Metastasis
| Metastasis | |
|---|---|
 | |
| Description (en) | |
| Iri |
secondary neoplasm (en) neoplasm (en) |
| Specialty (en) | oncology |
| Identifier (en) | |
| ICD-O: | 8000/6 |
| DiseasesDB | 28954 |
| MedlinePlus | 002260 |
| eMedicine | 002260 |
| MeSH | D009362 |


Metastasis wani wakili ne mai yaduwa daga wuri na farko ko na farko zuwa wani wuri daban ko na biyu a cikin jikin mai gida; [1] yawanci ana amfani da kalmar lokacin da ake magana akan metastasis ta hanyar ciwon daji.[2] Sabbin wuraren cututtukan cututtuka, to, sune metastases ( mets ).[3][4] Gabaɗaya an bambanta shi daga mamayewar kansa, wanda shine haɓaka kai tsaye da shigar da ƙwayoyin cutar kansa zuwa kyallen maƙwabta.[5]
Ciwon daji yana faruwa ne bayan sel sun canza ta hanyar kwayoyin halitta don yaduwa cikin sauri kuma har abada. Wannan yaduwar rashin kulawa ta hanyar mitosis yana haifar da ƙwayar cuta ta farko. Kwayoyin da ke haifar da ƙari daga ƙarshe suna yin metaplasia, sannan dysplasia sannan anaplasia, wanda ke haifar da mummunan phenotype. Wannan malignancy yana ba da damar mamayewa a cikin wurare dabam dabam, sannan kuma mamayewa zuwa wuri na biyu don tumorigenesis .
Wasu ƙwayoyin cutar kansa da aka sani da ƙwayoyin tumor masu yaduwa suna samun damar shiga bangon lymphatic ko tasoshin jini, bayan haka za su iya yaduwa ta cikin jini zuwa wasu shafuka da kyallen takarda a cikin jiki.[6] An san wannan tsari (bi da bi) azaman yaduwar lymphatic ko hematogenous . Bayan sel masu ciwon sun zo hutawa a wani wuri, sai su sake shiga cikin jirgin ruwa ko bangon kuma su ci gaba da karuwa, daga bisani su haifar da wani ciwon daji da za a iya ganowa a asibiti.[ana buƙatar hujja] sabon ƙwayar cuta a matsayin ƙwayar ƙwayar cuta (ko sakandare ). Metastasis yana daya daga cikin alamun ciwon daji, wanda ke bambanta shi da ciwace-ciwacen daji.[7] Yawancin ciwon daji na iya daidaitawa, kodayake a cikin nau'i daban-daban. Basal cell carcinoma misali da wuya metastasizes.[7]
Lokacin da ƙwayoyin ƙari suka ƙaru, ana kiran sabon ƙwayar cuta ta sakandare ko ƙwayar cuta, kuma ƙwayoyinsa suna kama da waɗanda ke cikin ƙwayar asali ko na farko.[8] Wannan yana nufin cewa idan ciwon nono ya koma cikin huhu, ƙwayar cuta ta biyu ta ƙunshi ƙwayoyin nono marasa kyau, ba na ƙwayoyin huhu ba. Ciwon daji da ke cikin huhu ana kiransa da kansar nono metastatic, ba ciwon huhu ba . Metastasis shine maɓalli mai mahimmanci a cikin tsarin sarrafa kansa kamar tsarin tsarin TNM , inda yake wakiltar "M". A cikin rukuni na gaba ɗaya, metastasis yana sanya kansa a cikin Stage IV. Yiwuwar maganin warkewa suna raguwa sosai, ko galibi ana cire su gaba ɗaya lokacin da ciwon daji ya ƙaru.
Alamomi da alamomi
[gyara sashe | gyara masomin]
Da farko, ana bugun nodes na lymph na kusa da wuri. [9] Huhu, hanta, kwakwalwa, da kasusuwa sune wuraren da aka fi sani da metastasis daga ciwace-ciwace. [9]
- A cikin ƙananan ƙwayoyin lymph metastasis, alamar ta kowa shine lymphadenopathy
- Metastasis na huhu: tari, hemoptysis da dyspnea [9] (ƙancewar numfashi)
- Metastasis na hanta: hepatomegaly (ƙaramar hanta ), tashin zuciya [9] da jaundice [9]
- Metastasis na kashi: ciwon kashi, [9] karaya na kasusuwan da aka shafa [9]
- Kwakwalwa metastasis : bayyanar cututtuka na jijiya kamar ciwon kai, [9] seizures, [9] da vertigo [9]
Kodayake ciwon daji na ci gaba na iya haifar da ciwo, yawanci ba shine alamar farko ba.
Wasu marasa lafiya, duk da haka, ba su nuna alamun ba. [9] Lokacin da gabobin jiki ya kamu da cutar metastatic takan fara raguwa har sai kumburin lymph ya fashe, ko kuma ya sami lysis .
Pathophysiology
[gyara sashe | gyara masomin]Ciwon daji na metastatic ya zama ruwan dare a ƙarshen matakan ciwon daji. Yaduwar metastasis na iya faruwa ta hanyar jini ko lymphatics ko ta hanyoyi biyu. Wuraren da aka fi sani da metastases sune huhu, hanta, kwakwalwa, da kasusuwa.[10]
A halin yanzu, an gabatar da manyan ra'ayoyi guda uku don bayyana hanyar metastatic na ciwon daji: canjin epithelial-mesenchymal (EMT) da kuma mesenchymal-epithelial (MET) hasashe (1), hasashewar kwayar cutar kansa (2), da macrophage- Hasashen haɗakar ƙwayoyin kansar ƙwayar cuta (3). An kuma ba da shawarar wasu sabbin hasashe, watau, ƙarƙashin tasirin wasu ƙwayoyin cuta na ƙwayoyin cuta da/ko damuwa ta jiki, ƙwayoyin kansa za su iya fuskantar korar makaman nukiliya tare da ɓarna macrophage da haɗuwa na gaba, tare da samuwar ƙwayoyin haɗakar cutar kansa (CFCs). [11]
Abubuwan da suka shafi
[gyara sashe | gyara masomin]Metastasis yana ƙunshe da jerin matakai masu rikitarwa waɗanda ƙwayoyin kansa ke barin asalin asalin ƙwayar cuta kuma suyi ƙaura zuwa wasu sassan jiki ta hanyar jini, ta hanyar tsarin lymphatic, ko ta tsawaita kai tsaye. Don yin haka, ƙananan ƙwayoyin cuta suna rabu da ƙwayar cuta ta farko kuma suna haɗawa da kuma lalata sunadaran da ke tattare da matrix na waje (ECM), wanda ke raba ƙwayar cuta daga ƙwayoyin da ke kusa. Ta hanyar wulakanta waɗannan sunadaran, ƙwayoyin kansa suna iya keta ECM kuma su tsere. Wurin metastases ba koyaushe bane bazuwar, tare da nau'ikan ciwon daji daban-daban waɗanda ke yaduwa zuwa ga wasu gabobin jiki da kyallen takarda a ƙimar da ya fi yadda ake tsammani ta hanyar ƙididdiga kawai.[12] Ciwon daji na nono, alal misali, yana yin ƙaura zuwa ƙasusuwa da huhu. Wannan ƙayyadaddun da alama ana yin sulhu ta hanyar ƙwayoyin sigina masu narkewa kamar chemokines[13] da canza yanayin haɓakar beta .[14] Jiki yana tsayayya da metastasis ta hanyoyi daban-daban ta hanyar ayyukan wani nau'in sunadaran da aka sani da masu hana metastasis, wanda kusan dozin an san su.[15]
Kwayoyin ɗan adam suna nuna nau'ikan motsi daban-daban: motsi na gama gari, motsi -nau'in mesenchymal, da motsin amoeboid . Kwayoyin cutar kansa galibi suna canzawa tsakanin nau'ikan motsi daban-daban da dacewa. Wasu masu binciken cutar kansa suna fatan samun magungunan da za su iya dakatarwa ko aƙalla rage yaduwar cutar kansa ta ko ta yaya toshe wani matakin da ya dace a cikin nau'ikan motsi ɗaya ko fiye. [16][17]
Duk matakan ɓacin rai na metastatic sun ƙunshi matakai na zahiri da yawa. Shigewar tantanin halitta yana buƙatar samar da ƙarfi, kuma lokacin da ƙwayoyin cutar kansa ke yaduwa ta hanyar vasculature, wannan yana buƙatar gibin jiki a cikin tasoshin jini don ƙirƙirar.[18] Bayan runduna, ƙa'idar nau'ikan nau'ikan tantanin halitta da adhesions na sel-matrix na da mahimmanci yayin metastasis.
Matakan metastatic ana tsara su sosai ta nau'ikan tantanin halitta daban-daban, gami da sel na jini (kwayoyin endothelial), ƙwayoyin rigakafi ko ƙwayoyin stromal. Ci gaban sabuwar hanyar sadarwa ta hanyoyin jini, wanda ake kira tumor angiogenesis,[19] alama ce mai mahimmanci ta kansa. Don haka an ba da shawarar cewa masu hana angiogenesis zasu hana haɓakar metastases.[7] An nuna ƙwararrun ƙwayoyin cuta da angiogenesis.[20][21] Kwayoyin mahaifa na endothelial suna da mahimmanci a cikin ci gaban ƙwayar cuta, angiogenesis da metastasis, kuma ana iya yin alama ta amfani da Inhibitor na DNA Binding 1 (ID1). Wannan labari ne da ake nema yana nufin cewa masu binciken sun sami ikon waƙa da sel na progogelalial daga cikin ƙwayar ƙasa zuwa jini ga ƙwayar cuta ga ƙwayar cuta zuwa kumburi. Kwayoyin ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwayar cuta suna nuna cewa wannan nau'in tantanin halitta a cikin haɓakar jini-jini yana da mahimmanci a cikin saitin ƙari da metastasis. Bugu da ƙari kuma, zubar da ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙashi na iya haifar da raguwa mai yawa a cikin ci gaban ƙwayar cuta da ci gaban vasculature. Don haka, sel masu tasowa na endothelial suna da mahimmanci a cikin ilimin halittar tumo kuma suna gabatar da sabbin dabarun warkewa.[22] Tsarin garkuwar jiki yawanci ana soke shi a cikin ciwon daji kuma yana shafar matakai da yawa na ci gaban ƙari, gami da metastasis.
Tsarin Epigenetic kuma yana taka muhimmiyar rawa a cikin haɓakar ƙwayoyin ƙwayar cuta da aka yaɗa. Metastases suna nuna sauye-sauye a cikin gyare-gyare na tarihi, irin su H3K4-methylation da H3K9-methylation, idan aka kwatanta da ma'auni na farko.[23] Wadannan gyare-gyare na epigenetic a cikin metastases na iya ba da damar yaduwa da rayuwa na ƙwayoyin tumor da aka yada a cikin gabobin nesa.[24]
Wani bincike na baya-bayan nan ya nuna cewa PKC-iota yana inganta mamayewar kwayar cutar melanoma ta hanyar kunna Vimentin yayin EMT. PKC-iota hanawa ko ƙwanƙwasa ya haifar da karuwa a cikin matakan E-cadherin da RhoA yayin da aka rage jimlar Vimentin, phosphorylated Vimentin (S39) da Par6 a cikin ƙwayoyin melanoma na metastatic. Waɗannan sakamakon sun ba da shawarar cewa PKC-ι yana da hannu a cikin hanyoyin sigina waɗanda ke daidaita EMT a cikin melanoma ta haka kai tsaye yana haɓaka metastasis.[25]
Kwanan nan, jerin manyan gwaje-gwajen da aka yi suna nuna cewa haɗin gwiwar tattaunawa ta tsaka-tsakin tsaka-tsakin tsaka-tsaki ta hanyar exosome vesicles wani muhimmin abu ne da ke cikin dukkan matakai na mamayewa-metastasis cascade.[26]
Hanyoyi
[gyara sashe | gyara masomin]Metastasis yana faruwa ta hanyoyi huɗu masu zuwa:
Transcoelomic
[gyara sashe | gyara masomin]Yaduwar malignancy zuwa cikin cavities na jiki na iya faruwa ta hanyar shiga saman peritoneal, pleural, pericardial, ko subarachnoid sarari. Misali, ciwace-ciwacen ovarian na iya yaduwa ta hanyar transperitoneally zuwa saman hanta.
Lymphatic yaduwa
[gyara sashe | gyara masomin]Yaduwar ƙwayar cuta yana ba da damar jigilar ƙwayoyin tumo zuwa ƙwayoyin lymph na yanki kusa da ƙwayar cuta ta farko kuma a ƙarshe, zuwa wasu sassan jiki. Ana kiran wannan haɗin gwiwa, nodes masu kyau, ko cutar yanki. "Kyakkyawan nodes" kalma ce da ƙwararrun likita za su yi amfani da ita don kwatanta ƙwayoyin lymph na yanki waɗanda aka gwada tabbatacce don rashin lafiya. Al'adar likita ce ta gama gari don gwada ta hanyar biopsy aƙalla kumburin lymph ɗaya kusa da wani wurin ƙari lokacin yin tiyata don bincika ko cire ƙari. Wannan kumburin lymph ana kiransa saƙon lymph node . Yaduwar Lymphatic ita ce hanyar da aka fi sani da metastasis na farko don carcinomas .[7] Sabanin haka, ba sabon abu ba ne don sarcoma don daidaitawa ta wannan hanya. Yaduwar da aka keɓe zuwa ƙananan ƙwayoyin lymph na yanki kusa da ƙwayar cuta ta farko ba a ƙidaya shi azaman metastasis ba, kodayake wannan alama ce ta sakamako mafi muni. A ƙarshe tsarin lymphatic yana magudawa daga magudanar thoracic da duct na dama zuwa cikin tsarin jijiyar jini a kusurwar jijiyoyi da kuma cikin veins na brachiocephalic, sabili da haka waɗannan kwayoyin halitta suna iya yadawa ta hanyar hematogenous.

Hematogenous yadawa
[gyara sashe | gyara masomin]Wannan hanya ce ta al'ada ta metastasis don sarcomas, amma kuma ita ce hanyar da aka fi so don wasu nau'in ciwon daji, irin su ciwon daji na renal cell wanda ya samo asali a cikin koda da follicular carcinomas na thyroid. Saboda ƙananan bangon su, jijiyoyi suna mamayewa akai-akai fiye da arteries, kuma metastasis yana kula da bin tsarin jijiyar jini . Wato, yaɗuwar hematogenous sau da yawa yakan bi salo daban-daban dangane da wurin da kumburin farko yake. Alal misali, ciwon daji na launin fata yana yaduwa ta farko ta hanyar portal vein zuwa hanta.
Canalicular baza
[gyara sashe | gyara masomin]Wasu ciwace-ciwacen ciwace-ciwace, musamman carcinomas na iya daidaitawa tare da filayen canalicular na jiki. Waɗannan wurare sun haɗa da misali bile ducts, tsarin urinary, hanyoyin iska da sararin subarachnoid . Tsarin yana kama da na transcoelomic baza. Koyaya, sau da yawa ba a sani ba ko ciwace-ciwacen da aka gano a lokaci guda na tsarin canalicular tsari ne na metastatic ko kuma a zahiri ciwace-ciwacen ciwace-ciwacen da wakili ɗaya ke haifar da shi (ciwon daji na filin ).
Ƙayyadaddun manufa ta gabobin jiki
[gyara sashe | gyara masomin]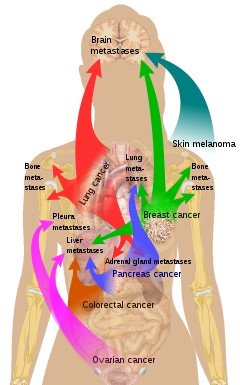
Akwai yuwuwar wasu ciwace-ciwace zuwa iri a wasu gabobin. An fara tattauna wannan a matsayin ka'idar "iri da ƙasa" ta Stephen Paget a cikin 1889. Yunkuri don kwayar metastatic don yaduwa ga wani niyyar da aka harba 'ungiyar unguwa'. Misali, ciwon daji na prostate yakan yi metastasize zuwa kashi. Hakazalika, ciwon daji na hanji yana da hali don daidaita hanta. Ciwon daji na ciki sau da yawa yakan kai ga ovary a cikin mata, lokacin da ake kira ciwon daji na Krukenberg .
Bisa ga ka'idar "iri da ƙasa", yana da wuya ƙwayoyin ciwon daji su rayu a waje da yankinsu na asali, don haka don daidaitawa dole ne su sami wuri mai irin wannan halaye.[28] Alal misali, ƙwayoyin ciwon nono, waɗanda ke tattara ions calcium daga madarar nono, suna daidaitawa zuwa nama na kashi, inda za su iya tattara ions na calcium daga kashi. Melanoma mai cutarwa ya yadu zuwa kwakwalwa, mai yiwuwa saboda nama na jijiyoyi da melanocytes suna tasowa daga layin tantanin halitta a cikin amfrayo .[29]
A cikin 1928, James Ewing ya kalubalanci ka'idar "iri da ƙasa" kuma ya ba da shawarar cewa metastasis yana faruwa ne kawai ta hanyoyin jiki da na inji. An yi amfani da wannan hasashe kwanan nan don ba da shawarar hasashe da yawa game da yanayin rayuwar ƙwayoyin tumor ƙwayoyin cuta (CTCs) da kuma sanyawa cewa za a iya fahimtar tsarin yaɗuwar ta hanyar hangen nesa 'tace da kwarara'.[30] Duk da haka, shaidun zamani sun nuna cewa ƙwayar ƙwayar cuta ta farko na iya ƙaddamar da ƙwayoyin cuta ta organotropic metastases ta hanyar haifar da samuwar pre-metastatic niches a wurare masu nisa, inda ƙwayoyin metastatic masu shigowa zasu iya shiga da kuma yin mulkin mallaka.[26] Musamman, exosome vesicles boye ta ciwace-ciwacen daji an nuna su gida zuwa pre-metastatic sites, inda suke kunna pro-metastatic matakai kamar angiogenesis da kuma gyara na rigakafi mahallin, don inganta m microenvironment ga sakandare ƙari girma.[26]
Metastasis da ciwon daji na farko
[gyara sashe | gyara masomin]An yi la'akari da cewa metastasis koyaushe yana yin daidai da ciwon daji na farko, kuma, kamar haka, ƙari ne wanda ya fara daga kwayar cutar kansa ko sel a wani sashe na jiki. Koyaya, sama da kashi 10% na marasa lafiya da ke gabatarwa ga sassan oncology za su sami metastases ba tare da samun ci gaba na farko ba. A cikin waɗannan lokuta, likitoci suna kiran ƙwayar cuta ta farko a matsayin "ba a sani ba" ko "fasafi," kuma an ce majiyyaci yana da ciwon daji wanda ba a san asalin asali ba (CUP) ko kuma ba a sani ba (UPT).[31] An kiyasta cewa kashi 3 cikin 100 na dukkan cututtukan daji ba a san asalinsu ba.[32] Nazarin ya nuna cewa, idan tambaya mai sauƙi ba ta bayyana tushen ciwon daji ba (tarin jini - "watakila huhu ", jinin fitsari - "wataƙila mafitsara "), hadaddun hoto ba zai yiwu ba.[32] A wasu daga cikin waɗannan al'amuran ƙwayar cuta ta farko na iya bayyana daga baya.
Amfani da immunohistochemistry ya ƙyale masu ilimin cututtuka su ba da ainihi ga yawancin waɗannan metastases. Koyaya, hoton wurin da aka nuna kawai lokaci-lokaci yana bayyana na farko. A lokuta da ba kasafai ba (misali, na melanoma ), ba a sami ciwace-ciwacen farko ba, ko da a kan gawa . Don haka ana tunanin cewa wasu ciwace-ciwacen ciwace-ciwace na iya komawa gaba ɗaya, amma suna barin metastases a baya. A wasu lokuta, ƙwayar cutar na iya zama ƙanƙanta da/ko a wani wuri da ba a sani ba don a gano shi.
Bincike
[gyara sashe | gyara masomin]
Kwayoyin da ke cikin ƙwayar ƙwayar cuta suna kama da waɗanda ke cikin ƙwayar cuta ta farko. Da zarar an bincika nama mai ciwon daji a ƙarƙashin na'urar hangen nesa don tantance nau'in tantanin halitta, yawanci likita zai iya faɗi ko ana samun irin wannan nau'in tantanin halitta a cikin sassan jikin da aka ɗauko samfurin nama.
Misali, kwayoyin cutar kansar nono suna kama da juna ko an same su a cikin nono ko kuma sun yada zuwa wani sashe na jiki. Don haka, idan samfurin nama da aka ɗauka daga ƙari a cikin huhu ya ƙunshi sel masu kama da ƙwayoyin nono, likita ya ƙayyade cewa ƙwayar huhu ita ce ƙari na biyu. Duk da haka, ƙaddamar da ƙwayar ƙwayar cuta ta farko na iya zama da wahala sau da yawa, kuma likitan ilimin likitanci na iya amfani da wasu fasahohin adjuvant, irin su immunohistochemistry, FISH ( fluorescent in situ hybridization ), da sauransu. Duk da amfani da dabaru, a wasu lokuta cutar ta farko ta kasance ba a gano ta ba.
Ana iya samun ciwon daji na metastatic a lokaci guda da ƙwayar cuta ta farko, ko watanni ko shekaru bayan haka. Lokacin da aka sami ƙari na biyu a cikin majiyyaci da aka yi wa maganin kansa a baya, ya fi sau da yawa metastasis fiye da wani ciwon daji na farko.
A baya an yi tunanin cewa yawancin ƙwayoyin ciwon daji suna da ƙananan yuwuwar metastatic kuma cewa akwai ƙwayoyin da ba kasafai ba waɗanda ke haɓaka ikon haɓaka ta hanyar haɓakar maye gurbin somatic.[33] Bisa ga wannan ka'idar, ganewar asali na ciwon daji na metastatic yana yiwuwa ne kawai bayan abin da ya faru na metastasis. Hannun al'ada na gano cutar kansa (misali biopsy ) zai bincika ƙaramin adadin ƙwayoyin cutar kansa kawai kuma ba zai iya yin samfuri daga yawan jama'a tare da yuwuwar metastatic ba.[34]
Ba a tabbatar da ka'idar maye gurbin somatic na ci gaban metastasis a cikin cututtukan daji na ɗan adam ba. Maimakon haka, da alama yanayin kwayoyin halitta na ƙwayar cuta ta farko tana nuna ikon wannan ciwon daji don daidaitawa.[34] Bincike da aka kwatanta maganganun kwayoyin halitta tsakanin adenocarcinomas na farko da na metastatic ya gano wani yanki na kwayoyin halitta wanda furcinsu zai iya bambanta ciwace-ciwacen daji daga ciwace-ciwacen daji, wanda aka yiwa lakabi da "sa hannu na metastatic."[34] Ƙwayoyin halitta waɗanda aka tsara a cikin sa hannu sun haɗa da: SNRPF, HNRPAB, DHPS da securin . Actin, myosin da MHC aji II ƙa'ida kuma an haɗa su da sa hannu. Bugu da ƙari, an kuma lura da bayyanar cututtukan da ke da alaƙa da waɗannan ƙwayoyin cuta a cikin wasu ciwace-ciwacen daji na farko, wanda ke nuna cewa ana iya gano ƙwayoyin da ke da yuwuwar metastasize a lokaci guda tare da ganewar ƙwayar cuta ta farko.[35] Ayyukan kwanan nan sun gano wani nau'i na rashin zaman lafiyar kwayoyin halitta a cikin ciwon daji da ake kira rashin zaman lafiya na chromosome (CIN) a matsayin direba na metastasis.[36] A cikin ƙwayoyin cutar kansa masu ƙarfi, ɓangarori na DNA daga chromosomes marasa ƙarfi suna zubo a cikin cytosol wanda ke haifar da ci gaba da kunna hanyoyin rigakafi na asali, waɗanda ƙwayoyin kansa ke sace su yada zuwa gabobin nesa.
Bayanin wannan sa hannu na metastatic an haɗa shi tare da rashin fahimta mara kyau kuma an nuna shi daidai a cikin nau'ikan ciwon daji da yawa. An nuna hasashen ya zama mafi muni ga mutane waɗanda ciwace-ciwacen ciwace-ciwace suka bayyana sa hannun metastatic.[34] Bugu da ƙari, an nuna bayanin waɗannan kwayoyin halittar da ke da alaƙa da metastatic don amfani da wasu nau'in ciwon daji ban da adenocarcinoma . Metastases na ciwon nono, medulloblastoma da ciwon gurguwar prostate duk suna da irin wannan salon magana na waɗannan kwayoyin halitta masu alaƙa da metastasis.[34]
Gano wannan sa hannu mai alaƙa da metastasis yana ba da alƙawarin gano ƙwayoyin sel waɗanda ke da yuwuwar metastatic a cikin ƙwayar cuta ta farko da kuma bege don inganta hasashen waɗannan cututtukan daji masu alaƙa da metastatic. Bugu da ƙari, gano ƙwayoyin halittar da aka canza bayanin su a cikin metastasis yana ba da yuwuwar maƙasudi don hana metastasis.[34]
-
Micrograph na ciwon daji na thyroid ( papillary thyroid carcinoma ) a cikin ƙwayar lymph na wuyansa. H&E tabo
-
Hoton CT na metastases na hanta da yawa
-
Hoton CT na metastasis na huhu
-
Metastasis da aka tabbatar ta hanyar biopsy hanta (tumor ( adenocarcinoma ) - ƙananan kashi biyu bisa uku na hoto). H&E tabo .
-
Metastatic ciwon daji a cikin huhu
-
Metastases daga huhu zuwa kwakwalwa
-
Metastases daga huhu zuwa pancreas
Gudanarwa
[gyara sashe | gyara masomin]Ana ƙayyade jiyya da rayuwa, zuwa matuƙar, ta hanyar ko ciwon daji ya kasance a wuri ko yaduwa zuwa wasu wurare a cikin jiki. Idan ciwon daji ya ƙaru zuwa wasu kyallen takarda ko gabobin yawanci yana ƙaruwa da yuwuwar mutuwa ga majiyyaci. Wasu ciwon daji-kamar wasu nau'in cutar sankarar bargo, ciwon daji na jini, ko kuma rashin lafiya a cikin kwakwalwa - na iya kashewa ba tare da yaduwa ba.
Da zarar ciwon daji ya ƙaru har yanzu ana iya bi da shi tare da radiosurgery, chemotherapy, radiation far, nazarin halittu, hormone far, tiyata, ko hade da wadannan tsokoki ("multimodal far"). Zaɓin magani ya dogara da dalilai da yawa, ciki har da nau'in ciwon daji na farko, girman da wuri na metastases, shekarun mai haƙuri da lafiyar jiki, da kuma nau'in jiyya da aka yi amfani da su a baya. A cikin marasa lafiya da aka gano tare da CUP sau da yawa har yanzu yana yiwuwa a bi da cutar koda lokacin da ba a iya gano ƙwayar cuta ta farko.
Jiyya na yanzu ba kasafai suke iya warkar da ciwon daji ba ko da yake wasu ciwace-ciwacen ciwace-ciwacen ciwace-ciwacen ciwace-ciwacen ciwace-ciwacen ciwace-ciwacen ciwace-ciwacen ciwace-ciwacen ciwace-ciwace, irin su ciwon daji na testicular da kansar thyroid, galibi ana iya warkewa.
Kulawa mai laushi, kulawa da nufin inganta rayuwar mutanen da ke da manyan cututtuka, an ba da shawarar a matsayin wani ɓangare na shirye-shiryen gudanarwa don metastasis.[37] Sakamako daga nazari na yau da kullun na wallafe-wallafen akan jiyya na radiation don metastases na kwakwalwa sun gano cewa akwai ƙaramin shaida don sanar da tasirin kwatancen da sakamakon da ke da alaƙa da haƙuri akan ingancin rayuwa, matsayin aiki, da tasirin fahimi.[38]
Bincike
[gyara sashe | gyara masomin]Kodayake metastasis an yarda da shi don zama sakamakon ƙaurawar ƙwayoyin tumo, akwai hasashe da ke cewa wasu metastases sune sakamakon matakan kumburi ta ƙwayoyin rigakafi marasa al'ada.[39] Kasancewar ciwon daji na metastatic a cikin rashin ciwace-ciwacen farko kuma yana nuna cewa metastasis ba koyaushe ke haifar da mugayen ƙwayoyin cuta waɗanda ke barin ciwace-ciwacen farko ba.[40]
Binciken da ƙungiyar Sarna ta yi ya tabbatar da cewa ƙwayoyin melanoma masu launin launi suna da nauyin matasa kimanin 4.93, yayin da a cikin waɗanda ba su da launi ya kasance 0.98 kawai.[41] A wani gwaji kuma sun gano cewa elasticity na sel melanoma yana da mahimmanci ga metastasis da girma: ciwace-ciwacen da ba su da launi sun fi girma fiye da launi kuma yana da sauƙin yadawa. Sun nuna cewa akwai sel masu launi da marasa launi a cikin ciwace-ciwacen ƙwayar cuta na melanoma, ta yadda za su iya zama masu jure wa ƙwayoyi da metastatic.[41]
Tarihi
[gyara sashe | gyara masomin]A cikin Maris 2014 masu bincike sun gano mafi tsufa cikakken misali na ɗan adam da ciwon daji na metastatic. Ciwon daji ya samo asali ne a cikin kwarangwal mai shekaru 3,000 da aka gano a cikin 2013 a wani kabari a Sudan tun daga shekara ta 1200 BC. Anyi nazarin kwarangwal ta hanyar amfani da radiyo da na'urar duban abin gani na lantarki. An buga waɗannan binciken a cikin mujallar Kimiya ta Jama'a.[42][43][44]
Etymology
[gyara sashe | gyara masomin]Metastasis kalmar Helenanci ce ma'ana "maura", daga μετά, meta, "na gaba", da στάσις, stasis, "jeri".
Duba kuma
[gyara sashe | gyara masomin]- Abscopal sakamako
- Kwakwalwa metastasis
- Brown-Séquard ciwo (sassan kan rashin lafiya na kogo, germinoma, ciwon renal cell carcinoma da ciwon huhu)
- Hijira tantanin halitta
- Tuntuɓar daidaitawa
- Cutar da aka yada
- Micrometastasis
- Mouse model na nono metastasis
- Positron emission tomography (PET)
Hanyoyin haɗi na waje
[gyara sashe | gyara masomin]- Tambaya&A: Ciwon daji na Metastatic -daga Cibiyar Archived 2008-08-27 at the Wayback Machine Ciwon daji ta Kasa
Manazarta
[gyara sashe | gyara masomin]- ↑ "Metastasis", Merriam–Webster online, accessed 20 Aug 2017.
- ↑ "What is Metastasis?". Cancer.Net. 2 February 2016.
- ↑ Klein CA (September 2008). "Cancer. The metastasis cascade". Science. 321 (5897): 1785–7. doi:10.1126/science.1164853. PMID 18818347. S2CID 206515808.
- ↑ Chiang AC, Massagué J (December 2008). "Molecular basis of metastasis". The New England Journal of Medicine. 359 (26): 2814–23. doi:10.1056/NEJMra0805239. PMC 4189180. PMID 19109576.
- ↑ "Invasion and metastasis". Cancer Australia. 2014-12-16. Retrieved 2018-10-26.
- ↑ Maheswaran S, Haber DA (February 2010). "Circulating tumor cells: a window into cancer biology and metastasis". Current Opinion in Genetics & Development. 20 (1): 96–9. doi:10.1016/j.gde.2009.12.002. PMC 2846729. PMID 20071161.
- ↑ 7.0 7.1 7.2 7.3 Kumar V, Abbas AK, Fausto N, Robbins SL, Cotran RS (2005). Robbins and Cotran pathologic basis of disease (7th ed.). Philadelphia: Elsevier Saunders. ISBN 978-0-7216-0187-8.
- ↑ "O que é a metástase?" (in Harshen Potugis). Dr. Felipe Ades MD PhD—Oncologista. 2018-07-24. Retrieved 2018-10-23.
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 National Cancer Institute: Metastatic Cancer: Questions and Answers Archived 2008-08-27 at the Wayback Machine. Retrieved on<rc-c2d-number> 2008-11-01</rc-c2d-number>
- ↑ "Metastatic Cancer: Questions and Answers". National Cancer Institute. Archived from the original on 2008-08-27. Retrieved 2008-08-28.
- ↑ Olteanu G-E, Mihai I-M, Bojin F, Gavriliuc O, Paunescu V. The natural adaptive evolution of cancer: The metastatic ability of cancer cells. Bosn J of Basic Med Sci [Internet]. 2020Feb.3;. Available from: https://www.bjbms.org/ojs/index.php/bjbms/article/view/4565
- ↑ Nguyen DX, Massagué J (May 2007). "Genetic determinants of cancer metastasis". Nature Reviews. Genetics. 8 (5): 341–52. doi:10.1038/nrg2101. PMID 17440531. S2CID 17745552.
- ↑ Zlotnik A, Burkhardt AM, Homey B (August 2011). "Homeostatic chemokine receptors and organ-specific metastasis". Nature Reviews. Immunology. 11 (9): 597–606. doi:10.1038/nri3049. PMID 21866172. S2CID 34438005.
- ↑ Drabsch Y, ten Dijke P (June 2011). "TGF-β signaling in breast cancer cell invasion and bone metastasis". Journal of Mammary Gland Biology and Neoplasia. 16 (2): 97–108. doi:10.1007/s10911-011-9217-1. PMC 3095797. PMID 21494783.
- ↑ Yoshida BA, Sokoloff MM, Welch DR, Rinker-Schaeffer CW (November 2000). "Metastasis-suppressor genes: a review and perspective on an emerging field". Journal of the National Cancer Institute. 92 (21): 1717–30. doi:10.1093/jnci/92.21.1717. PMID 11058615.
- ↑ Matteo Parri, Paola Chiarugi. "Rac and Rho GTPases in cancer cell motility control" 2010
- ↑ Friedl P, Wolf K (May 2003). "Tumour-cell invasion and migration: diversity and escape mechanisms". Nature Reviews. Cancer. 3 (5): 362–74. doi:10.1038/nrc1075. PMID 12724734. S2CID 5547981.
- ↑ Escribano J, Chen MB, Moeendarbary E, Cao X, Shenoy V, Garcia-Aznar JM, et al. (May 2019). "Balance of mechanical forces drives endothelial gap formation and may facilitate cancer and immune-cell extravasation". PLOS Computational Biology. 15 (5): e1006395. arXiv:1811.09326. Bibcode:2019PLSCB..15E6395E. doi:10.1371/journal.pcbi.1006395. PMC 6497229. PMID 31048903.
- ↑ Weidner N, Semple JP, Welch WR, Folkman J (January 1991). "Tumor angiogenesis and metastasis--correlation in invasive breast carcinoma". The New England Journal of Medicine. 324 (1): 1–8. doi:10.1056/NEJM199101033240101. PMID 1701519.
- ↑ Gao D, Nolan DJ, Mellick AS, Bambino K, McDonnell K, Mittal V (January 2008). "Endothelial progenitor cells control the angiogenic switch in mouse lung metastasis". Science. 319 (5860): 195–8. Bibcode:2008Sci...319..195G. doi:10.1126/science.1150224. PMID 18187653. S2CID 12577022.
- ↑ Nolan DJ, Ciarrocchi A, Mellick AS, Jaggi JS, Bambino K, Gupta S, et al. (June 2007). "Bone marrow-derived endothelial progenitor cells are a major determinant of nascent tumor neovascularization". Genes & Development. 21 (12): 1546–58. doi:10.1101/gad.436307. PMC 1891431. PMID 17575055.
- ↑ Mellick AS, Plummer PN, Nolan DJ, Gao D, Bambino K, Hahn M, et al. (September 2010). "Using the transcription factor inhibitor of DNA binding 1 to selectively target endothelial progenitor cells offers novel strategies to inhibit tumor angiogenesis and growth". Cancer Research. 70 (18): 7273–82. doi:10.1158/0008-5472.CAN-10-1142. PMC 3058751. PMID 20807818.
- ↑ Franci C, Zhou J, Jiang Z, Modrusan Z, Good Z, Jackson E, Kouros-Mehr H (2013). "Biomarkers of residual disease, disseminated tumor cells, and metastases in the MMTV-PyMT breast cancer model". PLOS ONE. 8 (3): e58183. Bibcode:2013PLoSO...858183F. doi:10.1371/journal.pone.0058183. PMC 3592916. PMID 23520493.
- ↑ Lujambio A, Esteller M (February 2009). "How epigenetics can explain human metastasis: a new role for microRNAs". Cell Cycle. 8 (3): 377–82. doi:10.4161/cc.8.3.7526. PMID 19177007.
- ↑ Ratnayake WS, Apostolatos AH, Ostrov DA, Acevedo-Duncan M (November 2017). "Two novel atypical PKC inhibitors; ACPD and DNDA effectively mitigate cell proliferation and epithelial to mesenchymal transition of metastatic melanoma while inducing apoptosis". International Journal of Oncology. 51 (5): 1370–1382. doi:10.3892/ijo.2017.4131. PMC 5642393. PMID 29048609.
- ↑ 26.0 26.1 26.2 Syn N, Wang L, Sethi G, Thiery JP, Goh BC (July 2016). "Exosome-Mediated Metastasis: From Epithelial-Mesenchymal Transition to Escape from Immunosurveillance". Trends in Pharmacological Sciences. 37 (7): 606–617. doi:10.1016/j.tips.2016.04.006. PMID 27157716.
- ↑ List of included entries and references is found on main image page in Commons: Commons:File:Metastasis sites for common cancers.svg#Summary
- ↑ Hart IR (1982). "'Seed and soil' revisited: mechanisms of site-specific metastasis". Cancer and Metastasis Reviews. 1 (1): 5–16. doi:10.1007/BF00049477. PMID 6764375. S2CID 19573769.
- ↑ Weinberg RA (2007). The Biology of Cancer. New York: Taylor & Francis. ISBN 978-0-8153-4076-8. quoted in Angier N (3 April 2007). "Basics: A mutinous group of cells on a greedy, destructive task". The New York Times.
- ↑ Scott J, Kuhn P, Anderson AR (July 2012). "Unifying metastasis--integrating intravasation, circulation and end-organ colonization". Nature Reviews. Cancer. 12 (7): 445–6. doi:10.1038/nrc3287. PMC 4533867. PMID 22912952.
- ↑ Ettinger DS, Agulnik M, Cates JM, Cristea M, Denlinger CS, Eaton KD, et al. (December 2011). "NCCN Clinical Practice Guidelines Occult primary". Journal of the National Comprehensive Cancer Network. 9 (12): 1358–95. doi:10.6004/jnccn.2011.0117. PMID 22157556.
- ↑ 32.0 32.1 Briasoulis E, Pavlidis N (1997). "Cancer of Unknown Primary Origin". The Oncologist. 2 (3): 142–152. doi:10.1634/theoncologist.2-3-142. PMID 10388044.
- ↑ Poste G, Fidler IJ (January 1980). "The pathogenesis of cancer metastasis". Nature. 283 (5743): 139–46. Bibcode:1980Natur.283..139P. CiteSeerX 10.1.1.553.5472. doi:10.1038/283139a0. PMID 6985715. S2CID 4302076.
- ↑ 34.0 34.1 34.2 34.3 34.4 34.5 Ramaswamy S, Ross KN, Lander ES, Golub TR (January 2003). "A molecular signature of metastasis in primary solid tumors". Nature Genetics. 33 (1): 49–54. doi:10.1038/ng1060. PMID 12469122. S2CID 12059602.
- ↑ van 't Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AA, Mao M, et al. (January 2002). "Gene expression profiling predicts clinical outcome of breast cancer". Nature. 415 (6871): 530–6. doi:10.1038/415530a. hdl:1874/15552. PMID 11823860. S2CID 4369266.
- ↑ Bakhoum SF, Ngo B, Laughney AM, Cavallo JA, Murphy CJ, Ly P, et al. (January 2018). "Chromosomal instability drives metastasis through a cytosolic DNA response". Nature. 553 (7689): 467–472. Bibcode:2018Natur.553..467B. doi:10.1038/nature25432. PMC 5785464. PMID 29342134.
- ↑ Irwin KE, Greer JA, Khatib J, Temel JS, Pirl WF (February 2013). "Early palliative care and metastatic non-small cell lung cancer: potential mechanisms of prolonged survival". Chronic Respiratory Disease. 10 (1): 35–47. doi:10.1177/1479972312471549. PMID 23355404. S2CID 6743524.
- ↑ Garsa, Adam; Jang, Julie K.; Baxi, Sangita; Chen, Christine; Akinniranye, Olamigoke; Hall, Owen; Larkin, Jody; Motala, Aneesa; Hempel, Susanne (2021). "Radiation Therapy for Brain Metastases: A Systematic Review". Practical Radiation Oncology (in Turanci). 11 (5): 354–365. doi:10.1016/j.prro.2021.04.002. PMID 34119447 Check
|pmid=value (help). - ↑ Shahriyari L (2016). "A new hypothesis: some metastases are the result of inflammatory processes by adapted cells, especially adapted immune cells at sites of inflammation". F1000Research. 5: 175. doi:10.12688/f1000research.8055.1. PMC 4847566. PMID 27158448.
- ↑ López-Lázaro M (2015-01-01). "The migration ability of stem cells can explain the existence of cancer of unknown primary site. Rethinking metastasis". Oncoscience. 2 (5): 467–75. doi:10.18632/oncoscience.159. PMC 4468332. PMID 26097879.
- ↑ 41.0 41.1 Sarna M, Krzykawska-Serda M, Jakubowska M, Zadlo A, Urbanska K (June 2019). "Melanin presence inhibits melanoma cell spread in mice in a unique mechanical fashion". Scientific Reports. 9 (1): 9280. Bibcode:2019NatSR...9.9280S. doi:10.1038/s41598-019-45643-9. PMC 6594928. PMID 31243305.
- ↑ Kelland K (17 March 2014). "Archaeologists discover earliest example of human with cancer". Reuters. Retrieved 18 March 2014.
- ↑ Ghosh P (18 March 2014). "Ancient skeleton is the earliest case of cancer yet detected". BBC. Retrieved 18 March 2014.
- ↑ Ross P (17 March 2014). "Possible Oldest Cancer Found In 3,000-Year-Old Skeleton Could Reveal 'Evolution' Of Modern Disease". International Business Times. Retrieved 18 March 2014.
- All articles with unsourced statements
- Articles with unsourced statements from March 2017
- Articles with invalid date parameter in template
- Webarchive template wayback links
- Cutar daji
- Shafuka masu fassarorin da ba'a duba ba
- CS1 Harshen Potugis-language sources (pt)
- CS1 errors: PMID
- CS1 Turanci-language sources (en)