer Institute. February 27, 2014. Archived from the original on July 5, 2014. Retrieved June 29, 2014.
- ↑ Theodoratou E, Timofeeva M, Li X, Meng X, Ioannidis JP (August 2017). "Nature, Nurture, and Cancer Risks: Genetic and Nutritional Contributions to Cancer". Annual Review of Nutrition (Review). 37: 293–320. doi:10.1146/annurev-nutr-071715-051004. PMC 6143166. PMID 28826375.
- ↑ US Preventive Services Task, Force.; Davidson, KW; Barry, MJ; Mangione, CM; Cabana, M; Caughey, AB; Davis, EM; Donahue, KE; Doubeni, CA; Krist, AH; Kubik, M; Li, L; Ogedegbe, G; Owens, DK; Pbert, L; Silverstein, M; Stevermer, J; Tseng, CW; Wong, JB (18 May 2021). "Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement". JAMA. 325 (19): 1965–1977. doi:10.1001/jama.2021.6238. PMID 34003218 Check
|pmid=value (help). - ↑ US Preventive Services Task, Force.; Davidson, KW; Barry, MJ; Mangione, CM; Cabana, M; Caughey, AB; Davis, EM; Donahue, KE; Doubeni, CA; Krist, AH; Kubik, M; Li, L; Ogedegbe, G; Owens, DK; Pbert, L; Silverstein, M; Stevermer, J; Tseng, CW; Wong, JB (18 May 2021). "Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement". JAMA. 325 (19): 1965–1977. doi:10.1001/jama.2021.6238. PMID 34003218 Check
|pmid=value (help). - ↑ Thorat MA, Cuzick J (December 2013). "Role of aspirin in cancer prevention". Current Oncology Reports. 15 (6): 533–540. doi:10.1007/s11912-013-0351-3. PMID 24114189. S2CID 40187047.
- ↑ "Routine aspirin or nonsteroidal anti-inflammatory drugs for the primary prevention of colorectal cancer: recommendation statement". American Family Physician. 76 (1): 109–113. July 2007. PMID 17668849. Archived from the original on July 14, 2014.
- ↑ "SEER Stat Fact Sheets: Colon and Rectum Cancer". NCI. Archived from the original on June 24, 2014. Retrieved June 18, 2014.
- ↑ Forman, David; Ferlay, Jacques (2014). "Chapter 1.1: The global and regional burden of cancer". In Stewart, Bernard W.; Wild, Christopher P (eds.). World Cancer Report. the International Agency for Research on Cancer, World Health Organization. pp. 16–53. ISBN 978-92-832-0443-5.
- ↑ Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (November 2018). "Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries". Ca. 68 (6): 394–424. doi:10.3322/caac.21492. PMID 30207593.
- ↑ Alpers DH, Kalloo AN, Kaplowitz N, Owyang C, Powell DW (2008). Yamada T (ed.). Principles of clinical gastroenterology. Chichester, West Sussex: Wiley-Blackwell. p. 381. ISBN 978-1-4051-6910-3. Archived from the original on September 28, 2015.
- ↑ Juul JS, Hornung N, Andersen B, Laurberg S, Olesen F, Vedsted P (August 2018). "The value of using the faecal immunochemical test in general practice on patients presenting with non-alarm symptoms of colorectal cancer". British Journal of Cancer (in Turanci). 119 (4): 471–479. doi:10.1038/s41416-018-0178-7. PMC 6133998. PMID 30065255.
- ↑ 16.0 16.1 Astin M, Griffin T, Neal RD, Rose P, Hamilton W (May 2011). "The diagnostic value of symptoms for colorectal cancer in primary care: a systematic review". The British Journal of General Practice. 61 (586): e231–e243. doi:10.3399/bjgp11X572427. PMC 3080228. PMID 21619747.
- ↑ Adelstein BA, Macaskill P, Chan SF, Katelaris PH, Irwig L (May 2011). "Most bowel cancer symptoms do not indicate colorectal cancer and polyps: a systematic review". BMC Gastroenterology. 11: 65. doi:10.1186/1471-230X-11-65. PMC 3120795. PMID 21624112.
- ↑ 18.0 18.1 Watson AJ, Collins PD (2011). "Colon cancer: a civilization disorder". Digestive Diseases. 29 (2): 222–228. doi:10.1159/000323926. PMID 21734388. S2CID 7640363.
- ↑ Cunningham D, Atkin W, Lenz HJ, Lynch HT, Minsky B, Nordlinger B, Starling N (March 2010). "Colorectal cancer". Lancet. 375 (9719): 1030–1047. doi:10.1016/S0140-6736(10)60353-4. PMID 20304247. S2CID 25299272.
- ↑ "Colorectal Cancer 2011 Report: Food, Nutrition, Physical Activity, and the Prevention of Colorectal Cancer" (PDF). World Cancer Research Fund & American Institute for Cancer Research. 2011. Archived (PDF) from the original on September 9, 2016.
- ↑ Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT (July 2012). "Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy". Lancet. 380 (9838): 219–229. doi:10.1016/S0140-6736(12)61031-9. PMC 3645500. PMID 22818936.
- ↑ Fedirko V, Tramacere I, Bagnardi V, Rota M, Scotti L, Islami F, et al. (September 2011). "Alcohol drinking and colorectal cancer risk: an overall and dose-response meta-analysis of published studies". Annals of Oncology. 22 (9): 1958–1972. doi:10.1093/annonc/mdq653. PMID 21307158.
- ↑ Valtin H (November 2002). ""Drink at least eight glasses of water a day." Really? Is there scientific evidence for "8 x 8"?". American Journal of Physiology. Regulatory, Integrative and Comparative Physiology. 283 (5): R993-1004. doi:10.1152/ajpregu.00365.2002. PMID 12376390. S2CID 2256436.
- ↑ Boleij A, van Gelder MM, Swinkels DW, Tjalsma H (November 2011). "Clinical Importance of Streptococcus gallolyticus infection among colorectal cancer patients: systematic review and meta-analysis". Clinical Infectious Diseases. 53 (9): 870–878. doi:10.1093/cid/cir609. PMID 21960713.
- ↑ Jans C, Meile L, Lacroix C, Stevens MJ (July 2015). "Genomics, evolution, and molecular epidemiology of the Streptococcus bovis/Streptococcus equinus complex (SBSEC)". Infection, Genetics and Evolution. 33: 419–436. doi:10.1016/j.meegid.2014.09.017. PMID 25233845.
- ↑ Abdulamir AS, Hafidh RR, Abu Bakar F (January 2011). "The association of Streptococcus bovis/gallolyticus with colorectal tumors: the nature and the underlying mechanisms of its etiological role". Journal of Experimental & Clinical Cancer Research. 30 (1): 11. doi:10.1186/1756-9966-30-11. PMC 3032743. PMID 21247505.Samfuri:CC-notice
- ↑ Arthur JC (June 2020). "Microbiota and colorectal cancer: colibactin makes its mark". Nature Reviews. Gastroenterology & Hepatology. 17 (6): 317–318. doi:10.1038/s41575-020-0303-y. PMID 32317778. S2CID 216033220.
- ↑ Jawad N, Direkze N, Leedham SJ (2011). "Inflammatory bowel disease and colon cancer". Inflammation and Gastrointestinal Cancers. Recent Results in Cancer Research. 185. pp. 99–115. doi:10.1007/978-3-642-03503-6_6. ISBN 978-3-642-03502-9. PMID 21822822.
- ↑ Hu T, Li LF, Shen J, Zhang L, Cho CH (2015). "Chronic inflammation and colorectal cancer: the role of vascular endothelial growth factor". Current Pharmaceutical Design. 21 (21): 2960–2967. doi:10.2174/1381612821666150514104244. PMID 26004415.
- ↑ 30.0 30.1 Bye WA, Nguyen TM, Parker CE, Jairath V, East JE (September 2017). "Strategies for detecting colon cancer in patients with inflammatory bowel disease". The Cochrane Database of Systematic Reviews. 9: CD000279. doi:10.1002/14651858.cd000279.pub4. PMC 6483622. PMID 28922695.
- ↑ Juhn E, Khachemoune A (2010). "Gardner syndrome: skin manifestations, differential diagnosis and management". American Journal of Clinical Dermatology. 11 (2): 117–122. doi:10.2165/11311180-000000000-00000. PMID 20141232. S2CID 36836169.
- ↑ Half E, Bercovich D, Rozen P (October 2009). "Familial adenomatous polyposis". Orphanet Journal of Rare Diseases. 4: 22. doi:10.1186/1750-1172-4-22. PMC 2772987. PMID 19822006.
- ↑ Möslein G, Pistorius S, Saeger HD, Schackert HK (March 2003). "Preventive surgery for colon cancer in familial adenomatous polyposis and hereditary nonpolyposis colorectal cancer syndrome". Langenbeck's Archives of Surgery. 388 (1): 9–16. doi:10.1007/s00423-003-0364-8. PMID 12690475. S2CID 21385340.
- ↑ Mankaney G, Rouphael C, Burke CA (April 2020). "Serrated Polyposis Syndrome". Clinical Gastroenterology and Hepatology. 18 (4): 777–779. doi:10.1016/j.cgh.2019.09.006. PMID 31520728.
- ↑ Fan C, Younis A, Bookhout CE, Crockett SD (March 2018). "Management of Serrated Polyps of the Colon". Current Treatment Options in Gastroenterology. 16 (1): 182–202. doi:10.1007/s11938-018-0176-0. PMC 6284520. PMID 29445907.
- ↑ Bourdais R, Rousseau B, Pujals A, Boussion H, Joly C, Guillemin A, et al. (May 2017). "Polymerase proofreading domain mutations: New opportunities for immunotherapy in hypermutated colorectal cancer beyond MMR deficiency". Critical Reviews in Oncology/Hematology. 113: 242–248. doi:10.1016/j.critrevonc.2017.03.027. PMID 28427513.
- ↑ Stein U, Walther W, Arlt F, Schwabe H, Smith J, Fichtner I, et al. (January 2009). "MACC1, a newly identified key regulator of HGF-MET signaling, predicts colon cancer metastasis". Nature Medicine. 15 (1): 59–67. doi:10.1038/nm.1889. PMID 19098908. S2CID 8854895.
- ↑ Stein U (2013) MACC1 – a novel target for solid cancers. Expert Opin Ther Targets
- ↑ Schuebel KE, Chen W, Cope L, Glöckner SC, Suzuki H, Yi JM, et al. (September 2007). "Comparing the DNA hypermethylome with gene mutations in human colorectal cancer". PLOS Genetics. 3 (9): 1709–1723. doi:10.1371/journal.pgen.0030157. PMC 1988850. PMID 17892325.
- ↑ "What is the relationship between Ashkenazi Jews and colorectal cancer?". WebMD (in Turanci). Retrieved 17 October 2019.
- ↑ Ionov Y, Peinado MA, Malkhosyan S, Shibata D, Perucho M (June 1993). "Ubiquitous somatic mutations in simple repeated sequences reveal a new mechanism for colonic carcinogenesis". Nature. 363 (6429): 558–561. Bibcode:1993Natur.363..558I. doi:10.1038/363558a0. PMID 8505985. S2CID 4254940.
- ↑ Chakravarthi S, Krishnan B, Madhavan M (1999). "Apoptosis and expression of p53 in colorectal neoplasms". Indian J. Med. Res. 86 (7): 95–102.
- ↑ Abdul Khalek FJ, Gallicano GI, Mishra L (November 2010). "Colon cancer stem cells". Gastrointestinal Cancer Research (Suppl 1): S16–S23. PMC 3047031. PMID 21472043.
- ↑ Markowitz SD, Bertagnolli MM (December 2009). "Molecular origins of cancer: Molecular basis of colorectal cancer". The New England Journal of Medicine. 361 (25): 2449–2460. doi:10.1056/NEJMra0804588. PMC 2843693. PMID 20018966.
- ↑ 45.00 45.01 45.02 45.03 45.04 45.05 45.06 45.07 45.08 45.09 45.10 45.11 45.12 45.13 45.14 45.15 45.16 45.17 45.18 45.19 45.20 45.21 45.22 45.23 45.24 Empty citation (help)
- ↑ 46.0 46.1 Muzny DM, Bainbridge MN, Chang K, Dinh HH, Drummond JA, Fowler G, et al. (Cancer Genome Atlas Network) (July 2012). "Comprehensive molecular characterization of human colon and rectal cancer". Nature. 487 (7407): 330–337. Bibcode:2012Natur.487..330T. doi:10.1038/nature11252. PMC 3401966. PMID 22810696.
- ↑ Gatalica Z, Vranic S, Xiu J, Swensen J, Reddy S (July 2016). "High microsatellite instability (MSI-H) colorectal carcinoma: a brief review of predictive biomarkers in the era of personalized medicine". Familial Cancer. 15 (3): 405–412. doi:10.1007/s10689-016-9884-6. PMC 4901118. PMID 26875156.
- ↑ Hissong E, Crowe EP, Yantiss RK, Chen YT (November 2018). "Assessing colorectal cancer mismatch repair status in the modern era: a survey of current practices and re-evaluation of the role of microsatellite instability testing". Modern Pathology. 31 (11): 1756–1766. doi:10.1038/s41379-018-0094-7. PMID 29955148.
- ↑ Grady WM, Markowitz SD (March 2015). "The molecular pathogenesis of colorectal cancer and its potential application to colorectal cancer screening". Digestive Diseases and Sciences. 60 (3): 762–772. doi:10.1007/s10620-014-3444-4. PMC 4779895. PMID 25492499.
- ↑ Nguyen H, Loustaunau C, Facista A, Ramsey L, Hassounah N, Taylor H, et al. (July 2010). "Deficient Pms2, ERCC1, Ku86, CcOI in field defects during progression to colon cancer". Journal of Visualized Experiments (41): 1931. doi:10.3791/1931. PMC 3149991. PMID 20689513. 28 minute video
- ↑ Lochhead P, Chan AT, Nishihara R, Fuchs CS, Beck AH, Giovannucci E, Ogino S (January 2015). "Etiologic field effect: reappraisal of the field effect concept in cancer predisposition and progression". Modern Pathology. 28 (1): 14–29. doi:10.1038/modpathol.2014.81. PMC 4265316. PMID 24925058.
- ↑ Wilbur B, ed. (2009). The World of the Cell (7th ed.). San Francisco, C.
- ↑ Kimball's Biology Pages. Archived 2017-12-31 at the Wayback Machine "Oncogenes" Free full text
- ↑ Kanwal R, Gupta S (April 2012). "Epigenetic modifications in cancer". Clinical Genetics. 81 (4): 303–311. doi:10.1111/j.1399-0004.2011.01809.x. PMC 3590802. PMID 22082348.
- ↑ Schnekenburger M, Diederich M (March 2012). "Epigenetics Offer New Horizons for Colorectal Cancer Prevention". Current Colorectal Cancer Reports. 8 (1): 66–81. doi:10.1007/s11888-011-0116-z. PMC 3277709. PMID 22389639.
- ↑ Jacinto FV, Esteller M (July 2007). "Mutator pathways unleashed by epigenetic silencing in human cancer". Mutagenesis. 22 (4): 247–253. doi:10.1093/mutage/gem009. PMID 17412712.
- ↑ Lahtz C, Pfeifer GP (February 2011). "Epigenetic changes of DNA repair genes in cancer". Journal of Molecular Cell Biology. 3 (1): 51–58. doi:10.1093/jmcb/mjq053. PMC 3030973. PMID 21278452.
- ↑ Bernstein C, Nfonsam V, Prasad AR, Bernstein H (March 2013). "Epigenetic field defects in progression to cancer". World Journal of Gastrointestinal Oncology. 5 (3): 43–49. doi:10.4251/wjgo.v5.i3.43. PMC 3648662. PMID 23671730.
- ↑ "Colorectal Cancer". The Lecturio Medical Concept Library. Retrieved 22 July 2021.
- ↑ Coppedè F, Lopomo A, Spisni R, Migliore L (January 2014). "Genetic and epigenetic biomarkers for diagnosis, prognosis and treatment of colorectal cancer". World Journal of Gastroenterology. 20 (4): 943–956. doi:10.3748/wjg.v20.i4.943. PMC 3921546. PMID 24574767.
- ↑ Guinney J, Dienstmann R, Wang X, de Reyniès A, Schlicker A, Soneson C, et al. (November 2015). "The consensus molecular subtypes of colorectal cancer". Nature Medicine. 21 (11): 1350–1356. doi:10.1038/nm.3967. PMC 4636487. PMID 26457759.
- ↑ "Colorectal Cancer". The Lecturio Medical Concept Library. Retrieved 10 July 2021.
- ↑ "Colon, Rectosigmoid, and Rectum Equivalent Terms and Definitions C180-C189, C199, C209, (Excludes lymphoma and leukemia M9590 – M9992 and Kaposi sarcoma M9140) - Colon Solid Tumor Rules 2018. July 2019 Update" (PDF). National Cancer Institute.
- ↑ "Colorectal cancer types". Cancer Treatment Centers of America. October 4, 2018. Retrieved 2020-01-16.
- ↑ Di Como JA, Mahendraraj K, Lau CS, Chamberlain RS (October 2015). "Adenosquamous carcinoma of the colon and rectum: a population based clinical outcomes study involving 578 patients from the Surveillance Epidemiology and End Result (SEER) database (1973–2010)". Journal of the American College of Surgeons. 221 (4): 56. doi:10.1016/j.jamcollsurg.2015.08.044.
- ↑ Whiteside G, Munglani R (September 1998). "TUNEL, Hoechst and immunohistochemistry triple-labelling: an improved method for detection of apoptosis in tissue sections--an update". Brain Research. Brain Research Protocols. 3 (1): 52–53. doi:10.1016/s1385-299x(98)00020-8. PMID 9767106.
- ↑ "TNM staging of colorectal carcinoma (AJCC 8th edition)". www.pathologyoutlines.com. Retrieved 2019-02-24.
- ↑ Parkin DM, Boyd L, Walker LC (December 2011). "16. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010". British Journal of Cancer. 105 (S2): S77–S81. doi:10.1038/bjc.2011.489. PMC 3252065. PMID 22158327.
- ↑ Searke D (2006). Cancer Epidemiology and Prevention (3 ed.). Oxford University Press. p. 809. ISBN 978-0199747979. Archived from the original on September 28, 2015.
- ↑ Rennert G (2007). Cancer Prevention. Springer. p. 179. ISBN 978-3540376965. Archived from the original on October 3, 2015.
- ↑ "Colorectal Cancer Prevention Overview". National Cancer Institute (in Turanci). 1 March 2018. Retrieved 26 October 2018.
- ↑ "Cancer prevention". World Health Organization. Retrieved 27 October 2018.
- ↑ Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K (August 2016). "Body Fatness and Cancer--Viewpoint of the IARC Working Group". The New England Journal of Medicine. 375 (8): 794–798. doi:10.1056/nejmsr1606602. PMC 6754861. PMID 27557308.
- ↑ 74.0 74.1 74.2 Empty citation (help)
- ↑ 75.0 75.1 Empty citation (help)
- ↑ "Colorectal cancer".
- ↑ Willett WC, Key T, Romieu I (2014). "Chapter 2.6: Diet, obesity, and physical activity". In Stewart BW, Wild CP (eds.). World Cancer Report. the International Agency for Research on Cancer, World Health Organization. pp. 124–133. ISBN 978-92-832-0443-5.
Several large prospective cohort studies of dietary fibre and colon cancer risk have not supported an association, although an inverse relation was seen in the large European Prospective Investigation into Cancer and Nutrition (EPIC) study and a recent meta-analysis. The variation in findings from prospective studies needs to be better understood; dietary fibre is complex and heterogeneous, and the relation with colorectal cancer could differ by dietary source. (p. 127)
- ↑ Reynolds A, Mann J, Cummings J, Winter N, Mete E, Te Morenga L (February 2019). "Carbohydrate quality and human health: a series of systematic reviews and meta-analyses". Lancet. 393 (10170): 434–445. doi:10.1016/S0140-6736(18)31809-9. PMID 30638909. S2CID 58632705.
- ↑ Harriss DJ, Atkinson G, Batterham A, George K, Cable NT, Reilly T, et al. (September 2009). "Lifestyle factors and colorectal cancer risk (2): a systematic review and meta-analysis of associations with leisure-time physical activity". Colorectal Disease. 11 (7): 689–701. doi:10.1111/j.1463-1318.2009.01767.x. PMID 19207713. S2CID 8026021.
- ↑ Robsahm TE, Aagnes B, Hjartåker A, Langseth H, Bray FI, Larsen IK (November 2013). "Body mass index, physical activity, and colorectal cancer by anatomical subsites: a systematic review and meta-analysis of cohort studies". European Journal of Cancer Prevention. 22 (6): 492–505. doi:10.1097/CEJ.0b013e328360f434. PMID 23591454. S2CID 24764995.
- ↑ Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, et al. (August 2016). "Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013". BMJ. 354: i3857. doi:10.1136/bmj.i3857. PMC 4979358. PMID 27510511.
- ↑ Cooper K, Squires H, Carroll C, Papaioannou D, Booth A, Logan RF, et al. (June 2010). "Chemoprevention of colorectal cancer: systematic review and economic evaluation". Health Technology Assessment. 14 (32): 1–206. doi:10.3310/hta14320. PMID 20594533.
- ↑ Emilsson L, Holme Ø, Bretthauer M, Cook NR, Buring JE, Løberg M, et al. (January 2017). "Systematic review with meta-analysis: the comparative effectiveness of aspirin vs. screening for colorectal cancer prevention". Alimentary Pharmacology & Therapeutics. 45 (2): 193–204. doi:10.1111/apt.13857. PMID 27859394.
- ↑ Bibbins-Domingo K (June 2016). "Aspirin Use for the Primary Prevention of Cardiovascular Disease and Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement". Annals of Internal Medicine. 164 (12): 836–845. doi:10.7326/M16-0577. PMID 27064677.
- ↑ Agency for Healthcare Research and Quality. "Aspirin or Nonsteroidal Anti-inflammatory Drugs for the Primary Prevention of Colorectal Cancer". United States Department of Health & Human Services. Archived from the original on January 5, 2016.
2010/2011
- ↑ Weingarten MA, Zalmanovici A, Yaphe J (January 2008). "Dietary calcium supplementation for preventing colorectal cancer and adenomatous polyps". The Cochrane Database of Systematic Reviews. 2010 (1): CD003548. doi:10.1002/14651858.CD003548.pub4. PMC 8719254 Check
|pmc=value (help). PMID 18254022. - ↑ Ma Y, Zhang P, Wang F, Yang J, Liu Z, Qin H (October 2011). "Association between vitamin D and risk of colorectal cancer: a systematic review of prospective studies". Journal of Clinical Oncology. 29 (28): 3775–3782. doi:10.1200/JCO.2011.35.7566. PMID 21876081.
- ↑ Yin L, Grandi N, Raum E, Haug U, Arndt V, Brenner H (2011). "Meta-analysis: Serum vitamin D and colorectal adenoma risk". Preventive Medicine. 53 (1–2): 10–16. doi:10.1016/j.ypmed.2011.05.013. PMID 21672549.
- ↑ "What Can I Do to Reduce My Risk of Colorectal Cancer?". Centers for Disease Control and Prevention. April 2, 2014. Archived from the original on February 26, 2015. Retrieved March 5, 2015.
- ↑ 90.0 90.1 He J, Efron JE (2011). "Screening for colorectal cancer". Advances in Surgery. 45: 31–44. doi:10.1016/j.yasu.2011.03.006. hdl:2328/11906. PMID 21954677.
- ↑ Siegel RL, Ward EM, Jemal A (March 2012). "Trends in colorectal cancer incidence rates in the United States by tumor location and stage, 1992-2008". Cancer Epidemiology, Biomarkers & Prevention. 21 (3): 411–416. doi:10.1158/1055-9965.EPI-11-1020. PMID 22219318.
- ↑ Swartz AW, Eberth JM, Josey MJ, Strayer SM (October 2017). "Reanalysis of All-Cause Mortality in the U.S. Preventive Services Task Force 2016 Evidence Report on Colorectal Cancer Screening". Annals of Internal Medicine. 167 (8): 602–603. doi:10.7326/M17-0859. PMC 5823607. PMID 28828493.
- ↑ Hewitson P, Glasziou P, Watson E, Towler B, Irwig L (June 2008). "Cochrane systematic review of colorectal cancer screening using the fecal occult blood test (hemoccult): an update". The American Journal of Gastroenterology. 103 (6): 1541–1549. PMID 18479499.
- ↑ Lee JK, Liles EG, Bent S, Levin TR, Corley DA (February 2014). "Accuracy of fecal immunochemical tests for colorectal cancer: systematic review and meta-analysis". Annals of Internal Medicine. 160 (3): 171. doi:10.7326/M13-1484. PMC 4189821. PMID 24658694.
- ↑ "Screening for Colorectal Cancer". U.S. Preventive Services Task Force. 2008. Archived from the original on February 7, 2015. Retrieved December 19, 2011.
- ↑ Brenner H, Stock C, Hoffmeister M (April 2014). "Effect of screening sigmoidoscopy and screening colonoscopy on colorectal cancer incidence and mortality: systematic review and meta-analysis of randomised controlled trials and observational studies". BMJ. 348 (apr09 1): g2467. doi:10.1136/bmj.g2467. PMC 3980789. PMID 24922745.
- ↑ American Gastroenterological Association. "Five Things Physicians and Patients Should Question" (PDF). Choosing Wisely: An Initiative of the ABIM Foundation. Archived from the original (PDF) on August 9, 2012. Retrieved August 17, 2012.
- ↑ Winawer S, Fletcher R, Rex D, Bond J, Burt R, Ferrucci J, et al. (February 2003). "Colorectal cancer screening and surveillance: clinical guidelines and rationale-Update based on new evidence". Gastroenterology. 124 (2): 544–560. doi:10.1053/gast.2003.50044. PMID 12557158. S2CID 29354772.
- ↑ Qaseem A, Denberg TD, Hopkins RH, Humphrey LL, Levine J, Sweet DE, Shekelle P (March 2012). "Screening for colorectal cancer: a guidance statement from the American College of Physicians". Annals of Internal Medicine. 156 (5): 378–386. doi:10.7326/0003-4819-156-5-201203060-00010. PMID 22393133.
- ↑ Tang V, Boscardin WJ, Stijacic-Cenzer I, Lee SJ (April 2015). "Time to benefit for colorectal cancer screening: survival meta-analysis of flexible sigmoidoscopy trials". BMJ. 350: h1662. doi:10.1136/bmj.h1662. PMC 4399600. PMID 25881903.
- ↑ "NHS Bowel Cancer Screening Programme". cancerscreening.nhs.uk. Archived from the original on November 29, 2014.
- ↑ "Home – Bowel Cancer Australia". bowelcanceraustralia.org. Archived from the original on December 24, 2014.
- ↑ "Bevolkingsonderzoek darmkanker". rivm.nl. Archived from the original on December 17, 2014.
- ↑ Tepus M, Yau TO (July 2020). "Non-Invasive Colorectal Cancer Screening: An Overview". Gastrointestinal Tumors. 7 (3): 62–73. doi:10.1159/000507701. PMC 7445682. PMID 32903904.
- ↑ Stein A, Atanackovic D, Bokemeyer C (September 2011). "Current standards and new trends in the primary treatment of colorectal cancer". European Journal of Cancer. 47 (Suppl 3): S312–S314. doi:10.1016/S0959-8049(11)70183-6. PMID 21943995.
- ↑ Chiorean EG, Nandakumar G, Fadelu T, Temin S, Alarcon-Rozas AE, Bejarano S, et al. (March 2020). "Treatment of Patients With Late-Stage Colorectal Cancer: ASCO Resource-Stratified Guideline". JCO Global Oncology. 6 (6): 414–438. doi:10.1200/JGO.19.00367. PMC 7124947. PMID 32150483.
- ↑ McCarthy K, Pearson K, Fulton R, Hewitt J, et al. (Cochrane Colorectal Cancer Group) (December 2012). "Pre-operative chemoradiation for non-metastatic locally advanced rectal cancer". The Cochrane Database of Systematic Reviews. 12: CD008368. doi:10.1002/14651858.CD008368.pub2. PMID 23235660.
- ↑ "Colorectal (Colon) Cancer". Cleveland Clinic. Retrieved 9 July 2021.
- ↑ Böckelman C, Engelmann BE, Kaprio T, Hansen TF, Glimelius B (January 2015). "Risk of recurrence in patients with colon cancer stage II and III: a systematic review and meta-analysis of recent literature". Acta Oncologica. 54 (1): 5–16. doi:10.3109/0284186x.2014.975839. PMID 25430983.
- ↑ "Chemotherapy of metastatic colorectal cancer". Prescrire International. 19 (109): 219–224. October 2010. PMID 21180382.
- ↑ Fakih MG (June 2015). "Metastatic colorectal cancer: current state and future directions". Journal of Clinical Oncology. 33 (16): 1809–1824. doi:10.1200/JCO.2014.59.7633. PMID 25918280.
- ↑ Shaib W, Mahajan R, El-Rayes B (September 2013). "Markers of resistance to anti-EGFR therapy in colorectal cancer". Journal of Gastrointestinal Oncology. 4 (3): 308–318. doi:10.3978/j.issn.2078-6891.2013.029. PMC 3712296. PMID 23997942.
- ↑ Yau TO (October 2019). "Precision treatment in colorectal cancer: Now and the future". JGH Open. 3 (5): 361–369. doi:10.1002/jgh3.12153. PMC 6788378. PMID 31633039.
- ↑ Sugarbaker PH, Van der Speeten K (February 2016). "Surgical technology and pharmacology of hyperthermic perioperative chemotherapy". Journal of Gastrointestinal Oncology. 7 (1): 29–44. doi:10.3978/j.issn.2078-6891.2015.105. PMC 4754302. PMID 26941982.
- ↑ Segura-Sampedro JJ, Morales-Soriano R (August 2020). "Prophylactic HIPEC with oxaliplatin might be of benefit in T4 and perforated colon cancer: another possible interpretation of the COLOPEC results". Revista Espanola de Enfermedades Digestivas. 112 (8): 666. doi:10.17235/reed.2020.6755/2019. PMID 32686435.
- ↑ Esquivel J, Sticca R, Sugarbaker P, Levine E, Yan TD, Alexander R, et al. (January 2007). "Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in the management of peritoneal surface malignancies of colonic origin: a consensus statement. Society of Surgical Oncology". Annals of Surgical Oncology. 14 (1): 128–133. doi:10.1245/s10434-006-9185-7. PMID 17072675. S2CID 21282326.
- ↑ DeVita VT, Lawrence TS, Rosenberg SA (2008). DeVita, Hellman, and Rosenberg's Cancer: Principles & Practice of Oncology. Lippincott Williams & Wilkins. pp. 1258–. ISBN 978-0-7817-7207-5.
- ↑ Feeney G, Sehgal R, Sheehan M, Hogan A, Regan M, Joyce M, Kerin M (September 2019). "Neoadjuvant radiotherapy for rectal cancer management". World Journal of Gastroenterology. 25 (33): 4850–4869. doi:10.3748/wjg.v25.i33.4850. PMC 6737323. PMID 31543678.
- ↑ Li Y, Wang J, Ma X, Tan L, Yan Y, Xue C, et al. (2016). "A Review of Neoadjuvant Chemoradiotherapy for Locally Advanced Rectal Cancer". International Journal of Biological Sciences. 12 (8): 1022–1031. doi:10.7150/ijbs.15438. PMC 4971740. PMID 27489505.
- ↑ Cao C, Wang D, Tian DH, Wilson-Smith A, Huang J, Rimner A (December 2019). "A systematic review and meta-analysis of stereotactic body radiation therapy for colorectal pulmonary metastases". Journal of Thoracic Disease. 11 (12): 5187–5198. doi:10.21037/jtd.2019.12.12. PMC 6988072. PMID 32030236.
- ↑ Boland PM, Ma WW (May 2017). "Immunotherapy for Colorectal Cancer". Cancers. 9 (5): 50. doi:10.3390/cancers9050050. PMC 5447960. PMID 28492495.
- ↑ Syn NL, Teng MW, Mok TS, Soo RA (December 2017). "De-novo and acquired resistance to immune checkpoint targeting". The Lancet. Oncology. 18 (12): e731–e741. doi:10.1016/s1470-2045(17)30607-1. PMID 29208439.
- ↑ "ASCO Provisional Clinical Opinion: The Integration of Palliative Care into Standard Oncology Care". ASCO. Archived from the original on August 21, 2014. Retrieved 20 August 2014.
- ↑ Higginson IJ, Evans CJ (Sep–Oct 2010). "What is the evidence that palliative care teams improve outcomes for cancer patients and their families?". Cancer Journal. 16 (5): 423–435. doi:10.1097/PPO.0b013e3181f684e5. PMID 20890138. S2CID 39881122.
- ↑ Wasserberg N, Kaufman HS (December 2007). "Palliation of colorectal cancer". Surgical Oncology. 16 (4): 299–310. doi:10.1016/j.suronc.2007.08.008. PMID 17913495.
- ↑ Amersi F, Stamos MJ, Ko CY (July 2004). "Palliative care for colorectal cancer". Surgical Oncology Clinics of North America. 13 (3): 467–477. doi:10.1016/j.soc.2004.03.002. PMID 15236729.
- ↑ "National Comprehensive Cancer Network" (PDF). nccn.org. Archived (PDF) from the original on March 25, 2009.
- ↑ Desch CE, Benson AB, Somerfield MR, Flynn PJ, Krause C, Loprinzi CL, et al. (November 2005). "Colorectal cancer surveillance: 2005 update of an American Society of Clinical Oncology practice guideline". Journal of Clinical Oncology. 23 (33): 8512–8519. doi:10.1200/JCO.2005.04.0063. PMID 16260687.
- ↑ Betof AS, Dewhirst MW, Jones LW (March 2013). "Effects and potential mechanisms of exercise training on cancer progression: a translational perspective". Brain, Behavior, and Immunity. 30 (Suppl): S75–S87. doi:10.1016/j.bbi.2012.05.001. PMC 3638811. PMID 22610066.
- ↑ Ballard-Barbash R, Friedenreich CM, Courneya KS, Siddiqi SM, McTiernan A, Alfano CM (June 2012). "Physical activity, biomarkers, and disease outcomes in cancer survivors: a systematic review". Journal of the National Cancer Institute. 104 (11): 815–840. doi:10.1093/jnci/djs207. PMC 3465697. PMID 22570317.
- ↑ Zacharakis M, Xynos ID, Lazaris A, Smaro T, Kosmas C, Dokou A, et al. (February 2010). "Predictors of survival in stage IV metastatic colorectal cancer". Anticancer Research. 30 (2): 653–660. PMID 20332485.
- ↑ Box 3-1, Page 107 in: Agabegi ED, Agabegi SS (2008). Step-Up to Medicine (Step-Up Series). Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 978-0-7817-7153-5.
- ↑ Hong Y (30 June 2020). "Clinical study of colorectal cancer operation: Survival analysis". Korean Journal of Clinical Oncology 2020. 16: 3–8. doi:10.14216/kjco.20002. Retrieved 9 May 2021.
- ↑ "Five-Year Survival Rates". National Cancer Institute. Retrieved 9 May 2021.
- ↑ Xu Z, Becerra AZ, Fleming FJ, Aquina CT, Dolan JG, Monson JR, et al. (October 2019). "Treatments for Stage IV Colon Cancer and Overall Survival". The Journal of Surgical Research. 242: 47–54. doi:10.1016/j.jss.2019.04.034. PMID 31071604. S2CID 149443256.
- ↑ Drageset S, Lindstrøm TC, Underlid K (April 2016). ""I just have to move on": Women's coping experiences and reflections following their first year after primary breast cancer surgery". European Journal of Oncology Nursing (in English). 21: 205–211. doi:10.1016/j.ejon.2015.10.005. PMID 26521054.CS1 maint: unrecognized language (link)
- ↑ Restivo A, Zorcolo L, D'Alia G, Cocco F, Cossu A, Scintu F, Casula G (February 2016). "Risk of complications and long-term functional alterations after local excision of rectal tumors with transanal endoscopic microsurgery (TEM)". International Journal of Colorectal Disease. 31 (2): 257–266. doi:10.1007/s00384-015-2371-y. PMID 26298182. S2CID 29087556.
- ↑ Bregendahl S, Emmertsen KJ, Lindegaard JC, Laurberg S (January 2015). "Urinary and sexual dysfunction in women after resection with and without preoperative radiotherapy for rectal cancer: a population-based cross-sectional study". Colorectal Disease. 17 (1): 26–37. doi:10.1111/codi.12758. PMID 25156386. S2CID 42069306.
- ↑ Ramirez M, McMullen C, Grant M, Altschuler A, Hornbrook MC, Krouse RS (December 2009). "Figuring out sex in a reconfigured body: experiences of female colorectal cancer survivors with ostomies". Women & Health. 49 (8): 608–624. doi:10.1080/03630240903496093. PMC 2836795. PMID 20183104.
- ↑ Steele N, Haigh R, Knowles G, Mackean M (September 2007). "Carcinoembryonic antigen (CEA) testing in colorectal cancer follow up: what do patients think?". Postgraduate Medical Journal. 83 (983): 612–614. doi:10.1136/pgmj.2007.059634. PMC 2600007. PMID 17823231.
- ↑ Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–2128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMID 23245604. S2CID 1541253.
- ↑ Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010). "Colorectal Cancer Incidence, Mortality and Prevalence Worldwide in 2008 – Summary". Archived from the original on October 17, 2012.; "GLOBOCAN 2008 v2.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10". Lyon, France: International Agency for Research on Cancer. Archived from the original on May 8, 2011.
- ↑ Redmond J, Vanderpool R, McClung R (2012). "Effectively Communicating Colorectal Cancer Screening Information to Primary Care Providers: Application for State, Tribe or Territory Comprehensive Cancer Control Coalitions". American Journal of Health Education. 43 (4): 194–201. doi:10.1080/19325037.2012.10599235. PMC 4770578. PMID 26937262.
- ↑ Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Altekruse SF, Kosary CL, Ruhl J, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Chen HS, Feuer EJ, Cronin KA. SEER Cancer Statistics Review, 1975–2009 (Vintage 2009 Populations). Bethesda, MD: National Cancer Institute. Archived from the original on September 3, 2012. Based on November 2011 SEER data submission, posted to the SEER web site, 2012.
- ↑ "Bowel cancer | About bowel cancer | Cancer Research UK". www.cancerresearchuk.org (in Turanci). Archived from the original on March 9, 2017. Retrieved May 12, 2017.
- ↑ Cancer in Australia: an Overview, 2014. Cancer series No 90. Cat. No. CAN 88. Canberra: Australian Institute of Health and Welfare. 2014. ISBN 978-1-74249-677-1.
- ↑ Cancer in Papua New Guinea: an Overview, 2016. Cancer series No. 176. Cat. No. CAN 88. Papua New Guinea Department of Health. 2016.
- ↑ Rehemtulla A (December 2010). "Dinosaurs and ancient civilizations: reflections on the treatment of cancer". Neoplasia. 12 (12): 957–968. doi:10.1593/neo.101588. PMC 3003131. PMID 21170260.
- ↑ Golovko D, Kedrin D, Yilmaz ÖH, Roper J (2015). "Colorectal cancer models for novel drug discovery". Expert Opinion on Drug Discovery. 10 (11): 1217–1229. doi:10.1517/17460441.2015.1079618. PMC 4872297. PMID 26295972.
- ↑ Oh BY, Hong HK, Lee WY, Cho YB (February 2017). "Animal models of colorectal cancer with liver metastasis". Cancer Letters. 387: 114–120. doi:10.1016/j.canlet.2016.01.048. PMID 26850374.
- ↑ Evans JP, Sutton PA, Winiarski BK, Fenwick SW, Malik HZ, Vimalachandran D, et al. (February 2016). "From mice to men: Murine models of colorectal cancer for use in translational research". Critical Reviews in Oncology/Hematology. 98: 94–105. doi:10.1016/j.critrevonc.2015.10.009. PMID 26558688.
- ↑ "Colorectal Cancer Atlas". Archived from the original on January 13, 2016.
- CS1 errors: PMID
- CS1 Turanci-language sources (en)
- Pages with empty citations
- Webarchive template wayback links
- CS1 errors: PMC
- CS1 maint: unrecognized language
- All articles with unsourced statements
- Articles with unsourced statements from May 2021
- Articles with invalid date parameter in template
- Articles containing potentially dated statements from 2012
- All articles containing potentially dated statements
- Cutar daji
