Ciwon daji na prostate
Ciwon daji na prostate shine ci gaban kansa a cikin prostate, gland a cikin tsarin haihuwa na namiji.[1] Yawancin ciwon daji na prostate suna jinkirin girma; duk da haka kuma, wasu suna girma da sauri.[2][3] Kwayoyin ciwon daji na iya yaduwa daga prostate zuwa wasu sassan jiki, musamman kasusuwa da ƙwayoyin lymph.[4] Yana iya da farko ya haifar da babu alamun.[2] A mataki na gaba, yana iya haifar da wahalar fitsari, jini a cikin fitsari ko jin zafi a ƙashin ƙugu, baya, ko lokacin fitsari.[5] Cutar da aka sani da hyperplasia na prostatic na iya haifar da irin wannan alamun.[2] Sauran alamomin marigayi na iya haɗawa da jin gajiya saboda ƙarancin matakan jajayen ƙwayoyin jini.[2]
Abubuwan da ke ƙara haɗarin cutar kansar prostate sun haɗa da tsufa, tarihin iyali na cutar, da launin fata.[3] Kimanin kashi 99% na lokuta suna faruwa a cikin maza fiye da shekaru 50.[3] Samun dangi na farko tare da cutar yana kara haɗarin sau biyu zuwa uku. Sauran abubuwan da ka iya haɗawa sun haɗa da abinci mai yawa na nama da aka sarrafa, jan nama ko madara ko ƙarancin wasu kayan lambu.[3] An sami haɗin gwiwa tare da gonorrhea, amma ba a gano dalilin wannan dangantaka ba.[6] Haɗarin haɓaka yana haɗuwa da maye gurbin BRCA.[7] Ana gano kansar prostate ta hanyar biopsy.[5] Ana iya yin hoton likita don sanin ko ciwon daji ya yadu zuwa wasu sassan jiki.[5]
Binciken kansar prostate yana da cece-kuce.[3][8] Gwajin takamaiman antigen na Prostate (PSA) yana ƙara gano cutar kansa, amma yana da rigima game da ko yana inganta sakamako.[8][9][10] Ana ba da shawarar shawarar yanke shawara idan aka zo batun tantancewa tsakanin waɗanda ke da shekaru 55 zuwa 69.[11][12] Gwaji, idan an yi shi, ya fi dacewa a cikin waɗanda ke da tsawon rai.[13] Duk da yake masu hana 5a-reductase suna bayyana don rage ƙananan haɗarin ciwon daji, ba su shafar haɗarin ciwon daji mai girma kuma don haka ba a ba da shawarar yin rigakafi ba.[3] Ƙarawa tare da bitamin ko ma'adanai ba ya bayyana yana tasiri ga hadarin.[3][14]
Yawancin lokuta ana sarrafa su tare da sa ido mai aiki ko jira a hankali.[5] Wasu jiyya na iya haɗawa da haɗin tiyata, maganin radiation, maganin hormone ko chemotherapy.[5] Lokacin da kawai ya faru a cikin prostate, ana iya warkewa.[2] A cikin wadanda cutar ta yada zuwa kasusuwa, magungunan ciwo, bisphosphonates da maganin da aka yi niyya, da sauransu, na iya zama da amfani.[5] Sakamakon ya dogara ne akan shekarun mutum da sauran matsalolin kiwon lafiya da kuma yadda ciwon daji ke da yawa.[5] Yawancin maza masu fama da cutar kansar prostate ba sa mutuwa daga cutar.[5] Adadin rayuwa na shekaru 5 a Amurka shine 98%.[15]
A duniya baki daya, ita ce nau'in ciwon daji na biyu mafi yawa kuma na biyar kan haddasa mutuwar masu alaka da cutar daji a cikin maza.[16] A cikin 2018, ya faru a cikin maza miliyan 1.2 kuma ya yi sanadiyar mutuwar 359,000.[17] Ita ce cutar sankara mafi yawa a cikin maza a cikin kasashe 84, wanda ya fi faruwa a cikin kasashen da suka ci gaba.[18] Ƙididdigar ƙima na karuwa a cikin ƙasashe masu tasowa.[19] Gano ya ƙaru sosai a cikin 1980s da 1990s a wurare da yawa saboda ƙarin gwajin PSA.[3] Nazarin mazan da suka mutu daga abubuwan da ba su da alaƙa sun sami ciwon daji na prostate a cikin 30% zuwa 70% na waɗanda suka wuce shekaru 60.[2][18]
Alamomi da alamomi
[gyara sashe | gyara masomin]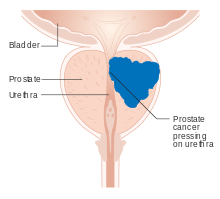
Ciwon daji na prostate na farko yawanci ba shi da bayyanar cututtuka. Lokacin da suka bayyana, sau da yawa suna kama da na prostate hyperplasia mara kyau . Wadannan sun hada da yawan fitsari, nocturia (yawan fitsari da daddare), wahalar farawa da kiyaye tsayayyen fitsari, hematuria (jini a cikin fitsari), dysuria (fitsari mai zafi) da gajiya saboda anemia, da ciwon kashi. [20] Ɗaya daga cikin binciken ya gano cewa kusan kashi ɗaya bisa uku na marasa lafiya da aka gano suna da ɗaya ko fiye da irin waɗannan alamun.[21]
Ciwon daji na prostate yana da alaƙa da tabarbarewar fitsari kamar yadda glandan prostate ke kewaye da urethra na prostate . Canje-canje a cikin gland yana shafar aikin fitsari kai tsaye. Saboda vas deferens yana sanya ruwan jima'i a cikin urethra na prostate, kuma ɓoye daga prostate yana cikin abun ciki na maniyyi, ciwon gurguwar prostate yana iya haifar da matsala tare da aikin jima'i da aiki, kamar wahalar samun haɓaka ko fitar maniyyi mai raɗaɗi.
Metastatic ciwon daji na prostate zai iya haifar da ƙarin bayyanar cututtuka. Alamar da aka fi sani shine ciwon kashi, sau da yawa a cikin kashin baya (kasusuwa na kashin baya), ƙashin ƙugu, ko haƙarƙari . Yaduwar ciwon daji zuwa wasu kasusuwa kamar femur yawanci zuwa sashin kashi kusa da prostate . Ciwon daji na prostate a cikin kashin baya zai iya damfara kashin baya, haifar da tingling, rauni na ƙafafu, da rashin daidaituwa na fitsari da kuma najasa .[22]
Abubuwan haɗari
[gyara sashe | gyara masomin]Abubuwan haɗari na farko sune kiba, shekaru, da tarihin iyali. An gano cewa maza masu kiba suna da kashi 34 cikin dari mafi girma daga cutar sankara ta prostate fiye da waɗanda ke da nauyin al'ada.[23] Ciwon daji na prostate ba sabon abu bane a cikin maza masu kasa da 45, amma ya zama ruwan dare tare da tsufa. Matsakaicin shekaru a lokacin ganewar asali shine 70.[24] Binciken gawarwaki na mutanen Sinawa, Jamusanci, Isra'ila, Jamaica, Sweden, da Ugandan da suka mutu sakamakon wasu dalilai sun sami kansar prostate a cikin kashi 30% na maza masu shekaru 50, kuma a cikin 80% na maza masu shekaru 70.[25][26][27]
Maza masu hawan jini sun fi kamuwa da ciwon daji na prostate. [28] Ƙananan haɓakar haɗari yana haɗuwa da rashin motsa jiki.[29] Matakan testosterone na jini[30] na iya ƙara haɗari.
Genetics
[gyara sashe | gyara masomin]Genetics na iya shafar haɗari, kamar yadda ƙungiyoyi tare da kabilanci, iyali, da takamaiman bambance-bambancen jinsi suka ba da shawara.[31] Maza da ke da dangi na farko (mahai ko ɗan'uwa) tare da ciwon daji na prostate suna da haɗarin kamuwa da ciwon gurguwar prostate sau biyu, kuma waɗanda ke da dangi biyu na farko da abin ya shafa suna da haɗarin ninka sau biyar idan aka kwatanta da maza marasa tarihin iyali.[32][33] Wannan haɗarin ya bayyana ya fi girma ga maza da ɗan'uwan da abin ya shafa fiye da waɗanda ke da uban da abin ya shafa. A Amurka, cutar sankara ta prostate ta fi kamuwa da bakar fata fiye da farare ko mutanen Hispanic, kuma ta fi kashe mutane bakaken fata.[34][35] Sabanin haka, yawan abubuwan da suka faru da mace-mace ga mazajen Hispanic sun kasance kashi ɗaya bisa uku na ƙasa fiye da na fararen fata waɗanda ba Hispanic ba. Nazarin tagwaye a Scandinavia sun nuna cewa kashi 40 cikin 100 na haɗarin cutar kansar prostate ana iya bayyana su ta hanyar abubuwan da aka gada .[36]
Yawancin kwayoyin halitta suna shiga cikin ciwon daji na prostate. Maye gurbi a cikin BRCA1 da BRCA2 (muhimman abubuwan haɗari ga ciwon daji na ovarian da ciwon nono a cikin mata) an haɗa su.[37] Sauran kwayoyin halittar da ke da alaƙa sun haɗa da geneditary prostate cancer gene 1 ( HPC1 ), da androgen receptor, da kuma mai karɓar bitamin D. TMPRSS2 - ETS gene iyali Fusion, musamman TMPRSS2- ERG ko TMPRSS2- ETV1 / 4 inganta ciwon daji cell girma.[38] Wadannan fusions na iya tasowa ta hanyar sarƙoƙi na sake tsarawa da ake kira chromoplexy .[39]
Biyu manyan nazarin ƙungiyoyin genome-fadi sun haɗu da polymorphisms guda-nucleotide polymorphisms (SNPs) zuwa ciwon daji na prostate a 2008.[40][41] Waɗannan binciken sun gano SNPs masu dacewa da yawa. Misali, mutanen da ke da nau'in TT allele a SNP rs10993994 an ba da rahoton cewa suna cikin haɗarin sau 1.6 mafi girma fiye da waɗanda ke da nau'in CC allele. Wannan SNP yana bayyana wani ɓangare na ƙarin haɗarin da Amirkawa-Amurka ke fuskanta. C allele ya fi yawa a cikin na ƙarshe; wannan SNP yana cikin yankin mai gabatarwa na kwayar halittar MSMB, don haka yana rinjayar adadin furotin MSMB da aka haɗa da ɓoye ta ƙwayoyin epithelial na prostate.[42]
Yayin da aka gudanar da ƙananan binciken da aka yi la'akari da haɗarin kamuwa da cutar sankarar prostate mai tsanani, wani binciken haɗin gwiwar genome-wide (GWAS) na 12,518 ciwon daji na prostate ya gano loci biyu da ke hade da babban Gleason jimlar, SNP rs78943174 mafi kusa da gene NAALADL2 da SNP. rs35148638 kusa da RASA1 . [43]
Abincin abinci
[gyara sashe | gyara masomin]An gano cin 'ya'yan itatuwa da kayan marmari ba su da fa'ida kaɗan. [44] Wasu nazarin sun ba da rahoton cewa yawan cin nama yana da alaƙa da haɗari mafi girma. [45]
Shan madara na iya kasancewa yana da alaƙa da kansar prostate.[46][47] Wani bita na tsari na 2020 ya gano sakamakon kan shan madara da cutar kansar prostate bai cika ba amma ya bayyana cewa mutanen da ke da haɗari mafi girma na iya rage ko kawar da madara.[48] Wani bayyani na shekarar 2019 ya bayyana cewa shaidar da ta danganta madara da yawan ciwon daji na prostate bai dace ba kuma bai dace ba.[49] Wani bincike da aka yi a shekarar 2021 daga Japan yana duban maza 26,464 ya gano cewa shan madara ya kara barazanar kamuwa da cutar sankara ta prostate da kashi 37%.[50]
Ƙananan matakan bitamin D na iya ƙara haɗari.[51] Ɗaya daga cikin binciken bai sami wani tasiri na kariyar folic acid akan haɗari ba.[52]
Bayyanar magani
[gyara sashe | gyara masomin]An kafa wasu hanyoyin haɗin gwiwa tsakanin ciwon daji na prostate da magunguna, hanyoyin likita, da yanayin likita.[53] Statins na iya rage haɗari.[54]
Kamuwa da cuta
[gyara sashe | gyara masomin]Prostatitis ( kamuwa da cuta ko kumburi ) na iya ƙara haɗari. Musamman, kamuwa da cututtukan da ake ɗauka ta hanyar jima'i Chlamydia, gonorrhea, ko syphilis yana da alama yana ƙara haɗari. [55]
An ba da shawarar kwayar cutar papilloma don samun rawar da za ta taka, amma tun daga 2015, shaidar ba ta cika ba;[56] kamar na 2018, an yi muhawara game da haɗarin haɗari.[57]
Muhalli
[gyara sashe | gyara masomin]Tsohon sojan Amurka wadanda aka fallasa ga Agent Orange sun sami karuwar 48% na haɗarin kamuwa da cutar kansar prostate bayan tiyata.
Jima'i
[gyara sashe | gyara masomin]Ko da yake wasu shaidu daga binciken ƙungiyoyi masu zuwa na nuna cewa yawan maniyyi na iya rage haɗarin ciwon gurguwar prostate,[58] ba wani gwajin da aka sarrafa ba ya ruwaito wannan fa'ida.[59] An sami wata ƙungiya tsakanin vasectomy da ciwon gurguwar prostate, amma ba'a kafa dalili ba.[60]
Pathophysiology
[gyara sashe | gyara masomin]
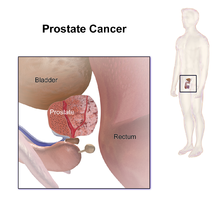
Prostate wani bangare ne na tsarin haihuwa na namiji wanda ke taimakawa wajen yin da kuma adana ruwan sha . A cikin manya maza, prostate na yau da kullun yana kusan 3 cm tsayi kuma yayi kimanin 20 g.[61] Yana cikin ƙashin ƙugu, ƙarƙashin mafitsara na fitsari da kuma gaban dubura . Prostate yana kewaye wani yanki na urethra, bututun da ke ɗaukar fitsari daga mafitsara yayin fitsari da maniyyi yayin fitar maniyyi . [62] Prostate yana ƙunshe da ƙananan ƙwayoyin cuta masu yawa waɗanda ke yin kusan kashi 20% na ruwan da ya zama maniyyi .[63]
Fiye da haka, gindin prostate yana haɗuwa tare da hanyar mafitsara. A mafi ƙanƙanta, koli na prostate yana kaiwa zuwa ga diaphragm na urogenital, wanda aka nuna a baya-ƙananan. Za a iya raba prostate zuwa wurare huɗu na jiki: na gefe, na tsakiya, na tsaka-tsaki, da kuma fibromuscular stroma na gaba.[64] Wurin da ke gefen ya ƙunshi ɓangarori na baya da na gefe na prostate, da kuma ƙananan sassan prostate. Wurin tsakiya ya ƙunshi mafi girman ɓangaren prostate ciki har da mafi kusancin bangarorin urethra da wuyan mafitsara. Wurin juzu'i yana gaban tsakiyar sararin samaniya kuma ya haɗa da nisa daga urethra zuwa tsakiyar urethra. Hanyar daurewar jijiyoyin jini tare da saman prostate na baya kuma yana shiga cikin capsule na prostatic a can kuma.
Yawancin nau'in glandular ana samun su a cikin yankuna na tsakiya da na tsakiya (yankin gefe: 70-80% na nama na glandular; yankin tsakiya: 20% na nama na glandular).[65] Ana samun wasu a cikin sararin tsaka-tsaki (5% na nama na glandular). Don haka, yawancin ciwon daji da ke tasowa daga nama na glandular ana samun su a wurare na gefe da na tsakiya,[66] yayin da kusan kashi 5% ana samun su a sararin tsaka-tsakin. Babu wani abu da aka samo a cikin fibromuscular stroma na baya tun da babu glandan da ke cikin wannan sararin samaniya.

Glandar prostate suna buƙatar hormones na maza, wanda aka sani da androgens, don yin aiki da kyau. Androgens sun hada da testosterone, wanda aka yi a cikin gwaje- gwaje ; dehydroepiandrosterone, sanya a cikin adrenal gland ; da dihydrotestosterone, wanda aka canza daga testosterone a cikin prostate kanta. Androgens kuma suna da alhakin halayen halayen jima'i na biyu kamar gashin fuska da ƙara yawan ƙwayar tsoka.

Saboda wurin wurin prostate, cututtukan prostate sukan shafi fitsari, fitar maniyyi, da kuma rashin bayan gida . A cikin ciwon daji na prostate, ƙwayoyin waɗannan gland suna canzawa zuwa ƙwayoyin kansa.
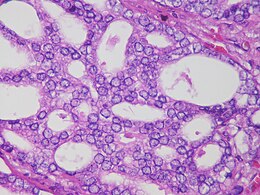
Yawancin ciwon daji na prostate ana rarraba su a matsayin adenocarcinomas, ko ciwon daji na glandular, wanda ke farawa lokacin da kwayoyin glandular masu ɓoye maniyyi suka canza zuwa kwayoyin cutar kansa. Yankin glandan prostate inda adenocarcinoma ya fi kowa shine yankin na gefe. Da farko, ƙananan ƙumburi na ƙwayoyin cutar kansa suna kasancewa a cikin in ba haka ba glandan prostate na yau da kullun, yanayin da aka sani da carcinoma a wurin ko prostatic intraepithelial neoplasia (PIN). Kodayake babu wata hujja da ta tabbatar da cewa PIN shine farkon ciwon daji, yana da alaƙa da kansa sosai. Bayan lokaci, waɗannan ƙwayoyin suna haɓaka kuma suna bazuwa zuwa ƙwayoyin prostate da ke kewaye ( stroma ) suna samar da ƙari .
A ƙarshe, ƙwayar cuta na iya girma girma isa ya mamaye gabobin da ke kusa da su kamar ƙwayoyin jini na jini ko dubura, ko ƙwayoyin tumo na iya haɓaka ikon yin tafiya a cikin jini da tsarin lymphatic .
Ana ɗaukar ciwon daji na prostate a matsayin mummunan ƙari saboda yana iya mamaye wasu sassan jiki. Ana kiran wannan mamayewar metastasis . Ciwon daji na prostate ya fi ƙaura zuwa ƙasusuwa da nodes na lymph, kuma yana iya mamaye dubura, mafitsara, da ƙananan ureters bayan ci gaban gida. Ana tunanin hanyar metastasis zuwa kashi venous ne, kamar yadda prostatic venous plexus yana zubar da prostate yana haɗuwa da veins na kashin baya.[67]
Prostate wata kwayar halitta ce mai tara zinc, mai samar da citrate . Sufurin gina jiki ZIP1 ne ke da alhakin jigilar zinc cikin ƙwayoyin prostate. Ɗaya daga cikin muhimman ayyuka na zinc shine canza canjin tantanin halitta don samar da citrate, muhimmin bangaren maniyyi. Tsarin tarawa na zinc, sauye-sauye na metabolism, da samar da citrate ba makamashi ba ne, kuma kwayoyin prostate suna buƙatar makamashi mai yawa ( ATP ) don cim ma wannan aikin. Kwayoyin cutar kansar prostate gabaɗaya ba su da zinc. Kwayoyin ciwon daji na Prostate suna adana kuzari ta hanyar rashin yin citrate, kuma suna amfani da makamashin da aka adana don girma, haifuwa da yadawa.
Ana tunanin rashin zinc yana faruwa ta hanyar yin shiru da kwayar halittar da ke samar da ZIP1. Ana kiransa samfurin ƙwayar ƙwayar ƙwayar ƙwayar cuta don kwayar halitta SLC39A1 . Ba a san dalilin yin shiru na epigenetic ba. Dabarun da ke jigilar zinc zuwa ƙwayoyin prostate da suka canza yadda ya kamata suna kawar da waɗannan kwayoyin halitta a cikin dabbobi. Zinc yana hana hanyoyin NF-κB, yana hana haɓakawa, kuma yana haifar da apoptosis a cikin ƙwayoyin da ba su da kyau. Abin baƙin ciki shine, shigar da baki na zinc ba shi da tasiri tun da yawan adadin zinc a cikin ƙwayoyin prostate ba zai yiwu ba sai da ZIP1. [68]
Asarar kwayoyin cutar ciwon daji, da farko a cikin carcinogenesis na prostate, an sanya su zuwa chromosomes 8p, 10q, 13q, da 16q . Maye gurbi na P53 a cikin ciwon daji na prostate na farko yana da ɗan ƙaramin ƙarfi kuma ana yawan gani akai-akai a cikin saitunan metastatic, saboda haka, maye gurbi na p53 wani lamari ne na marigayi a cikin ilimin cututtuka. Sauran kwayoyin halittar da ke hana ciwace-ciwace da ake tunanin za su taka rawa sun hada da PTEN da KAI1 . "Kusan kashi 70 cikin 100 na maza masu fama da cutar kansar prostate sun rasa kwafin kwayar halittar PTEN guda daya a lokacin da aka gano cutar."[69] An kuma lura da mitar asarar E-cadherin da CD44 . Asarar furotin na retinoblastoma (RB) yana haifar da raguwar masu karɓar mai karɓa na androgen a cikin ciwon gurguwar ƙwayar cuta mai jurewa ta hanyar rage furucin E2F1 .[70]
Abubuwan da ke haifar da ci gaban cuta da tsinkayen asibiti sun kasance a ɗan fahimta kaɗan kawai amma an gano nau'ikan abubuwan tantance ƙwayoyin ƙwayoyin cuta waɗanda da alama suna da hannu. Mafi mahimmancin waɗannan na iya zama tyrosine phosphatase ACP1 wanda furucin zai iya fin karfin tsarin Gleason don tsinkayar cutar.[71] Sauran kwayoyin da aka gano sun haɗa da nau'in rubutun RUNX2 wanda zai iya hana kwayoyin cutar kansa daga yin apoptosis,[72] PI3k/Akt mai siginar sigina tare da haɓakar haɓakar haɓakar beta / SMAD siginar cascade wanda kuma yana kare kariya daga apoptosis.[73] An inganta Pim-1 a cikin ciwon daji na prostate. X-linked inhibitor na apoptosis ( XIAP ) an yi la'akari da shi don inganta rayuwa da ci gaban ciwon daji,[74] cytokine-1 (MIC-1) mai hanawa Macrophage wanda ke ƙarfafa hanyar adhesion kinase (FAK) mai mahimmanci.[75] Duk da haka, yana da kyau a faɗi cewa abubuwan da ke tabbatar da dalilin da yasa wasu marasa lafiya ke fama da rashin lafiya yayin da sauran tsinkayen nunin sun kasance a ɓoye.
Mai karɓar androgen yana taimakawa ƙwayoyin kansa don tsira.[76] Prostate-specific membrane antigen (PSMA) yana ƙarfafa ci gaban kansa ta hanyar haɓaka matakan folate, yana taimakawa ƙwayoyin kansa su rayu da girma; yana ƙara yawan folates don amfani ta hanyar hydrolyzing folates glutamated.[77]
Bincike
[gyara sashe | gyara masomin]
Matsayin Ƙungiyar Ciwon daji ta Amirka game da gano wuri ta gwajin PSA shine:
Har yanzu bincike bai tabbatar da cewa yuwuwar amfanin gwaji ya fi illar gwaji da magani ba. Ƙungiyar Ciwon daji ta Amurka ta yi imanin cewa bai kamata a gwada maza ba tare da koyo game da abin da muka sani ba kuma ba mu sani ba game da haɗari da yiwuwar amfani da gwaji da magani. Tun yana da shekaru 50, (45 idan Ba'amurke ɗan Afirka ko ɗan'uwa ko uba ya sha wahala daga yanayin kafin shekaru 65) yi magana da likitan ku game da ribobi da fursunoni na gwaji don ku iya yanke shawara idan gwajin shine zaɓin da ya dace a gare ku.
Ana iya amfani da wasu gwaje-gwaje da yawa don tattara bayanai game da prostate da kuma urinary fili. Binciken duburar dijital na iya ƙyale likita ya gano rashin daidaituwa na prostate. Cystoscopy yana nuna hanyar fitsari daga cikin mafitsara, ta yin amfani da siriri, bututun kyamara mai sassauƙa da aka saka a cikin urethra . Ultrasonography na transrectal yana haifar da hoto na prostate ta amfani da raƙuman sauti daga bincike a cikin dubura, amma kawai gwajin da zai iya tabbatar da cikakken ganewar ciwon daji na prostate shine biopsy, cire ƙananan ƙwayar prostate don nazarin microscopic.
Hoto
[gyara sashe | gyara masomin]Duban dan tayi da magnetic resonance imaging (MRI) su ne manyan hanyoyin hoto guda biyu da ake amfani da su don gano kansar prostate.
MRI
[gyara sashe | gyara masomin]Bayyanar prostate akan MRI
[gyara sashe | gyara masomin]A kan MRI, yankuna na tsakiya da na tsaka-tsaki duka suna da ƙananan siginar T2 fiye da yanki na gefe. Tun da yankunan tsakiya da na tsaka-tsaki ba za a iya bambanta da juna ba, za a iya kwatanta su da kyau a matsayin ƙwayar tsakiya a kan MRI. Don haka, ƙwayar ƙwayar cuta tana da sigina mafi girma akan T2WI fiye da gland na tsakiya. A cikin gland shine ciwon daji na prostate yana bayyana azaman rauni mai rauni . Duk da haka, a cikin ƙananan ƙwayar cuta, ƙananan ƙananan ƙwayoyin cuta ba za a iya bambanta su da ƙananan ƙananan ƙwayar cuta ba. Ƙuntatawar yaduwa yana da kayan aiki don ganowa da kuma kwatanta raunuka na tsakiya. Haɗe-haɗe-haɗe-haɗe-nauyin (DW) hoto da ƙwaƙƙwaran haɓaka-madaidaicin MRI don bambance m daga raunin prostate mara kyau za a iya amfani da su. Hotunan da aka haɗe, na DW da MRI tare da haɓaka bambanci mai ƙarfi, na iya hango wuraren da ke da ƙananan sigina da tasirin wankewa da sauri - halayyar carcinomas. [78] Ana iya ganin Lymphadenopathy mafi kyau akan postcontrast, T1WI mai kitse. Ana iya kwatanta wasu yankuna akan MRI. Ƙwararrun fibromuscular na baya da ƙwayar prostate tare da prostate na baya da na gefe suna da ƙananan siginar T2WI, sabanin siginar haske na yanki na gefe. Za'a iya ganin tsawaitawar prostatic tare da rushewar ingancin capsule.
MRI don gano ciwon daji na prostate
[gyara sashe | gyara masomin]Tun daga shekara ta 2011, an yi amfani da MRI don gano maƙasudi don biopsy na prostate ta amfani da MRI fusion tare da duban dan tayi (US) ko Jagorar MRI kadai. MRI kadai zai gano daidai kashi 91 cikin dari na maza masu fama da cutar sankarar prostate a asibiti amma zai yi kuskuren rarraba kashi 63 cikin dari na maza masu hadarin kamuwa da ciwon gurguwar prostate kamar ciwon daji na prostate.[79] Wani biopsy da aka yi niyya na MRI zai gano daidai kashi 80 cikin 100 na maza masu ciwon prostate. Koyaya, zai rarraba kashi 6% na maza masu haɗarin kamuwa da cutar kansar prostate a matsayin suna da cutar kansar prostate a asibiti. An nuna alamun ciwon daji maras muhimmanci a asibiti lokacin da aka haɗu da kwayar cutar ta MRI tare da daidaitattun kwayoyin halitta ga maza tare da sakamako mai kyau akan MRI, idan aka kwatanta da daidaitattun hanyar biopsy.[80]
Bayan MRI, yankuna masu sha'awa a cikin binciken wanda zai iya zama ciwon daji ana yawan ƙididdige su akan ma'auni tsakanin 1 da 5. Ɗaya daga cikin irin wannan ma'auni shine prostate Hoto-reporting and Data System (PI-RADS) ma'auni wanda ke bayyana ma'auni na sabis na asibiti don multiparametric MRI (mpMRI), ciki har da ƙirƙirar hoto da rahoto. Maki na PI-RADS sigar 2 ya nuna ƙayyadaddun ƙayyadaddun ƙima da azanci na 73% da 95%, bi da bi, don gano kansar prostate.[81]
Lokacin da aka yi amfani da MRI don yanke shawarar ko za a yi biopsy a cikin maza da suka rigaya sun rigaya, yana da 5% mafi kusantar yin ganewar asali fiye da daidaitattun kwayoyin halitta kuma yana da 12% mafi kusantar zama daidai ga maza waɗanda zasu iya ko. maiyuwa ba a sami riga-kafin biopsy ba. A cikin mazan da suka sami biopsy mara kyau, wannan haɗin yana da 44% mafi kusantar haifar da ganewar asali.
Manazarta
[gyara sashe | gyara masomin]- ↑ "Prostate Cancer". National Cancer Institute. January 1980. Archived from the original on 12 October 2014. Retrieved 12 October 2014.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 "Prostate Cancer Treatment (PDQ) – Health Professional Version". National Cancer Institute. 2014-04-11. Archived from the original on 5 July 2014. Retrieved 1 July 2014.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 "Chapter 5.11". World Cancer Report. World Health Organization. 2014. ISBN 978-9283204299.
- ↑ Ruddon, Raymond W. (2007). Cancer biology (4th ed.). Oxford: Oxford University Press. p. 223. ISBN 978-0195175431. Archived from the original on 2015-09-15.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 "Prostate Cancer Treatment (PDQ) – Patient Version". National Cancer Institute. 2014-04-08. Archived from the original on 5 July 2014. Retrieved 1 July 2014.
- ↑ Caini S, Gandini S, Dudas M, Bremer V, Severi E, Gherasim A (August 2014). "Sexually transmitted infections and prostate cancer risk: a systematic review and meta-analysis". Cancer Epidemiology. 38 (4): 329–38. doi:10.1016/j.canep.2014.06.002. PMID 24986642.
- ↑ Lee MV, Katabathina VS, Bowerson ML, Mityul MI, Shetty AS, Elsayes KM, et al. (2016). "BRCA-associated Cancers: Role of Imaging in Screening, Diagnosis, and Management". Radiographics. 37 (4): 1005–1023. doi:10.1148/rg.2017160144. PMID 28548905.
- ↑ 8.0 8.1 "Prostate Cancer Treatment". National Cancer Institute (in Turanci). 6 February 2018. Retrieved 1 March 2018.
Controversy exists regarding the value of screening... reported no clear evidence that screening for prostate cancer decreases the risk of death from prostate cancer
- ↑ Catalona WJ (March 2018). "Prostate Cancer Screening". The Medical Clinics of North America. 102 (2): 199–214. doi:10.1016/j.mcna.2017.11.001. PMC 5935113. PMID 29406053.
- ↑ "PSA testing". nhs.uk. 3 January 2015. Retrieved 5 March 2018.
- ↑ "Final Recommendation Statement: Prostate Cancer: Screening – US Preventive Services Task Force". www.uspreventiveservicestaskforce.org (in Turanci). USPSTF. Retrieved 30 August 2018.
- ↑ Grossman DC, Curry SJ, Owens DK, Bibbins-Domingo K, Caughey AB, Davidson KW, et al. (May 2018). "Screening for Prostate Cancer: US Preventive Services Task Force Recommendation Statement". JAMA. 319 (18): 1901–1913. doi:10.1001/jama.2018.3710. PMID 29801017.
- ↑ Cabarkapa S, Perera M, McGrath S, Lawrentschuk N (December 2016). "Prostate cancer screening with prostate-specific antigen: A guide to the guidelines". Prostate International. 4 (4): 125–129. doi:10.1016/j.prnil.2016.09.002. PMC 5153437. PMID 27995110.
- ↑ Stratton J, Godwin M (June 2011). "The effect of supplemental vitamins and minerals on the development of prostate cancer: a systematic review and meta-analysis". Family Practice. 28 (3): 243–52. doi:10.1093/fampra/cmq115. PMID 21273283.
- ↑ "SEER Stat Fact Sheets: Prostate Cancer". NCI. Archived from the original on 6 July 2014. Retrieved 18 June 2014.
- ↑ "Chapter 1.1". World Cancer Report. World Health Organization. 2014. ISBN 978-9283204299.
- ↑ Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (November 2018). "Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries". Ca: A Cancer Journal for Clinicians. 68 (6): 394–424. doi:10.3322/caac.21492. PMID 30207593.
- ↑ 18.0 18.1 Baade PD, Youlden DR, Krnjacki LJ (February 2009). "International epidemiology of prostate cancer: geographical distribution and secular trends". Molecular Nutrition & Food Research. 53 (2): 171–84. doi:10.1002/mnfr.200700511. PMID 19101947.
- ↑ Baade PD, Youlden DR, Krnjacki LJ (February 2009). "International epidemiology of prostate cancer: geographical distribution and secular trends". Molecular Nutrition & Food Research. 53 (2): 171–84. doi:10.1002/mnfr.200700511. PMID 19101947.
- ↑ Leslie SW, Soon-Sutton TL, Sajjad H, Siref LE. Prostate Cancer. 2020 Oct 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; Samfuri:PMID.
- ↑ Miller DC, Hafez KS, Stewart A, Montie JE, Wei JT (September 2003). "Prostate carcinoma presentation, diagnosis, and staging: an update form the National Cancer Data Base" (PDF). Cancer. 98 (6): 1169–78. doi:10.1002/cncr.11635. hdl:2027.42/34379. PMID 12973840. S2CID 22077473.
- ↑ van der Cruijsen-Koeter IW, Vis AN, Roobol MJ, Wildhagen MF, de Koning HJ, van der Kwast TH, Schröder FH (July 2005). "Comparison of screen detected and clinically diagnosed prostate cancer in the European randomized study of screening for prostate cancer, section rotterdam". The Journal of Urology. 174 (1): 121–5. doi:10.1097/01.ju.0000162061.40533.0f. PMID 15947595.
- ↑ Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ (April 2003). "Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults". The New England Journal of Medicine. 348 (17): 1625–38. doi:10.1056/NEJMoa021423. PMID 12711737. S2CID 22714795.
- ↑ Hankey BF, Feuer EJ, Clegg LX, Hayes RB, Legler JM, Prorok PC, et al. (June 1999). "Cancer surveillance series: interpreting trends in prostate cancer--part I: Evidence of the effects of screening in recent prostate cancer incidence, mortality, and survival rates". Journal of the National Cancer Institute. 91 (12): 1017–24. doi:10.1093/jnci/91.12.1017. PMID 10379964.
- ↑ Breslow N, Chan CW, Dhom G, Drury RA, Franks LM, Gellei B, et al. (November 1977). "Latent carcinoma of prostate at autopsy in seven areas. The International Agency for Research on Cancer, Lyons, France". International Journal of Cancer. 20 (5): 680–8. doi:10.1002/ijc.2910200506. PMID 924691. S2CID 42501757.
- ↑ Bell KJ, Del Mar C, Wright G, Dickinson J, Glasziou P (October 2015). "Prevalence of incidental prostate cancer: A systematic review of autopsy studies". International Journal of Cancer. 137 (7): 1749–57. doi:10.1002/ijc.29538. PMC 4682465. PMID 25821151.
- ↑ Jahn JL, Giovannucci EL, Stampfer MJ (December 2015). "The high prevalence of undiagnosed prostate cancer at autopsy: implications for epidemiology and treatment of prostate cancer in the Prostate-specific Antigen-era". International Journal of Cancer. 137 (12): 2795–802. doi:10.1002/ijc.29408. PMC 4485977. PMID 25557753.
- ↑ Martin RM, Vatten L, Gunnell D, Romundstad P (March 2010). "Blood pressure and risk of prostate cancer: Cohort Norway (CONOR)". Cancer Causes & Control. 21 (3): 463–72. doi:10.1007/s10552-009-9477-x. PMID 19949849. S2CID 30484327.
- ↑ Friedenreich CM, Neilson HK, Lynch BM (September 2010). "State of the epidemiological evidence on physical activity and cancer prevention". European Journal of Cancer. 46 (14): 2593–604. doi:10.1016/j.ejca.2010.07.028. PMID 20843488.
- ↑ Gann PH, Hennekens CH, Ma J, Longcope C, Stampfer MJ (August 1996). "Prospective study of sex hormone levels and risk of prostate cancer". Journal of the National Cancer Institute. 88 (16): 1118–26. doi:10.1093/jnci/88.16.1118. PMID 8757191.
- ↑ "Prostate cancer". Genetics Home Reference (in Turanci). Retrieved 1 May 2020.
- ↑ Steinberg GD, Carter BS, Beaty TH, Childs B, Walsh PC (1990). "Family history and the risk of prostate cancer". The Prostate. 17 (4): 337–47. doi:10.1002/pros.2990170409. PMID 2251225. S2CID 44925478.
- ↑ Zeegers MP, Jellema A, Ostrer H (April 2003). "Empiric risk of prostate carcinoma for relatives of patients with prostate carcinoma: a meta-analysis". Cancer. 97 (8): 1894–903. doi:10.1002/cncr.11262. PMID 12673715. S2CID 12607885.
- ↑ Gallagher RP, Fleshner N (October 1998). "Prostate cancer: 3. Individual risk factors" (PDF). CMAJ. 159 (7): 807–13. PMC 1232741. PMID 9805030. Archived (PDF) from the original on 2009-12-29.
- ↑ Hoffman RM, Gilliland FD, Eley JW, Harlan LC, Stephenson RA, Stanford JL, et al. (March 2001). "Racial and ethnic differences in advanced-stage prostate cancer: the Prostate Cancer Outcomes Study". Journal of the National Cancer Institute. 93 (5): 388–95. doi:10.1093/jnci/93.5.388. PMID 11238701.
- ↑ Lichtenstein P, Holm NV, Verkasalo PK, Iliadou A, Kaprio J, Koskenvuo M, et al. (July 2000). "Environmental and heritable factors in the causation of cancer--analyses of cohorts of twins from Sweden, Denmark, and Finland". The New England Journal of Medicine. 343 (2): 78–85. doi:10.1056/NEJM200007133430201. PMID 10891514.
- ↑ Struewing JP, Hartge P, Wacholder S, Baker SM, Berlin M, McAdams M, et al. (May 1997). "The risk of cancer associated with specific mutations of BRCA1 and BRCA2 among Ashkenazi Jews". The New England Journal of Medicine. 336 (20): 1401–8. doi:10.1056/NEJM199705153362001. PMID 9145676.
- ↑ Beuzeboc P, Soulié M, Richaud P, Salomon L, Staerman F, Peyromaure M, et al. (December 2009). "[Fusion genes and prostate cancer. From discovery to prognosis and therapeutic perspectives]". Progres en Urologie (in Faransanci). 19 (11): 819–24. doi:10.1016/j.purol.2009.06.002. PMID 19945666.
- ↑ Baca SC, Prandi D, Lawrence MS, Mosquera JM, Romanel A, Drier Y, et al. (April 2013). "Punctuated evolution of prostate cancer genomes". Cell. 153 (3): 666–77. doi:10.1016/j.cell.2013.03.021. PMC 3690918. PMID 23622249.
- ↑ Eeles RA, Kote-Jarai Z, Giles GG, Olama AA, Guy M, Jugurnauth SK, et al. (March 2008). "Multiple newly identified loci associated with prostate cancer susceptibility". Nature Genetics. 40 (3): 316–21. doi:10.1038/ng.90. PMID 18264097. S2CID 30968525.
- ↑ Thomas G, Jacobs KB, Yeager M, Kraft P, Wacholder S, Orr N, et al. (March 2008). "Multiple loci identified in a genome-wide association study of prostate cancer". Nature Genetics. 40 (3): 310–5. doi:10.1038/ng.91. PMID 18264096. S2CID 22978381.
- ↑ Whitaker HC, Kote-Jarai Z, Ross-Adams H, Warren AY, Burge J, George A, et al. (October 2010). Vickers A (ed.). "The rs10993994 risk allele for prostate cancer results in clinically relevant changes in microseminoprotein-beta expression in tissue and urine". PLOS ONE. 5 (10): e13363. Bibcode:2010PLoSO...513363W. doi:10.1371/journal.pone.0013363. PMC 2954177. PMID 20967219.
- ↑ Berndt SI, Wang Z, Yeager M, Alavanja MC, Albanes D, Amundadottir L, et al. (May 2015). "Two susceptibility loci identified for prostate cancer aggressiveness". Nature Communications. 6: 6889. Bibcode:2015NatCo...6.6889.. doi:10.1038/ncomms7889. PMC 4422072. PMID 25939597.
- ↑ Venkateswaran V, Klotz LH (August 2010). "Diet and prostate cancer: mechanisms of action and implications for chemoprevention". Nature Reviews. Urology. 7 (8): 442–53. doi:10.1038/nrurol.2010.102. PMID 20647991. S2CID 10602814.
- ↑ "Chemicals in Meat Cooked at High Temperatures and Cancer Risk". National Cancer Institute. 2018-04-02. Archived from the original on 2011-11-06.
- ↑ "Milk and Health". American College of Cardiology. Retrieved 2021-02-21.
- ↑ Willett WC, Ludwig DS (February 2020). "Milk and Health". The New England Journal of Medicine. 382 (7): 644–654. doi:10.1056/NEJMra1903547. PMID 32053300. S2CID 211099544.
- ↑ Sargsyan A, Dubasi HB (July 2020). "Milk Consumption and Prostate Cancer: A Systematic Review". The World Journal of Men's Health. 38 (3): 419–428. doi:10.5534/wjmh.200051. PMC 8255404 Check
|pmc=value (help). PMID 32777868. - ↑ López-Plaza B, Bermejo LM, Santurino C, Cavero-Redondo I, Álvarez-Bueno C, Gómez-Candela C (May 2019). "Milk and dairy product consumption and prostate cancer risk and mortality: an overview of systematic reviews and meta-analyses". Adv Nutr. 10 (suppl_2): S212–S223. doi:10.1093/advances/nmz014. PMC 6518142. PMID 31089741.
- ↑ Mikami, K.; Ozasa, K.; Miki, T.; Watanabe, Y.; Mori, M.; Kubo, T.; Suzuki, K.; Wakai, K.; Nakao, M.; Tamakoshi, A.; JACC Study Group (2021). "Dairy products and the risk of developing prostate cancer: A large-scale cohort study (JACC Study) in Japan". Cancer Medicine. 10 (20): 7298–7307. doi:10.1002/cam4.4233. PMC 8525158 Check
|pmc=value (help). PMID 34606688 Check|pmid=value (help). S2CID 238358096 Check|s2cid=value (help). - ↑ Wigle DT, Turner MC, Gomes J, Parent ME (March 2008). "Role of hormonal and other factors in human prostate cancer". Journal of Toxicology and Environmental Health Part B: Critical Reviews. 11 (3–4): 242–59. doi:10.1080/10937400701873548. PMID 18368555. S2CID 24489849.
- ↑ Qin X, Cui Y, Shen L, Sun N, Zhang Y, Li J, et al. (September 2013). "Folic acid supplementation and cancer risk: a meta-analysis of randomized controlled trials". International Journal of Cancer. 133 (5): 1033–41. doi:10.1002/ijc.28038. PMID 23338728. S2CID 19830376.
- ↑ Jacobs EJ, Rodriguez C, Mondul AM, Connell CJ, Henley SJ, Calle EE, Thun MJ (July 2005). "A large cohort study of aspirin and other nonsteroidal anti-inflammatory drugs and prostate cancer incidence". Journal of the National Cancer Institute. 97 (13): 975–80. doi:10.1093/jnci/dji173. PMID 15998950.
- ↑ Shannon J, Tewoderos S, Garzotto M, Beer TM, Derenick R, Palma A, Farris PE (August 2005). "Statins and prostate cancer risk: a case-control study". American Journal of Epidemiology. 162 (4): 318–25. doi:10.1093/aje/kwi203. PMID 16014776.
- ↑ Dennis LK, Lynch CF, Torner JC (July 2002). "Epidemiologic association between prostatitis and prostate cancer". Urology. 60 (1): 78–83. doi:10.1016/S0090-4295(02)01637-0. PMID 12100928.
- ↑ Heidegger I, Borena W, Pichler R (May 2015). "The role of human papilloma virus in urological malignancies". Anticancer Research. 35 (5): 2513–9. PMID 25964524.
- ↑ Cai T, Di Vico T, Durante J, Tognarelli A, Bartoletti R (December 2018). "Human papilloma virus and genitourinary cancers: a narrative review". Minerva Urologica e Nefrologica. 70 (6): 579–587. doi:10.23736/S0393-2249.18.03141-7. PMID 30160386. S2CID 52118310.
- ↑ Rider JR, Wilson KM, Sinnott JA, Kelly RS, Mucci LA, Giovannucci EL (December 2016). "Ejaculation Frequency and Risk of Prostate Cancer: Updated Results with an Additional Decade of Follow-up". European Urology. 70 (6): 974–982. doi:10.1016/j.eururo.2016.03.027. PMC 5040619. PMID 27033442.
- ↑ Aboul-Enein BH, Bernstein J, Ross MW (July 2016). "Evidence for Masturbation and Prostate Cancer Risk: Do We Have a Verdict?". Sexual Medicine Reviews. 4 (3): 229–234. doi:10.1016/j.sxmr.2016.02.006. PMID 27871956.
- ↑ "A comprehensive cancer control program for BC". Retrieved 2 November 2021.
- ↑ Aumüller G (1979). Prostate Gland and Seminal Vesicles. Berlin-Heidelberg: Springer-Verlag.
- ↑ Moore KL, Chubb D (1999). Clinically Oriented Anatomy. Baltimore, Maryland: Lippincott Williams & Wilkins. ISBN 978-0-683-06132-1.
- ↑ Steive H (1930). "Männliche Genitalorgane". Handbuch der mikroskopischen Anatomie des Menschen. Vol. VII Part 2. Berlin: Springer. pp. 1–399.
- ↑ McNeal JE (1984). "Anatomy of the prostate and morphogenesis of BPH". Progress in Clinical and Biological Research. 145: 27–53. PMID 6201879.
- ↑ Oh WK, Hurwitz M, D'Amico AV, Richie JP, Kantoff PW (2003). "Biology of Prostate Cancer". Holland-Frei Cancer Medicine (in Turanci) (6th ed.).
- ↑ Reissigl A, Pointner J, Strasser H, Ennemoser O, Klocker H, Bartsch G (February 1997). "Frequency and clinical significance of transition zone cancer in prostate cancer screening". The Prostate. 30 (2): 130–5. doi:10.1002/(SICI)1097-0045(19970201)30:2<130::AID-PROS8>3.0.CO;2-S. PMID 9051151.
- ↑ "Male Genitals – Prostate Neoplasms". Pathology study images. University of Virginia School of Medicine. Archived from the original on 2011-07-20. Retrieved 2011-04-28.
There are many connections between the prostatic venous plexus and the vertebral veins. The veins forming the prostatic plexus do not contain valves and it is thought that straining to urinate causes prostatic venous blood to flow in a reverse direction and enter the vertebral veins carrying malignant cells to the vertebral column.
- ↑ Costello LC, Franklin RB (May 2006). "The clinical relevance of the metabolism of prostate cancer; zinc and tumor suppression: connecting the dots". Molecular Cancer. 5: 17. doi:10.1186/1476-4598-5-17. PMC 1481516. PMID 16700911.
- ↑ "Scientists Discover Anti-Cancer Mechanism that Arrests Early Prostate Cancer". August 4, 2005. Archived from the original on May 19, 2008.
- ↑ Sharma A, Yeow WS, Ertel A, Coleman I, Clegg N, Thangavel C, et al. (December 2010). "The retinoblastoma tumor suppressor controls androgen signaling and human prostate cancer progression". The Journal of Clinical Investigation. 120 (12): 4478–92. doi:10.1172/JCI44239. PMC 2993601. PMID 21099110.
- ↑ Ruela-de-Sousa RR, Hoekstra E, Hoogland AM, Souza Queiroz KC, Peppelenbosch MP, Stubbs AP, Pelizzaro-Rocha K, van Leenders GJ, Jenster G, Aoyama H, Ferreira CV, Fuhler GM (April 2016). "Low-Molecular-Weight Protein Tyrosine Phosphatase Predicts Prostate Cancer Outcome by Increasing the Metastatic Potential". Eur Urol. 69 (4): 710–719. doi:10.1016/j.eururo.2015.06.040. PMID 26159288.
- ↑ Leav I, Plescia J, Goel HL, Li J, Jiang Z, Cohen RJ, et al. (January 2010). "Cytoprotective mitochondrial chaperone TRAP-1 as a novel molecular target in localized and metastatic prostate cancer". The American Journal of Pathology. 176 (1): 393–401. doi:10.2353/ajpath.2010.090521. PMC 2797899. PMID 19948822.
- ↑ Zha J, Huang YF (September 2009). "[TGF-beta/Smad in prostate cancer: an update]". Zhonghua Nan Ke Xue = National Journal of Andrology (in Harshen Sinanci). 15 (9): 840–3. PMID 19947572.
- ↑ Watanabe S, Miyata Y, Kanda S, Iwata T, Hayashi T, Kanetake H, Sakai H (May 2010). "Expression of X-linked inhibitor of apoptosis protein in human prostate cancer specimens with and without neo-adjuvant hormonal therapy". Journal of Cancer Research and Clinical Oncology. 136 (5): 787–93. doi:10.1007/s00432-009-0718-x. PMID 19946707. S2CID 34855148.
- ↑ Senapati S, Rachagani S, Chaudhary K, Johansson SL, Singh RK, Batra SK (March 2010). "Overexpression of macrophage inhibitory cytokine-1 induces metastasis of human prostate cancer cells through the FAK-RhoA signaling pathway". Oncogene. 29 (9): 1293–302. doi:10.1038/onc.2009.420. PMC 2896817. PMID 19946339.
- ↑ Narizhneva NV, Tararova ND, Ryabokon P, Shyshynova I, Prokvolit A, Komarov PG, et al. (December 2009). "Small molecule screening reveals a transcription-independent pro-survival function of androgen receptor in castration-resistant prostate cancer". Cell Cycle. 8 (24): 4155–67. doi:10.4161/cc.8.24.10316. PMC 2896895. PMID 19946220.
- ↑ Yao V, Berkman CE, Choi JK, O'Keefe DS, Bacich DJ (February 2010). "Expression of prostate-specific membrane antigen (PSMA), increases cell folate uptake and proliferation and suggests a novel role for PSMA in the uptake of the non-polyglutamated folate, folic acid". The Prostate. 70 (3): 305–16. doi:10.1002/pros.21065. PMID 19830782. S2CID 21518526.
- ↑ Georgiev, A. (2016). Case of prostate cancer with anterior localization - Multiparametric MRI study. Rentgenologiya i Radiologiya, 55(4), 285–87.
- ↑ Drost FH, Osses DF, Nieboer D, Steyerberg EW, Bangma CH, Roobol MJ, Schoots IG, et al. (Cochrane Urology Group) (April 2019). "Prostate MRI, with or without MRI-targeted biopsy, and systematic biopsy for detecting prostate cancer". The Cochrane Database of Systematic Reviews. 4: CD012663. doi:10.1002/14651858.CD012663.pub2. PMC 6483565. PMID 31022301.
- ↑ Eklund, Martin; Jäderling, Fredrik; Discacciati, Andrea; Bergman, Martin; Annerstedt, Magnus; Aly, Markus; Glaessgen, Axel; Carlsson, Stefan; Grönberg, Henrik; Nordström, Tobias (2021-09-02). "MRI-Targeted or Standard Biopsy in Prostate Cancer Screening". New England Journal of Medicine (in Turanci). 385 (10): 908–920. doi:10.1056/NEJMoa2100852. ISSN 0028-4793. PMID 34237810 Check
|pmid=value (help). - ↑ Wang X, Bao J, Ping X, Hu C, Hou J, Dong F, Guo L (September 2018). "The diagnostic value of PI-RADS V1 and V2 using multiparametric MRI in transition zone prostate clinical cancer". Oncology Letters. 16 (3): 3201–3206. doi:10.3892/ol.2018.9038. PMC 6096261. PMID 30127915.