Ciwon daji na hanta
| Ciwon daji na hanta | |
|---|---|
 | |
| Description (en) | |
| Iri |
liver tumor (en) cuta |
| Specialty (en) | oncology |
| Sanadi |
Cirrhosis aflatoxins (en) |
| Symptoms and signs (en) |
Shawara, Ciwon ciki, weight loss (en) hepatomegaly (en) |
| Physical examination (en) |
computed tomography (en) blood test (en) |
| Identifier (en) | |
| ICD-10-CM | C22.9 da C22.0 |
| ICD-9-CM | 155.0 da 155.2 |
| OMIM | 114550 |
| Disease Ontology ID | DOID:3571 |
Ciwon daji na hanta, wanda kuma aka sani da ciwon hanta, shi ne kansar da ke farawa a cikin hanta.[1] Ciwon daji wanda ya yadu daga wani wuri zuwa hanta, wanda aka sani da hanta metastasis, ya fi kowa fiye da wanda ke farawa a cikin hanta.[2] Alamun ciwon daji na hanta na iya hadawa da dunkule ko ciwo a gefen dama a kasan hakarkarin hakarkari, kumburin ciki, fata mai launin rawaya, sauki mai laushi, asarar nauyi da rauni.[1]
Babban abin da ke haifar da ciwon hanta shine cirrhosis saboda hepatitis B, hepatitis C ko barasa.[3] Sauran abubuwan da ke haifar da cutar sun hada da aflatoxin, cutar hanta mai kitse ba ta barasa da murar hanta ba.[2] Mafi yawan nau'o'in ciwon daji na hanta (HCC), wanda ke da kashi 80% na lokuta, da cholangiocarcinoma. Nau'ukan da ba su da yawa sun hada da mucinous cystic neoplasm da intraductal papillary biliary neoplasm.[2] Ana iya samun goyan bayan ganewar asali ta gwajin jini da hoton likita, tare da tabbatarwa ta hanyar biopsy nama.[1]
Kokarin rigakafin sun hada da allurar rigakafin cutar hanta ta B da kuma kula da wadanda suka kamu da cutar hanta ta B ko C.[2] Ana ba da shawarar yin gwaji a cikin masu fama da cutar hanta.[2] Zabubbukan jiyya na iya hadawa da tiyata, maganin da aka yi niyya da kuma maganin radiation.[1] A wasu lokuta, ana iya amfani da farfagandar zubar da ciki, maganin kumburin ciki ko dashen hanta.[1] Ana iya bin kananan kullu a cikin hanta a hankali.[1]
Ciwon daji na hanta na farko shine na shida a yawan ciwon daji a duniya (6%) kuma na biyun da ke haifar da mutuwa daga cutar kansa (9%).[2][4] A cikin 2018, ya faru a cikin mutane 841,000 kuma ya yi sanadiyar mutuwar 782,000.[5] A cikin 2015, mutane 263,000 sun mutu daga cutar kansar hanta ta hanyar hanta, 245,000 ga barasa da 167,000 zuwa hepatitis C.[6] Yawan ciwon hanta ya fi girma a inda cutar hepatitis B da C ke da yawa, ciki har da Asiya da Afirka kudu da Sahara.[2] Maza sun fi kamuwa da HCC fiye da mata.[2] Ganowa ya fi yawa a tsakanin masu shekaru 55 zuwa 65.[7] Adadin rayuwa na shekaru biyar shine 18.4 % a Amurka,[7] da 40.4% a Japan.[8] Kalmar "hepatic" ta fito ne daga kalmar Helenanci hêpar, ma'ana "hanta".[9]
Ganin cewa akwai dalilai daban-daban na cutar kansar hanta, akwai hanyoyi da yawa don rigakafin cutar kansar hanta. Wadannan yunkurin sun hada da rigakafi da cutar hanta B, maganin hanta, maganin hanta na C, rage yawan amfani da barasa, rage kamuwa da aflatoxin a aikin gona, da kula da kiba da ciwon sukari . Ana ba da shawarar dubawa ga wadanda ke da cututtukan hanta na yau da kullun . Misali, ana ba da shawarar cewa mutanen da ke da ciwon hanta na yau da kullun wadanda ke cikin hadarin kamuwa da cutar sankarar hanta a kowane watanni 6 ta amfani da hoton duban dan tayi.
Domin ciwon hanta laima ce ga nau'ikan ciwon daji da yawa, alamu da alamun sun dogara ne akan irin nau'in ciwon daji. Alamun na iya zama m da fadi. Cholangiocarcinoma yana hade da gumi, jaundice, ciwon ciki, asarar nauyi da haɓaka hanta . [9] Cutar sankarau tana hade da ciwon ciki, ciwon ciki, emesis, anemia, ciwon baya, jaundice, itching, asarar nauyi da zazzabi .[10]
Zabubbukan magani na iya hadawa da tiyata, maganin da aka yi niyya da kuma maganin radiation . A wasu lokuta, ana iya amfani da farfagandar zubar da jini, embolization therapy ko dashen hanta .
Dalilai da abubuwan hadari
[gyara sashe | gyara masomin]Kamuwa da cuta
[gyara sashe | gyara masomin]
Kamuwa da cuta tare da cutar hanta ta C (HCV) ko cutar Hepatitis B (HBV) ita ce babban abin da ke haifar da ciwon hanta a duniya a yau, wanda ke da kashi 80% na HCC.[11][12][13] Maza masu HCV ko HBV na yau da kullum sun fi kamuwa da HCC fiye da matan da ke da HCV ko HBV; duk da haka, ba a san dalilan wannan bambancin jinsi ba. Cutar HBV kuma tana da alaƙa da cholangiocarcinoma . [14] Matsayin kwayoyin cuta banda HCV ko HBV a cikin ciwon hanta ba shi da kyau sosai, kodayake akwai wasu shaidun cewa kamuwa da cutar HBV da cutar hanta D na iya kara hadarin HCC.[15]
HBV da HCV na iya haifar da HCC, saboda wadannan kwayoyin cuta suna haifar da kumburi mai yawa, fibrosis, kuma cirrhosis na ƙarshe yana faruwa a cikin hanta.[16] Bugu da kari, yawancin canje-canjen kwayoyin halitta da na epigenetic suna samuwa a cikin kwayoyin hanta a lokacin HCV da HBV, wanda shine babban mahimmanci wajen samar da ciwace-ciwacen hanta. Kwayoyin cuta suna haifar da mummunan canje-canje a cikin sel ta hanyar canza kwayar halitta methylation, da tasiri akan maganganun kwayoyin halitta, da hadaka ko murkushe hanyoyin watsa siginar salula. Ta hanyar yin wannan, kwayoyin cuta na iya hana kwayoyin cuta yin tsarin tsarin mutuwar kwayar halitta ( apoptosis ) kuma suna hadaka kwafi da juriya.[17]
HBV da HCV suma suna haifar da muggan canje-canje ta hanyar haifar da lalacewar DNA da rashin zaman lafiyar kwayoyin halitta . Wannan shine ta hanyar kirkirar nau'in oxygen mai amsawa, sunadaran sunadaran da ke tsoma baki tare da gyaran enzymes na DNA, kuma HCV yana haifar da kunna enzyme mutator .[18][19]
Cirrhosis
[gyara sashe | gyara masomin]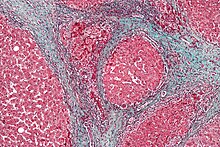
Baya ga cirrhosis mai alaka da kwayoyin cuta da aka bayyana a sama, wasu abubuwan da ke haifar da cirrhosis na iya haifar da HCC. Shan barasa yana da alaka da hadarin HCC, kuma hadarin ya fi girma a cikin mutane masu hanta cirrhotic mai haifar da barasa.[20] Akwai yan cututtuka wadanda aka san suna haifar da cirrhosis kuma suna haifar da ciwon daji, gami da hemochromatosis na gado da kuma cirrhosis na biliary na farko .[21]
Aflatoxin
[gyara sashe | gyara masomin]Bayyanar Aflatoxin na iya haifar da hadakar HCC.[22] Aflatoxins rukuni ne na sinadarai da fungi Aspergillus flavus (sunan ya fito daga A. flavus toxin) da A. parasiticus . Gurbatar abinci daga fungi yana haifar da shiga cikin sinadarai, wadanda suke da guba sosai ga hanta. Abubuwan abinci na yau da kullun da suka gurbata da guba sune hatsi, gyada, da sauran kayan lambu. Adadin (dose) da tsawon lokacin (lokacin) da mutum ke hulda da aflatoxin yana da alaƙa da HCC. Gurbacewar abinci ya zama ruwan dare a Afirka, Kudu maso Gabashin Asiya, da China. Hanyar da aflatoxins ke haifar da ciwon daji shine ta hanyar maye gurbi da sauye-sauye na epigenetic . Aflatoxins suna haifar da nau'in maye gurbi,[23][24] ciki har da a cikin kwayar cutar ciwon tumor p53, wanda shine maye gurbin da ake gani a yawancin nau'in ciwon daji. Maye gurbi a cikin p53, mai yiwuwa tare da wasu sauye-sauyen da ke haifar da aflatoxin da sauye-sauye na epigenetic, [25] yana iya zama sanadin gama gari na aflatoxin-induced carcinogenesis .
steatohepatitis mara barasa (NASH) da kuma hanta mai kitse (NAFL)
[gyara sashe | gyara masomin]NASH da NAFL an fara kiran su da haɗari ga ciwon hanta, musamman HCC.[26] A cikin 'yan shekarun nan, an sami karuwar dashen hanta ga HCC wanda aka danganta ga NASH. Ana bukatar karin bincike a wannan yanki da NASH/NAFL.
Sauran abubuwan haɗari a cikin manya
[gyara sashe | gyara masomin]- High grade dysplastic nodules su ne precancerous raunuka na hanta. A cikin shekaru biyu, akwai hadarin ciwon daji da ke tasowa daga wadannan nodules na 30-40%.[27]
- Kiba da ciwo na rayuwa sun fito a matsayin muhimmiyar hadari, saboda suna iya haifar da steatohepatitis .[28]
- Ciwon sukari yana kara hadarin HCC.
- Shan taba yana kara hadari ga HCC idan aka kwatanta da masu shan taba da masu shan taba a baya.
- Akwai kusan kashi 5-10% na hadarin rayuwa na cholangiocarcinoma a cikin mutanen da ke da sclerosing cholangitis na farko .[29]
- Kwayar cutar hanta yana kara hadarin cholangiocarcinoma, kuma wannan shine dalilin da yasa Thailand ke da yawan adadin wannan ciwon daji. [30]
- Choledochal cysts, cutar Caroli, da fibrosis na hanta na hanta suna hade da ci gaban cholangiocarcinoma.[31]
- Halin kwayoyin halitta : hemochromatosis na gado wanda ba a kula da shi ba, rashi na alpha-1-antitrypsin, cututtuka na ajiya na glycogen, porphyria cutanea tarda, cutar Wilson, tyrosinemia duk an danganta su da ci gaban HCC.
- Kwayar hana daukar ciki ta baka : Babu isassun shaida don lakabi maganin hana haihuwa a matsayin abin hadari. Duk da haka, binciken da aka yi kwanan nan ya gano cewa shan maganin hana haihuwa na baki fiye da shekaru 5 yana da alaka da HCC.
Yara
[gyara sashe | gyara masomin]Ciwon hanta na yara ba a saba gani ba.[32] Nau'in ciwon daji na hanta da aka fi gani a cikin yara sune hepatoblastoma, hepatocellular carcinoma, embryomal sarcoma na hanta, jarirai choriocarcinoma na hanta, da biliary rhabdomyosarcoma. Kara hadarin ciwon hanta a cikin yara na iya haifar da ciwon Beckwith-Wiedemann (wanda ke da alaka da hepatoblastoma),[33][34] iyali adenomatous polyposis (wanda ke hade da hepatoblastoma), kananan nauyin haihuwa (wanda ke hade da hepatoblastoma),[35] Ci gaban iyali cholestasis intrahepatic cholestasis (wanda ke hade da HCC)[36] Trisomy 18 (wanda ke hade da hepatoblastoma).
Rabewa
[gyara sashe | gyara masomin]Ciwon daji na hanta zai iya fitowa daga parenchyma na hanta da kuma wasu sifofi a cikin hanta kamar su bile duct, jini da kwayoyin rigakafi . Akwai kananan nau'ikan ciwon daji na hanta, wadanda aka fi sani da su a kasa.
Manazarta
[gyara sashe | gyara masomin]- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 "Adult Primary Liver Cancer Treatment (PDQ®)–Patient Version". NCI. 6 July 2016. Archived from the original on 2 October 2016. Retrieved 29 September 2016.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 5.6. ISBN 978-9283204299.
- ↑ GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ↑ World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 1.1. ISBN 978-9283204299.
- ↑ Bray, F; Ferlay, J; Soerjomataram, I; Siegel, RL; Torre, LA; Jemal, A (November 2018). "Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries". CA: A Cancer Journal for Clinicians. 68 (6): 394–424. doi:10.3322/caac.21492. PMID 30207593.
- ↑ GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ↑ 7.0 7.1 "SEER Stat Fact Sheets: Liver and Intrahepatic Bile Duct Cancer". NCI. Archived from the original on 2017-07-28.
- ↑ "がん診療連携拠点病院等院内がん登録生存率集計:[国立がん研究センター がん登録・統計]". ganjoho.jp. Retrieved 2 February 2020.
- ↑ 9.0 9.1 "Hepato- Etymology". dictionary.com. Archived from the original on 10 October 2015. Retrieved 24 October 2015.
- ↑ "Liver tumors in Children". Boston Children's Hospital. Archived from the original on 2011-06-04.
- ↑ Arzumanyan, A; Reis, HM; Feitelson, MA (February 2013). "Pathogenic mechanisms in HBV- and HCV-associated hepatocellular carcinoma". Nature Reviews. Cancer. 13 (2): 123–35. doi:10.1038/nrc3449. PMID 23344543. S2CID 29447705.
- ↑ Rosen, HR (Jun 23, 2011). "Clinical practice. Chronic hepatitis C infection". The New England Journal of Medicine. 364 (25): 2429–38. doi:10.1056/NEJMcp1006613. PMID 21696309. S2CID 19755395.
- ↑ "General Information About Adult Primary Liver Cancer". National Cancer Instituteb. 1980-01-01. Archived from the original on 2 January 2013. Retrieved 13 January 2013.
- ↑ Ralphs, S; Khan, SA (May 2013). "The role of the hepatitis viruses in cholangiocarcinoma". Journal of Viral Hepatitis. 20 (5): 297–305. doi:10.1111/jvh.12093. PMID 23565610. S2CID 44318080.
- ↑ Kew, MC (March 2013). "Hepatitis viruses (other than hepatitis B and C viruses) as causes of hepatocellular carcinoma: an update". Journal of Viral Hepatitis. 20 (3): 149–57. doi:10.1111/jvh.12043. PMID 23383653. S2CID 206164005.
- ↑ Dooley, James; Lok, Anna S. F.; Garcia-Tsao, Guadalupe; Pinzani, Massimo (eds.). Sherlock's diseases of the liver and biliary system. ISBN 978-1-119-23756-3. OCLC 1019837000.
- ↑ Jeong, SW; Jang, JY; Chung, RT (December 2012). "Hepatitis C virus and hepatocarcinogenesis". Clinical and Molecular Hepatology. 18 (4): 347–56. doi:10.3350/cmh.2012.18.4.347. PMC 3540370. PMID 23323249.
- ↑ Takeda H, Takai A, Inuzuka T, Marusawa H (2017). "Genetic basis of hepatitis virus-associated hepatocellular carcinoma: linkage between infection, inflammation, and tumorigenesis". J. Gastroenterol. 52 (1): 26–38. doi:10.1007/s00535-016-1273-2. PMID 27714455.
- ↑ Yang, SF; Chang, CW; Wei, RJ; Shiue, YL; Wang, SN; Yeh, YT (2014). "Involvement of DNA damage response pathways in hepatocellular carcinoma". BioMed Research International. 2014: 153867. doi:10.1155/2014/153867. PMC 4022277. PMID 24877058.
- ↑ Du, Xuan; Hidayat, Khemayanto; Shi, Bi-Min (30 June 2017). "Abdominal obesity and gastroesophageal cancer risk: systematic review and meta-analysis of prospective studies". Bioscience Reports. 37 (3): BSR20160474. doi:10.1042/BSR20160474. PMC 5426287. PMID 28336766.
- ↑ Fattovich, G; Stroffolini, T; Zagni, I; Donato, F (November 2004). "Hepatocellular carcinoma in cirrhosis: incidence and risk factors". Gastroenterology. 127 (5 Suppl 1): S35–50. doi:10.1053/j.gastro.2004.09.014. PMID 15508101.
- ↑ Balogh, Julius; Victor, David; Asham, Emad H; Burroughs, Sherilyn Gordon; Boktour, Maha; Saharia, Ashish; Li, Xian; Ghobrial, Mark; Monsour, Howard (October 2016). "Hepatocellular carcinoma: a review". Journal of Hepatocellular Carcinoma (in Turanci). 3: 41–53. doi:10.2147/JHC.S61146. ISSN 2253-5969. PMC 5063561. PMID 27785449.
- ↑ Smela ME, Currier SS, Bailey EA, Essigmann JM (April 2001). "The chemistry and biology of aflatoxin B(1): from mutational spectrometry to carcinogenesis". Carcinogenesis. 22 (4): 535–45. doi:10.1093/carcin/22.4.535. PMID 11285186.
- ↑ Perduca V, Omichessan H, Baglietto L, Severi G (January 2018). "Mutational and epigenetic signatures in cancer tissue linked to environmental exposures and lifestyle". Curr Opin Oncol. 30 (1): 61–67. doi:10.1097/CCO.0000000000000418. PMID 29076965. S2CID 20842446.
- ↑ Empty citation (help)
- ↑ "Liver (Hepatocellular) Cancer Prevention (PDQ®)–Health Professional Version - National Cancer Institute". www.cancer.gov (in Turanci). 2005-05-23. Retrieved 2021-02-23.
- ↑ Di Tommaso, L; Sangiovanni, A; Borzio, M; Park, YN; Farinati, F; Roncalli, M (April 2013). "Advanced precancerous lesions in the liver". Best Practice & Research. Clinical Gastroenterology. 27 (2): 269–84. doi:10.1016/j.bpg.2013.03.015. PMID 23809245.
- ↑ Chuang SC, La Vecchia C, Boffetta P (Dec 1, 2009). "Liver cancer: descriptive epidemiology and risk factors other than HBV and HCV infection". Cancer Letters. 286 (1): 9–14. doi:10.1016/j.canlet.2008.10.040. PMID 19091458.
- ↑ Razumilava, N; Gores, GJ (January 2013). "Classification, diagnosis, and management of cholangiocarcinoma". Clinical Gastroenterology and Hepatology. 11 (1): 13–21.e1, quiz e3–4. doi:10.1016/j.cgh.2012.09.009. PMC 3596004. PMID 22982100.
- ↑ Jemal, A; Bray, F; Center, MM; Ferlay, J; Ward, E; Forman, D (Mar–Apr 2011). "Global cancer statistics". CA: A Cancer Journal for Clinicians. 61 (2): 69–90. doi:10.3322/caac.20107. PMID 21296855. S2CID 30500384.
- ↑ Patel, Tushar (April 2011). "Cholangiocarcinoma—controversies and challenges". Nature Reviews. Gastroenterology & Hepatology. 8 (4): 189–200. doi:10.1038/nrgastro.2011.20. ISSN 1759-5045. PMC 3888819. PMID 21460876.
- ↑ "Childhood Liver Cancer Treatment (PDQ®)–Health Professional Version - National Cancer Institute". www.cancer.gov (in Turanci). 2020-11-27. Retrieved 2021-02-25.
- ↑ DeBaun, MR; Tucker, MA (March 1998). "Risk of cancer during the first four years of life in children from The Beckwith-Wiedemann Syndrome Registry". The Journal of Pediatrics. 132 (3 Pt 1): 398–400. doi:10.1016/S0022-3476(98)70008-3. PMID 9544889.
- ↑ Spector, LG; Birch, J (November 2012). "The epidemiology of hepatoblastoma". Pediatric Blood & Cancer. 59 (5): 776–9. doi:10.1002/pbc.24215. PMID 22692949. S2CID 65545.
- ↑ Emre, S; McKenna, GJ (December 2004). "Liver tumors in children". Pediatric Transplantation. 8 (6): 632–8. doi:10.1111/j.1399-3046.2004.00268.x. PMID 15598339. S2CID 35883310.
- ↑ Davit-Spraul, A; Gonzales, E; Baussan, C; Jacquemin, E (Jan 8, 2009). "Progressive familial intrahepatic cholestasis". Orphanet Journal of Rare Diseases. 4: 1. doi:10.1186/1750-1172-4-1. PMC 2647530. PMID 19133130.
