Sankaran Nono
| Sankaran Nono | |
|---|---|
 | |
| Description (en) | |
| Iri |
thoracic cancer (en) cuta |
| Specialty (en) | oncology |
| Symptoms and signs (en) |
breast lump (en) lump in chest (en) |
| Physical examination (en) |
MammaPrint (en) |
| Genetic association (en) |
MAP3K1 (en) |
| Medical treatment (en) | |
| Magani |
ethinylestradiol (en) |
| Identifier (en) | |
| ICD-10-CM | C50 da C50-C50 |
| ICD-10 | C50 |
| OMIM | 114480 |
| DiseasesDB | 1598 |
| MedlinePlus | 000913 |
| eMedicine | 000913 |
| Disease Ontology ID | DOID:1612 |

Ciwon Kansa Na Nono sankarane ko ciwon daji da ke fitowa akan fatan nonon mata.[1] Alamomin ciwon daji na nono na iya haɗawa da dunƙulewar cikin ƙirji, canjin siffar nono, lotsewa ko rami a fatan. ruwan da kuma ke fitowa daga kan nono, sabon jujjuyawar nono, ko facin fata ko ja.[2]
kin masu yaɗuwar cutar mai nisa, ana iya samun ciwon ƙashi, kumburin ƙwayoyin lymph, ƙarancin numfashi, ko sauyawan launin fata zuwa rawaya.[3]
Abubuwan haɗari da ke janyo ciwon nono sun haɗa da kiba, rashin motsa jiki, shan barasa, sauyin sassan jiki a yayin da kuma aka dena ala,ada,radiation tarihin ciwon daji na nono, da kuma tarihin iyali na ciwon nono. Kimanin kashi 5-10% na lokuta sun samo asali ne daga yanayin halittar da aka gada daga iyaye,[2] [4] gami da BRCA1 da BRCA2 da sauransu.[2] Ciwon daji na nono ya fi tasowa a cikin sel daga rufin bututun nono da lobules waɗanda ke ba wa waɗannan bututun madara.[2] Ciwon daji da ke tasowa daga bututu ana kuma kiran su da turanci ductal carcinomas, yayin da waɗanda ke tasowa daga lobules an san su da lobular carcinomas. Akwai ire-iren ciwon daji na nono fiye da 18.[2] Wasu, irin su ductal carcinoma in situ, suna tasowa daga raunukan da suka rigaya.[2] Ana tabbatar da cutar kansar nono ta hanyar yin biopsy na abin da ya shafi nama (na nono).[4] Da zarar an gano cutar, ana ƙara yin wasu gwaje-gwaje don sanin ko ciwon ya yadu fiye da nono da kuma hanyoyin za'a bi don magance su.[2]
Akwai rudani sosai dangane da ma'auni na fa'ida da kuma lahani na gwajin cutar kansar nono. Wani bita da Cochrane ta gudanar a shekara ta 2013, ta gano cewa ba a sani ba idan gwajin mammographic ya fi cutarwa fiye da amfaninshi,[5] a cewa yawancin matan da aka nuna suna da cutar ta hanyar gwajin daga bisani kuma ba su kamu ba. Acikin wani bincike da kungyar United States Preventive Services Task Force ta gudanae a shekara ta 2009, ta tabbatar da fa'idar gwajin ga 'yan shekaru 40, zuwa 70,[6] sannan kuma kungiyar ta ba da shawarar gwaji duk bayan shekaru biyu ga mata 'yan shakera 50 zuwa 74.[7] Ana iya amfani da magungunan Tamoxifen ko raloxifene a ƙoƙarin kariya daga ciwon sankarar nono ga waɗanda ke cikin haɗarin kamuwa da cutar. Aikin asibiti na cire nonon wani ma'aunin kariya ne ga mata masu cuta wadanda ke cikin hadarin gaske.[8] Ga waɗanda aka gano cutar, ana iya amfani da hanyoyin kiwon lafiya da dama, ciki har da tiyata, radiation therapy, chemotherapy, hormonal therapy, da kuma targeted therapy. Nau'o'in tiyata sun bambanta daga tiyata don kiyaye nono zuwa Yanke nono - mastectomy. [9][10] Aikin gyaran nono na iya faruwa a lokacin tiyata ko kuma a wani lokaci na daban.[10] Ga wadanda cutar sankara ta yadu zuwa wasu sassan jiki, ana yin yawancin magungunansu ne don inganta rayuwa da karin natsuwa.[10]
Sakamakon ciwon nono sun bambanta dangane da nau'in ciwon dajin, girman cutar, da shekarun mutum. [11][12][13] Gwajin sauran rayuwa na shekaru biyar a Ingila da Amurka yana tsakanin 80, zuwa 90%. A ƙasashe masu tasowa, basu kai shekaru biyar sosai.[14] A duniya baki daya, ciwon nono shine kan gaba acikin nau'in sankara da ke addabar mata, wanda ke da kashi 25% na daukakin cutar. A cikin shekara ta 2018, an amu sabbin ciwukan kusan miliyan 2 da sanadiyyar mutuwar mata 627,000.[15] Ya fi yawa a ƙasashen da suka ci gaba kuma ya ninka sau 100, a cikin mata fiye da maza.[11][16]
Alamomi.
[gyara sashe | gyara masomin]

Ciwon daji na nono yawanci yana farawa ne a zaman wani dan kullutu wanda ya bambanta da sauran naman nono.[17] Ana gano fiye da kashi 80% na ciwon ne a lokacinda akai la'akari da wannan kullutu da yatsa. Farkon ciwon nono, duk da haka kuma, ana ganosu ne ta gwaji na mammogram.[18][19] Kullutun da ake samu a hammata ma na [17] iya zama alamun kansar nono.
Alamun cutar sankarar nono banda kullutu na iya haɗawa da kauri daban da sauran naman nono, nono ɗaya yafi daya girma ko kuma daya ya kankance, dan kan-nono na iya canza wuri, ko siffarsa ko juyawa, tsagewar fata ko rami, ko kuma kuraje a zagaye da kan-nono, fitar da ruwa daga nono, ciwo a wani sashe na nono ko hammata da kumburi a karkashin hammata ko kewayen kashin wuya. [20] Ciwo ("mastodynia") muhimmin alama ne na gano kasancewar sankarar nono, amma yana iya zama alamar wasu cututtukan nono na daban.[17][18][21]
Wani alamar cutar sankarar nono mai wuyar tantancewa shine cutar Paget na nono. Alamun cutan yana farawa ne ta hanyar sauyawan kalan fata kamar cutar eczema; kamar yin ja, canza launi ko laushin fata na nono. Yayin da cutar Paget na nono ke ci gaba, alamun cututtuka na iya haɗawa da tsikari, kaikayi, ƙara yawan ciwo, zafi, da ciwo. Hakanan ana iya samun fitar ruwa daga kan nono. Kimanin rabin matan da aka gano suna da cutar Paget na nono suma suna da kumburi a cikin nono.[22][23]
Sankaran nono mai kumburi ciwo ne da ba kasafai ake samun shi ba (a cikin kasa da kashi 5, cikin 100, na cutar sankarar nono), duk da haka nau'in cutar kansar nono mai tsananin gaske wanda ke kumburi, sauyawa saman nono zuwa ja. Muhimmin sakamakon ciwon daji na nono mai kumburi na faruwa ne sakamakon toshewar tasoshin bututun nono lymph daga kwayoyin cutar kansa. Anfi samun irin wannan nau'in ciwon daji na nono a cikin waɗanda aka gano ta hanyar gwaji ga mata masu ƙananan shekaru, mata masu kiba da kuma matan Amurkawa 'yan asalin Afirka. Kamar yadda ciwon nono mai kumburi ba ya kasancewa da dunƙule wani lokaci ana iya samun jinkiri wajen gano shi.[24]
A lokuta da ba kasafai ba, abin da ya fara bayyana a matsayin fibroadenoma (mai karfi, dunƙule wanda ba-ciwon daji) na iya zama ƙwayar cutar phyllodes. Ciwon phyllodes na wanzuwa ne a cikin stroma (connective tissue) na ƙirjin kuma ya ƙunshi glandular da kuma nama na stromal. Ciwon daji na Phyllodes ba a aiwatar da su a cikin ma'anar da aka saba; An rarraba su bisa ga bayyanarsu a ƙarƙashin na'urar microscope a matsayin benign, borderline ko kuma malignant.[25]
Cutar malignant na iya haifar da ciwace-ciwacen metastatic tumours – secondary tumours (wanda ya samo asali daga primary tumour) wanda ke yaduwa fiye da wurin da ya fara. Alamomin da cutar sankarar nonona metastasis ke haifarwa ya dogara ne akan wurin metastasis yake. Wuraren da ake samun metastasis sun haɗa da kashi, hanta, huhu, da ƙwaƙwalwa. [26] Lokacin da ciwon daji ya kai irin wannan mawuyacib hali, ana kasafta shi a matsayin mataki na 4 na ciwon daji, ciwon daji a wannan mataki sau da yawa yana janyo mutuwa.[27] Alamomi na yau da kullun na ciwon daji na mataki na 4 sun haɗa da asarar nauyi wato kiba dna rashin dalili, ciwon kashi da gabobin jiki, sauyawar launin idanu ko fata da dai sauransu. [28]Ana kiran waɗannan alamomin a matsayin alamomin da basu tabbaa saboda suna iya zama alamu na cututtuka da daban daban.[29] Ciwon daji na nono ba safai yake yaduwa zuwa wuraren da ba a saba gani ba kamar ƙwayoyin lymph nodes waɗanda ke haifar da toshewar biliary wanda ke zama wahala kafin a gano shi.[30]

Yawancin almun ciwon nono, dangane da mafi yawan kullutu, ba sazama ciwon daji na nono. Alal misali, kasa da kashi 20, cikin 100, na kullutu a nono, ke zama ciwon daji na nono, [31] sannan kuma cututtukan nono na benign kamar mastitis da fibroadenoma na nono sune abubuwan da ke haifar da mafi yawancin alamomi na rashin lafiyar nono.[32]
Abubuwan haɗari.
[gyara sashe | gyara masomin]Abubuwan haɗari na iya kasuwa zuwa kashi biyu:
- abubuwan haɗari da za'a iya canzawa (abubuwan da mutane za su iya canza kansu, kamar shan barasa), da
- ƙayyadaddun abubuwan haɗari (abubuwan da ba za a iya canza su ba, kamar shekaru da jinsi).[33]
Muhimman abubuwan da ke haifar da cutar sankarar nono shine kasancewa mace da kuma tsufa.[34] Sauran abubuwan haɗari sun haɗa da kwayoyin halitta na gado, [35] rashin haihuwa ko rashin shayarwa, [36] mafi girman matakan wasu kwayoyin halitta,[37][38]wasu tsarin abinci, da kiba. Wani binciken ya nuna cewa kamuwa da gurɓataccen haske abu ne mai haɗari ga haifuwar ciwon nono.[39]
Idan duka manya (mutane) zasu kiyaye mafi kyawun salon rayuwa, ciki har da rashin shan barasa ba, kiyaye tsarin jiki mai lafiya, rashin shan taba, cin abinci mai kyau, da sauran ayyuka, to kusan kashi ɗaya cikin huɗu na ciwukan dajii na nono a duniya zasu ragu. [40] Ba za a iya hana sauran kashi uku cikin huɗu na cutar kansar nono ta hanyar sauya salon rayuwa ba. [40]
salon rayuwa
[gyara sashe | gyara masomin]
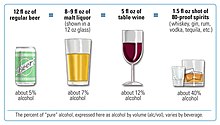
Shan barasa yana ƙara haɗarin cutar kansar nono, har ma da wanda basu sha sosai (mata suna shan ƙasa da rabin kwalban giya a rana). [41]Hadarin yafi yawa a tsakanin masu shan giya sosai. [42] A duniya baki daya, kusan kashi daya cikin 10, na masu fama da cutar kansar nono na faruwa ne sakamakon shan barasa a mata.[42] Shan barasa yana daga cikin abubuwan haɗari na yau da kullun da za a iya canza su.[43]
Akwai alaka sosai a dangantakar da ke tsakanin kiba da sankarar nono. Bincike ya nuna cewa wadanda ke saurin kiba bayan sun girma, suna cikin hatsari fiye da wadanda suke da kiba tun suna yara. [44]Hakazalika, kiba mai yawa a sashin tsakiyar jiki yana yana haifar da hadari mafi girma fiye da kiba sashin kasan jiki.[45] Wannan yana nuna cewa abincin da mutum ke ci yana da mahimmanci fiye da BMI na mutum .[46][47] Abubuwan da za su iya ƙara hadari sun hada da cin abinci mai yawan maiko da matakan cholesterol masu alaƙa da kiba. [48] Yawan cin abinci da ke da karancin iodine na iya taka muhimmin rawa.[49] Shaidar fiber a wajen janyo cutar kansar nono ba shi da tabbas. Wani binciken da aka yi a shekara ta 2015, ya gano cewa binciken da ke ƙoƙarin danganta cin fiber da ciwon nono ya haifar da sakamako daban daban. [50] A cikin shekarar 2016, an gano alaka mara tabbas a tsakanin ƙarancin cin fiber yayin samartaka da ciwon nono.[51]
Shan taba yana kara hadarin kamuwa da cutar kansar nono, tare da yawan adadin da ake sha, da kuma farkon fara shan taba a rayuwa na haifar da hadarin mafi girma.[52] A cikin wadanda ke shan taba na tsawon lokaci, haɗarin na karuwa daga kaso 35% zuwa 50%.[52]
An danganta rashin motsa jiki da kusan kashi 10% na cutar kansar nono.[53] Zama a wuri daya na tsawon lokaci yana da alaka da yawan mace-mace daga ciwon nono. Ba a kawar da hadarin ta hanyar motsa jiki na yau da kullum, ko da yake ana rage shi sosai.[54]
Maganin Hormone don magance menopause shima yana da alaƙa da hadarin cutar kansar nono. [55] Yin amfani da maganin hana haihuwa na hormonal baya haifar da ciwon nono ga yawancin mata;[56] idan yana da tasiri, yana da ƙananan (a kan tsari na 0.01% a kowace shekara-shekara; kwatankwacin adadin mace-macen mata masu juna biyu a Amurka ),[57] na wucin gadi, da raguwa ta masu amfani' sun ragu sosai. hadarin ciwon daji na ovarian da endometrial.[57] Daga cikin wadanda ke da tarihin iyali na ciwon daji na nono, yin amfani da maganin hana haihuwa na zamani ba zai iya yin tasiri ga hadarin ciwon nono ba.[58] Ba shi da tabbas ko maganin hana haihuwa na hormonal zai iya ƙara yawan adadin ciwon nono a cikin mata tare da maye gurbi a cikin kwayoyin cutar ciwon nono[59]
Shayarwa na rage hadarin kamuwa da cutar kansar nono sosai, gami da kansar nono.[60][61][62][63] A cikin 1980s, hasashen zubar da ciki – ciwon nono da aka yi nuni da cewa haifar da zubar da ciki ya kara haɗarin kamuwa da kansar nono.[64] Wannan hasashe ya kasance batun binciken kimiyya mai zurfi, wanda ya kammala da cewa ba zubar da ciki ko zubar da ciki ba yana da alaka da hadarin cutar kansar nono.[65]
Sauran abubuwan hadari sun hada da radiation [66] da rushewar circadian da ke da alaƙa da aikin motsa jiki da cin abinci na yau da kullun.[67] An kuma danganta adadin sinadarai,[68] ciki har da polychlorinated biphenyls, polycyclic aromatic hydrocarbons, da sauran kaushi na halitta Ko da yake radiation daga mammography yana da ƙananan kashi,[69] an kiyasta cewa binciken shekara daga 40, zuwa 80, shekaru zai haifar da kimanin 225, kamuwa da cutar kansar nono ga mata miliyan daya da aka duba.[70]
Kwayoyin haihuwa
[gyara sashe | gyara masomin]An yi imanin cuwa gado na kwayoyin haihuwa ne muhimmin abun da ke janyo ciwon nono a kashi 5–10% na daukakin cutar.[71] Matan da aka gano cutar a jikin mahaifiyarsu bayan shekaru 50, suna da hadarin kamuwa da cutar na 1.7, sannan wadanda aka gano cutan a iyayensu mata kafin shekaru 50, ko bayan sun sami karin hadarin 1.4.[72] A cikin wadanda ba su da sifili, dangi ɗaya ko biyu ya shafa, haɗarin ciwon nono kafin shekaru 80 shine 7.8%, 13.3%, da 21.1% tare da mace-mace mai zuwa daga cutar 2.3%, 4.2%, da 7.6% bi da bi. [73] A cikin wadanda ke da dangi na farko tare da cutar haɗarin kansar nono tsakanin shekaru 40, zuwa 50, ya ninka na yawan jama'a.[74]
A cikin kasa da kashi 5% na lokuta, kwayoyin halitta suna taka muhimmiyar rawa ta haifar da ciwon daji na nono-ovarian na gado . [75] Wannan ya hada da wadanda ke dauke da maye gurbi na BRCA1 da BRCA2 . [75]Wadannan maye gurbi sun kai kashi 90% na jimillar tasirin kwayoyin halitta tare da hadarin kansar nono na 60-80% a cikin wadanda abin ya shafa.[71] Sauran mahimman maye gurbi sun haɗa da p53 ( ciwoyin Li-Fraumeni ), PTEN ( ciwoyin Cowden ), da STK11 ( Peutz-Jeghers ciwo ), CHEK2, ATM, BRIP1, da PALB2 [71]. A shekara ta 2012, masu bincike sun ce akwai nau'ikan ciwon daji na nono guda hudu daban-daban kuma a kowane nau'i, canje-canjen kwayoyin halitta suna haifar da ciwon daji da yawa.[76]
Sauran abubuwan da ke haifar da kwayoyin halitta sun hada da yawan kwayar nono da matakan hormonal. Mata masu yawan nono suna iya kamuwa da ciwace-ciwacen ciwace kuma ba za a iya gano su da cutar kansar nono ba - saboda yawan nama yana sa ciwace-ciwace ba a iya gani a mammograms. Bugu da ƙari kuma, matan da ke da yawan isrogen da matakan progesterone suma suna cikin hadari mafi girma don ci gaban kwayar cuta.[77][78]
Yanayin lafiya
[gyara sashe | gyara masomin]Canje-canjen nono kamar hyperplasia atypical ductal hyperplasia [79] da carcinoma lobular ,[80][81] aka samu a cikin yanayin nono mara kyau kamar canjin nono fibrocystic, suna da alaƙa da haɗarin ciwon nono.
Ciwon sukari mellitus kuma na iya kara hadarin kansar nono.[82] Cututtukan autoimmune irin su lupus erythematosus da alama suna kara hadarin kamuwa da cutar kansar nono.[83]
Babban abubuwan da ke haifar da ciwon nono na lokaci-lokaci suna da alaka da matakan hormone. Ciwon daji na nono yana inganta ta hanyar estrogen. Wannan hormone yana kunna ci gaban nono a duk lokacin balaga, hawan haila da ciki. Rashin daidaituwa tsakanin estrogen da progesterone a lokacin haila yana haifar da yaduwar kwayar halitta. Haka kuma, oxidative metabolites na estrogen na iya kara lalacewar DNA da maye gurbi. Maimaita hawan keke da nakasa tsarin gyara na iya canza tantanin halitta ta al'ada zuwa pre-malignant kuma daga karshe m tantanin halitta ta maye gurbi. A lokacin mataki na gaba, za a iya kunna haɓakar kwayoyin stromal ta hanyar estrogen don tallafawa ci gaban ciwon nono. A lokacin kunnawa mai daure ligand, ER na iya daidaita maganganun kwayoyin halitta ta hanyar yin hulɗa tare da abubuwan amsawar isrogen a cikin masu habaka takamaiman kwayoyin halitta. Magana da kunnawa na ER saboda rashin isrogen za a iya motsa shi ta hanyar siginar salula. [84] Abin sha'awa, ER yana daure kai tsaye tare da sunadaran sunadaran, gami da masu karbar abubuwan haɓaka, na iya haɓaka maganganun kwayoyin halittar da ke da alaka da habakar tantanin halitta da rayuwa.[85]
Habaka matakan prolactin a cikin jini yana da alaka da hadarin cutar kansar nono.[86]
Pathophysiology
[gyara sashe | gyara masomin]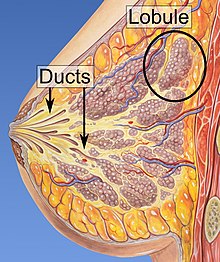
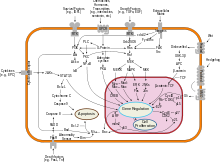
Ciwon daji na nono, kamar sauran cututtuka, yana faruwa ne saboda hulɗar da ke tsakanin yanayin muhalli (na waje) da kuma mai saurin kamuwa da kwayoyin halitta. Kwayoyin al'ada suna rarraba sau da yawa gwargwadon buƙata kuma suna tsayawa. Suna haɗawa da wasu sel kuma suna zama a cikin kyallen takarda. Kwayoyin suna zama masu cutar kansa lokacin da suka rasa ikon daina rarrabawa, mannewa ga wasu kwayoyin halitta, su zauna a inda suke, kuma su mutu a lokacin da ya dace.
Kwayoyin al'ada za su lalace da kansu ( shirin mutuwa cell ) lokacin da ba a buƙatar su. Har sai lokacin, sel suna samun kariya daga shirin mutuwa ta gungu na furotin da hanyoyi da yawa. Ɗaya daga cikin hanyoyin kariya shine hanyar PI3K / AKT ; wata ita ce hanyar RAS / MEK / ERK . Wani lokaci kwayoyin halittar da ke kan wadannan hanyoyin kariya suna canzawa ta hanyar da za su juya su har abada "a kunne", yana mai da tantanin halitta ba zai iya lalata kansa ba lokacin da ba a buƙata. Wannan yana daya daga cikin matakan da ke haifar da ciwon daji a hade tare da sauran maye gurbi. A al'ada, furotin PTEN yana kashe hanyar PI3K/AKT lokacin da tantanin halitta ya shirya don shirin mutuwar tantanin halitta. A wasu cututtukan nono, kwayar halittar furotin na PTEN ta canza, don haka hanyar PI3K/AKT ta makale a matsayin "kan", kuma kwayar cutar kansa ba ta lalata kanta.[87]
Maye gurbi da zai iya haifar da ciwon nono an gwada gwadawa da bayyanar isrogen.[88] Bugu da ƙari, G-protein haɗe-haɗe da masu karɓar isrogen an haɗa su da cututtuka daban-daban na tsarin haihuwa na mata ciki har da ciwon nono.[89]
Alamar haɓakar haɓaka mara kyau a cikin hulɗar tsakanin ƙwayoyin stromal da ƙwayoyin epithelial na iya sauƙaƙe haɓakar ƙwayar ƙwayar cuta. [90][91] A cikin ƙwayar adipose na nono, yawan wuce gona da iri na leptin yana haifar da haɓakar ƙwayoyin cuta da ciwon daji.[92]
A cikin Amurka, kashi 10, zuwa 20, na matan da ke fama da ciwon nono ko ciwon daji na ovarian suna da dangi na farko ko na biyu tare da ɗayan waɗannan cututtuka. Maza masu ciwon nono suna da yuwuwar hakan. Halin iyali na haɓaka waɗannan ciwon daji ana kiransa ciwon nono-ovarian cancer syndrome . Mafi sanannun waɗannan, maye gurbi na <i id="mwAdQ">BRCA</i>, suna ba da haɗarin rayuwa na ciwon nono tsakanin 60, da 85, bisa dari da kuma haɗarin ciwon daji na ovarian tsakanin 10, da 40, bisa dari. Wasu maye gurbi da ke da alaƙa da ciwon daji, kamar p53, BRCA1 da BRCA2, suna faruwa a cikin hanyoyin gyara kurakurai a cikin DNA . Wadannan maye gurbi ana gadonsu ko kuma ana samun su bayan haihuwa. Mai yiwuwa, suna ƙyale ƙarin maye gurbi, wanda ke ba da damar rarrabuwar kawuna, rashin haɗin kai, da metastasis ga gabobin nesa. Koyaya, akwai ƙaƙƙarfan shaida na saura haɗarin haɗarin da ke wuce gona da iri na BRCA na gado tsakanin iyalai masu ɗaukar kaya. Wannan yana faruwa ne ta hanyar abubuwan haɗari da ba a lura da su ba. Wannan yana haifar da muhalli da sauran dalilai a matsayin abubuwan da ke haifar da cutar kansar nono. Maye gurbin da aka gada a cikin BRCA1 ko BRCA2 na iya tsoma baki tare da gyara hanyoyin haɗin giciye na DNA da raguwar igiyoyi biyu na DNA (sananan ayyukan furotin da aka ɓoye). Wadannan carcinogens suna haifar da lalacewar DNA kamar mahaɗan giciye na DNA da kuma raguwar igiyoyi biyu waɗanda galibi suna buƙatar gyara ta hanyoyi masu ɗauke da BRCA1 da BRCA2. Duk da haka, maye gurbi a cikin kwayoyin halittar BRCA yana lissafin kashi 2, zuwa 3, ne kawai na duk cutar kansar nono. Levin et al. ka ce ciwon daji na iya zama ba makawa ga duk masu ɗauke da maye gurbi na BRCA1 da BRCA2. Kimanin rabin cututtukan daji na nono-ovarian na gado sun ƙunshi kwayoyin halittar da ba a san su ba. Bugu da ƙari kuma, wasu ƙwayoyin cuta masu ɓoye, na iya rage bayyanar kwayar cutar ta BRCA1 kuma suna ƙara haɗarin ciwace-ciwacen nono.
GATA-3 kai tsaye yana sarrafa maganganun mai karɓar isrogen (ER) da sauran kwayoyin halitta da ke da alaƙa da bambancin epithelial, kuma asarar GATA-3 yana haifar da asarar bambance-bambance da rashin hasashe mara kyau saboda cutar ciwon daji da kuma metastasis.
Bincike.
[gyara sashe | gyara masomin]Yawancin nau'in ciwon daji na nono suna da sauƙin ganewa ta hanyar nazarin microscopic na samfurin - ko biopsy - na yankin da abin ya shafa na nono. Hakanan, akwai nau'ikan cutar kansar nono waɗanda ke buƙatar gwajin gwaji na musamman.
Hanyoyi guda biyu da aka fi amfani da su na nunawa, gwajin jiki na ƙirjin da ma'aikacin kiwon lafiya da mammography, na iya ba da kusan yiwuwar cewa kullu ya zama ciwon daji, kuma yana iya gano wasu raunuka, irin su cysts mai sauƙi. Lokacin da waɗannan gwaje-gwajen ba su da ma'ana, ma'aikacin kiwon lafiya zai iya cire samfurin ruwan da ke cikin dunƙule don nazarin microscopic (wani hanya da aka sani da kyakkyawan buri, ko kyakkyawan buri da cytology, FNAC) don taimakawa wajen tabbatar da ganewar asali. Ana iya yin buri na allura a ofishin ma'aikatan kiwon lafiya ko asibitin. Ana iya amfani da maganin sa barci na gida don murƙushe ƙwayar nono don hana zafi yayin aikin, amma maiyuwa bazai zama dole ba idan kullin baya ƙarƙashin fata. Gano ruwa mai tsafta yana sa kullun ba zai zama mai cutar kansa ba, amma ana iya aika ruwan jini don dubawa a karkashin na'urar hangen nesa don sel masu ciwon daji. Tare, ana iya amfani da gwajin jiki na ƙirjin, mammography, da FNAC don tantance cutar kansar nono tare da ingantaccen matakin daidaito.
Sauran zaɓuɓɓukan don biopsy sun haɗa da core biopsy ko vacuum-assisted nono biopsy, waxannan hanyoyin da ake cire wani sashe na kutun nono; ko biopsy excisional, wanda a cikinsa aka cire gaba ɗaya dunƙule. Sau da yawa sakamakon gwajin jiki ta ma'aikacin kiwon lafiya, mammography, da ƙarin gwaje-gwajen da za'a iya yi a cikin yanayi na musamman (kamar hoto ta duban dan tayi ko MRI ) sun isa don ba da garantin biopsy na cirewa azaman madaidaicin ganewar asali da hanyar magani na farko. [ Babu tushen tushen da ake buƙata ]
-
MRI yana nuna kansar nono
-
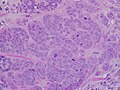
Carcinoma mai ɗorewa mai girma, tare da ƙananan ƙwayar tubule, alamar pleomorphism, da fitattun mitoses, filin 40x
-
Micrograph yana nuna kumburin lymph wanda ductal nono carcinoma ya mamaye, tare da tsawo na ƙari fiye da kumburin lymph.
-
Maganar Neuropilin-2 a cikin nono na al'ada da ƙwayar nono
-
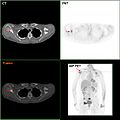
F-18 FDG PET/CT: Ciwon daji na nono metastasis zuwa scapula na dama
-
Allura biopsy na nono
-
Eastography yana nuna taurin ƙwayar cutar kansa akan hoton duban dan tayi.
-
Hoton duban dan tayi yana nuna yawan cutar kansar nono mara tsari.
-
Ciwon daji na nono (mai zazzagewa).
-
Mammograms yana nuna nono na yau da kullun (hagu) da nono mai ciwon daji (dama)
Rabewa
[gyara sashe | gyara masomin]An rarraba kansar nono ta tsarin ƙima da yawa. Kowane ɗayan waɗannan yana rinjayar hasashen kuma zai iya rinjayar amsawar jiyya. Bayanin ciwon nono yana da kyau ya haɗa da waɗannan abubuwan.
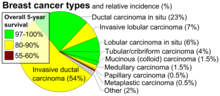
- Histopathology to . Nono ne yawanci classified farko da ta histological bayyanar. Yawancin ciwon daji na nono an samo su ne daga epithelium wanda ke rufe ducts ko lobules, kuma waɗannan ciwon daji an rarraba su azaman carcinoma ductal ko lobular. Carcinoma a wurin shine haɓakar ƙananan ƙwayoyin cuta masu ciwon daji ko ƙwayoyin cuta a cikin wani yanki na musamman kamar tashar mammary ba tare da mamaye nama da ke kewaye ba. Sabanin haka, carcinoma mai ɓarna ba ya keɓe kansa zuwa sashin nama na farko.
- Daraja . Ƙididdigar ƙididdiga tana kwatanta bayyanar ƙwayoyin kansar nono da bayyanar nama na nono na yau da kullun. Kwayoyin al'ada a cikin gaba kamar nono suna bambanta, ma'ana suna ɗaukar takamaiman siffofi da siffofi waɗanda ke nuna aikinsu a matsayin ɓangaren wannan sashin. Kwayoyin ciwon daji sun rasa wannan bambancin. A cikin ciwon daji, ƙwayoyin da za su yi layi a cikin tsari don samar da hanyoyin madara sun zama marasa tsari. Rarrabuwar salula ya zama mara sarrafawa. Kwayoyin tsakiya sun zama ƙasa da uniform. Masana ilimin cututtuka sun bayyana sel suma sun bambanta (ƙananan daraja), matsakaicin bambance-bambance (matsakaici), da rashin bambance-bambance (matsayi mai girma) yayin da ƙwayoyin ke ci gaba da rasa sifofin da ake gani a cikin ƙwayoyin nono na yau da kullun. Rashin bambance-bambancen daji mara kyau (waɗanda naman jikinsu ya fi ƙanƙanta kamar naman nono na yau da kullun) suna da mummunan hasashen.
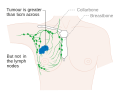
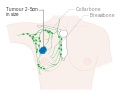
- Mataki . Ciwon daji na nono ta amfani da tsarin TNM yana dogara ne akan girman t umor ( T ), ko ciwon daji ya yadu zuwa lymph n odes ( N ) a cikin ƙwanƙwasa, da kuma ko ciwon daji yana da m etastasized ( M ) ( watau yaduwa zuwa wani yanki mai nisa na jiki). Girman girma, yaduwar nodal, da metastasis suna da lambar mataki mafi girma da mafi muni.
Manyan matakai sune:- Mataki na 0 shine pre-cancer ko alama yanayin, ko dai ductal carcinoma in situ (DCIS) ko lobular carcinoma in situ (LCIS).
- Matakai na 1-3, suna cikin nono ko yanki na lymph nodes.
- Mataki na 4, shine ciwon daji na 'metastatic' wanda ke da ƙarancin tsinkaya tun lokacin da ya yadu fiye da nono da ƙwayoyin lymph na yanki.
-
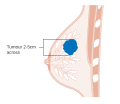
Stage T1 ciwon nono
-
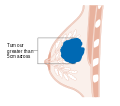
Stage T2 ciwon nono
-
Stage T3 ciwon nono
-
Metastatic ko mataki na 4 kansar nono
- Inda akwai, ana iya amfani da nazarin hoto azaman ɓangare na tsarin tsarawa a cikin zaɓin lokuta don neman alamun ciwon daji na ƙazanta. Duk da haka, a cikin lokuta na ciwon nono tare da ƙananan haɗari don metastasis, haɗarin da ke hade da PET scans, CT scans, ko duban kashi fiye da amfanin da za a iya samu, kamar yadda waɗannan hanyoyin suna fallasa mutum zuwa adadi mai mahimmanci na radiation ionizing mai haɗari.
- Matsayin mai karɓa . Kwayoyin cutar kansar nono suna da masu karɓa a saman su kuma a cikin cytoplasm da tsakiya . Manzannin sinadarai irin su hormones suna ɗaure ga masu karɓa, kuma wannan yana haifar da canje-canje a cikin tantanin halitta. Kwayoyin ciwon nono na iya ko ba su da masu karɓa guda uku masu mahimmanci: estrogen receptor (ER), progesterone receptor (PR), da HER2 .
Kwayoyin ciwon daji na ER+ (wato, ƙwayoyin ciwon daji waɗanda ke da masu karɓar isrogen) suna dogara ne akan estrogen don girma, don haka za'a iya magance su da kwayoyi don toshe tasirin estrogen (misali tamoxifen ), kuma gabaɗaya suna da kyakkyawan hangen nesa. Ba a yi magani ba, HER2+ ciwon nono gabaɗaya sun fi HER2- ciwon nono, amma HER2+ ƙwayoyin kansa suna amsa magunguna irin su monoclonal antibody trastuzumab (a hade tare da chemotherapy na al'ada), kuma wannan ya inganta hasashen sosai. Kwayoyin da ba su da kowane ɗayan waɗannan nau'ikan masu karɓa guda uku (masu karɓar isrogen, masu karɓar progesterone, ko HER2) ana kiran su sau uku-negative, ko da yake suna yawan bayyana masu karɓa ga sauran kwayoyin halitta, irin su mai karɓar androgen da prolactin receptor . - Binciken DNA . Gwajin DNA na nau'ikan nau'ikan daban-daban ciki har da microarrays na DNA sun kwatanta sel na yau da kullun zuwa ƙwayoyin kansar nono. Za a iya amfani da takamaiman canje-canje a cikin wani ciwon daji na nono don rarraba kansa ta hanyoyi da yawa, kuma yana iya taimakawa wajen zaɓar magani mafi inganci don irin wannan nau'in DNA.
-
Mataki na 1A ciwon nono
-
Mataki na 1B ciwon nono
-
Mataki na 2A ciwon nono
-
Mataki na 2A ciwon nono
-
Mataki na 2B ciwon nono
-
Mataki na 2B ciwon nono
-
Mataki na 2B ciwon nono
-
Mataki na 3A ciwon nono
-
Mataki na 3A ciwon nono
-
Mataki na 3A ciwon nono
-
Mataki na 3B ciwon nono
-
Mataki na 3B ciwon nono
-
Mataki na 4 ciwon nono
Gwaji.
[gyara sashe | gyara masomin]
Yin gwajin cutar kansar nono yana nufin gwada wasu mata masu lafiya game da cutar kansar nono a yunƙurin cimma wani bincike da aka yi a baya a ƙarƙashin zaton cewa ganowa da wuri zai inganta sakamako. An yi amfani da gwaje-gwajen gwaje-gwaje da yawa waɗanda suka haɗa da na asibiti da gwajin nono, mammography, gwajin ƙwayoyin cuta, duban dan tayi, da hoton maganadisu.
Gwajin nono na asibiti ko na kai ya ƙunshi jin ƙirjin don kulluwa ko wasu rashin daidaituwa. Ma’aikatan lafiya ne ke yin gwajin nono na asibiti, yayin da mutum da kansa ke yin gwajin nono. Shaidu ba su goyi bayan ingancin kowane nau'in jarrabawar nono ba, domin a lokacin da kullu ya yi girma da za a iya gano shi yana iya yin girma shekaru da yawa don haka nan da nan ya isa a same shi ba tare da jarrabawa ba. Binciken mammography don ciwon nono yana amfani da hasken X-ray don bincika nono ga kowane taro ko kullun da bai dace ba. Yayin nunawa, ƙirjin yana matsawa kuma mai fasaha yana ɗaukar hotuna daga kusurwoyi da yawa. Mammogram na gaba ɗaya yana ɗaukar hotuna na gabaɗayan nono, yayin da mammogram na bincike ya mai da hankali kan takamaiman dunƙule ko yanki na damuwa.
Yawancin ƙungiyoyin ƙasa sun ba da shawarar auna cutar kansar nono. Ga talakawan mace, da Amurka M Services Task Force da American College of Physicians bada shawarar mammography kowace shekara biyu a mata dake da shekaru 50,da 74, da majalisar Turai ya bada shawarar mammography tsakanin 50, da 69 tare da mafi shirye-shirye ta amfani da mitar shekaru 2, yayin da Hukumar Turai ta ba da shawarar mammography daga 45, zuwa 75, kowane 2, zuwa 3 shekaru, kuma a Kanada ana ba da shawarar yin gwajin tsakanin shekarun 50, da 74, a mitar 2, zuwa 3 shekaru. . Waɗannan rahotannin runduna sun yi nuni da cewa baya ga tiyatar da ba dole ba da damuwa, haɗarin da ke tattare da mammogram akai-akai sun haɗa da ƙaramin ƙanƙara amma ƙaƙƙarfan haɓakar kansar nono da radiation ta haifar.
Haɗin gwiwar Cochrane (2013),ya bayyana cewa mafi kyawun shaida mai inganci baya nuna raguwar takamaiman cutar kansa, ko raguwa a cikin duk abubuwan da ke haifar da mace-mace daga gwajin mammography. Lokacin da aka ƙara ƙananan gwaji a cikin bincike ana samun raguwar mace-mace saboda ciwon nono na 0.05% (raguwar 1 a cikin 2000, mutuwar daga ciwon nono sama da shekaru 10, ko kuma raguwar dangi na 15% daga ciwon nono). [93] Nunawa sama da shekaru 10, yana haifar da haɓakar 30% a cikin ƙimar fiye da kima da yawan jiyya (3 zuwa 14, a cikin 1000) kuma fiye da rabin za su sami aƙalla gwajin inganci na ƙarya. [93] Wannan ya haifar da ra'ayin cewa ba a bayyana ko duban mammography ya fi kyau ko cutarwa ba. [93] Cochrane ya bayyana cewa, saboda sauye-sauye na baya-bayan nan game da maganin cutar kansar nono, da kuma kasadar abubuwan da ke tattare da karya daga binciken cutar kansar nono da ke haifar da jiyya maras amfani, "don haka ba ya da amfani a halarci gwajin cutar kansar nono" a kowane zamani. Ko MRI a matsayin hanyar nunawa yana da lahani mafi girma ko amfani idan aka kwatanta da daidaitattun mammography ba a sani ba. duk abunda and cikr lailai kareria nada matuqar mahimmanci saboda tearing lafia da Maria dangane da Priyasamundomin samun lfy nada matuqar mahimmanci saboda tafiya da Kuma babu watadama face a bude him rigakafi abun godia saboda tsarin lafia da Kuma samun sauqi wajen Nemo dalilin yin rigakafi da Kuma Neman maganin ciwon nonan kansan mata.
Rigakafi.
[gyara sashe | gyara masomin]Salon Rayuwa
[gyara sashe | gyara masomin]Mata za su iya rage haɗarin kamuwa da cutar kansar nono ta hanyar kiyaye nauyi mai kyau, rage shan barasa, ƙara motsa jiki, da shayarwa. Wadannan gyare-gyaren na iya hana kashi 38% na cutar kansar nono a Amurka, 42% a Burtaniya, 28% a Brazil, da 20% a China. Ana ganin fa'idodin tare da matsakaicin motsa jiki kamar tafiya mai gaugawa a kowane rukunin shekaru ciki har da matan da suka shude. Yawan aikin motsa jiki yana rage haɗarin cutar kansar nono da kusan kashi 14%. Dabarun da ke ƙarfafa motsa jiki na yau da kullun da rage kiba kuma na iya samun wasu fa'idodi, kamar rage haɗarin cututtukan zuciya da ciwon sukari.
Al'ummar cutar kanzzon kai na Amurka da kuma al'ummar {asirci na Amurka da aka shawarci kasar a shekarar 2016, da ya kamata mutane su ci abinci a cikin kayan lambu, 'ya'yan itãcen marmari, hatsi guda, da kuma kafafun kafirai. Yawan cin 'ya'yan itacen citrus yana da alaƙa da raguwa 10% cikin haɗarin cutar kansar nono. Marine omega-3 polyunsaturated fatty acid ya bayyana yana rage haɗarin. Yawan cin abinci na tushen soya na iya rage haɗari.
Tiyatar Riga-kafi
[gyara sashe | gyara masomin]Cire ƙirjin biyu kafin a gano ciwon daji ko duk wani kullutu mai zato ko wani rauni ya bayyana (wani hanya da aka sani da "mastectomy prophylactic bilateral mastectomy" ko "haɗarin rage mastectomy") ana iya la'akari da mata masu BRCA1 da BRCA2 maye gurbi, waɗanda ke da alaƙa. tare da babban haɗari don gano cutar kansar nono. Shaida ba ta da ƙarfi don tallafawa wannan hanya a cikin kowa sai mata a cikin haɗari mafi girma. Ana ba da shawarar gwajin BRCA a cikin waɗanda ke da babban haɗarin iyali bayan shawarwarin kwayoyin halitta. Ba a ba da shawarar akai-akai ba. Wannan saboda akwai nau'ikan canje-canje da yawa a cikin kwayoyin halittar BRCA, kama daga nau'ikan polymorphisms marasa lahani zuwa ga maye gurbi mai haɗari. Tasirin yawancin sauye-sauyen da ake iya ganewa a cikin kwayoyin halitta ba shi da tabbas. Gwaji a cikin matsakaita mai haɗari yana da yuwuwar dawo da ɗayan waɗannan sakamako marasa fa'ida, marasa amfani. Cire nono na biyu a cikin mutumin da ke da ciwon nono (wanda ke rage haɗarin mastectomy ko CRRM) na iya rage haɗarin ciwon daji a cikin nono na biyu, duk da haka, ba a sani ba idan cire nono na biyu a cikin waɗanda ke da ciwon nono yana inganta rayuwa.
Magunguna
[gyara sashe | gyara masomin]Zaɓuɓɓukan masu karɓar mai karɓar isrogen suna rage haɗarin ciwon nono amma suna ƙara haɗarin thromboembolism da ciwon daji na endometrial. Babu wani sauyi gaba ɗaya a cikin haɗarin mutuwa. Don haka ba a ba da shawarar su don rigakafin cutar kansar nono a cikin mata a matsakaicin haɗari amma ana ba da shawarar a ba da su ga waɗanda ke cikin haɗarin haɗari kuma sama da shekaru 35. Amfanin rage ciwon nono yana ci gaba da aƙalla shekaru biyar bayan dakatar da wani. hanyar jiyya tare da waɗannan magunguna. Masu hana Aromatase (irin su exemestane da anasatrozole) na iya zama mafi tasiri fiye da masu amfani da masu karɓar isrogen receptor (irin su tamoxifen) don rage haɗarin ciwon nono kuma ba su da alaƙa da haɗarin ciwon daji na endometrial da thromboembolism.
Gudanarwa.
[gyara sashe | gyara masomin]Gudanar da ciwon nono ya dogara da abubuwa daban-daban, ciki har da matakin ciwon daji da kuma shekarun mutum. Jiyya sun fi zafi lokacin da ciwon daji ya fi girma ko kuma akwai haɗarin sake dawowa daga ciwon daji bayan magani.
Yawanci ana yin maganin kansar nono da tiyata, wanda ƙila a biyo shi ta hanyar chemotherapy ko radiation far, ko duka biyun. Hanyar da'a iri-iri ya fi dacewa. Hormone receptor-positive cancers yawanci ana bi da su tare da maganin toshewar hormone a cikin darussan shekaru da yawa. Monoclonal antibodies, ko wasu jiyya-modulating rigakafi, za a iya gudanar a wasu lokuta na metastatic da sauran ci gaban matakai na ciwon nono. Ko da yake ana ci gaba da nazarin wannan nau'in magani.

Tiyata
[gyara sashe | gyara masomin]Tiyata ta ƙunshi cire ƙwayar ƙwayar cuta ta jiki, yawanci tare da wasu nama da ke kewaye. Za a iya cire nodes ɗaya ko fiye da ƙwayoyin lymph yayin aikin tiyata; Ana ƙara yin samfurin ƙwayar lymph ta hanyar biopsy na node na lymph.
Daidaitaccen aikin tiyata ya haɗa da:
- Mastectomy: Cire dukkan nono.
- Quadrantectomy: Cire kashi ɗaya cikin huɗu na ƙirjin.
- Lumpectomy: Cire wani karamin sashi na nono.
Da zarar an cire ƙwayar cutar, idan mutum yana so, ana iya yin tiyatar gyaran nono, nau'in tiyata na filastik, don inganta kyawun wurin da aka yi masa magani. A madadin, mata suna amfani da kayan aikin nono don kwaikwayi nono a ƙarƙashin tufafi, ko zabar ƙirji mai lebur. Ana iya amfani da prosthesis na nono a kowane lokaci bayan mastectomy.
Magani
[gyara sashe | gyara masomin]Magungunan da aka yi amfani da su bayan da ban da tiyata ana kiran su maganin motsa jiki. Chemotherapy ko wasu nau'ikan jiyya kafin a yi tiyata ana kiran su neoadjuvant therapy. Aspirin na iya rage mace-mace daga kansar nono lokacin amfani da wasu jiyya.
A halin yanzu akwai manyan ƙungiyoyin magunguna guda uku da ake amfani da su don maganin ciwon nono na adjuvant: masu hana hormone, chemotherapy, da ƙwayoyin rigakafi na monoclonal.
Hormonal therapy
[gyara sashe | gyara masomin]Wasu ciwon daji na nono suna buƙatar estrogen don ci gaba da girma. Ana iya gano su ta hanyar kasancewar masu karɓar isrogen (ER +) da masu karɓa na progesterone (PR +) a saman su (wani lokaci ana kiran su tare a matsayin masu karɓa na hormone). Ana iya magance waɗannan cututtukan daji na ER+ da magunguna waɗanda ko dai suna toshe masu karɓa, misali. tamoxifen, ko kuma a madadin toshe samar da estrogen tare da mai hana aromatase, misali. Anastrozole ko letrozole. Ana bada shawarar yin amfani da tamoxifen na tsawon shekaru 10. Tamoxifen yana ƙara haɗarin zubar jini na postmenopausal, polyps na endometrial, hyperplasia, da ciwon daji na endometrial; Yin amfani da tamoxifen tare da Tsarin IntraUterine wanda ke sakin levonorgestrel na iya ƙara zubar jini a cikin farji bayan shekaru 1, zuwa 2, amma yana rage ɗan ƙaramin polyps na endometrial da hyperplasia, amma ba dole ba ne ciwon daji na endometrial. Letrozole yana bada shawarar tsawon shekaru biyar.
Masu hana Aromatase sun dace da mata kawai bayan menopause; duk da haka, a cikin wannan rukuni, sun fi kyau fiye da tamoxifen. Wannan shi ne saboda aromatase mai aiki a cikin matan da suka shude ya bambanta da nau'i mai yawa a cikin mata masu tasowa, sabili da haka waɗannan wakilai ba su da tasiri wajen hana babban aromatase na mata masu tasowa. Kada a ba masu hanawar Aromatase ga matan da suka riga sun haihu tare da ingantaccen aikin ovarian (sai dai idan suna kan magani don dakatar da ovaries daga aiki). Ana iya amfani da masu hana CDK a hade tare da endocrin ko maganin aromatase.
Chemotherapy
[gyara sashe | gyara masomin]Chemotherapy ana amfani dashi galibi don lokuta na ciwon nono a matakai na 2-4, kuma yana da fa'ida musamman a cikin cutar mai karɓar isrogen-negative (ER-). Ana gudanar da magungunan chemotherapy a cikin haɗuwa, yawanci na tsawon watanni 3-6. Ɗaya daga cikin tsarin da aka fi sani da "AC", ya haɗa cyclophosphamide tare da doxorubicin. Wani lokaci ana ƙara magungunan haraji, irin su docetaxel, kuma ana kiran tsarin mulkin da "CAT". Wani magani na yau da kullun shine cyclophosphamide, methotrexate, da fluorouracil (ko "CMF"). Yawancin magungunan chemotherapy suna aiki ta hanyar lalata ƙwayoyin cutar daji masu saurin girma da/ko masu saurin kwafi, ko dai ta haifar da lalacewar DNA akan kwafi ko ta wasu hanyoyin. Koyaya, magungunan kuma suna lalata ƙwayoyin al'ada masu girma cikin sauri, wanda zai iya haifar da mummunan sakamako. Lalacewa ga tsokar zuciya shine mafi hatsarin rikitarwa na doxorubicin, alal misali.[Ana bukatan hujja]
Monoclonal antibodies
[gyara sashe | gyara masomin]Trastuzumab, maganin rigakafi na monoclonal zuwa HER2, ya inganta rayuwar shekaru biyar marasa lafiya na mataki na 1-3 HER2 mai cutar kansa zuwa kusan 87% (ci gaba da rayuwa 95%). Tsakanin kashi 25 zuwa kashi 30 cikin 100 na cutar kansar nono suna wuce gona da iri kan HER2 gene ko furotin da ake samarwa, da kuma wuce gona da iri na HER2 a cikin ciwon nono yana da alaƙa da sake dawowar cututtuka da kuma mafi muni. Trastuzumab, duk da haka, yana da tsada sosai, kuma amfani da shi na iya haifar da munanan illolin (kimanin 2% na mutanen da suka karɓa suna haifar da mummunar lalacewar zuciya). Wani antibody pertuzumab yana hana HER2 dimerization kuma ana bada shawarar tare da trastuzumab da chemotherapy a cikin cututtuka mai tsanani.
Radiation
[gyara sashe | gyara masomin]
Ana ba da maganin rediyo bayan tiyata zuwa yankin gadon ciwon daji da kuma nodes na lymph nodes, don lalata ƙwayoyin tumor ƙananan ƙwayoyin cuta waɗanda wataƙila sun tsere daga tiyata. Lokacin da aka ba da shi ta hanyar tiyata kamar yadda aka yi niyya na intraoperative radiotherapy, yana iya yin tasiri mai fa'ida akan microenvironment na ƙari. Za'a iya isar da maganin radiation azaman maganin rediyo na katako na waje ko azaman brachytherapy (radiation na ciki). Ana ba da magungunan rediyo na al'ada bayan tiyata don ciwon nono. Hakanan za'a iya ba da radiation a lokacin aiki akan kansar nono. Radiation na iya rage haɗarin sake dawowa da kashi 50-66% (1/2 - 2/3 raguwa na haɗari) lokacin da aka kawo shi a cikin daidaitaccen kashi kuma ana la'akari da mahimmanci lokacin da ciwon nono ya yi amfani da shi ta hanyar cire kawai dunƙule (Lumpectomy ko Wide local excision). ). A farkon cutar sankarar nono, wani ɓangare na iska mai iska ba ya ba da ikon sarrafa kansa iri ɗaya a cikin nono kamar yadda ake kula da nono gabaɗaya kuma yana iya haifar da mummunan sakamako.
Kulawa mai biyo baya
[gyara sashe | gyara masomin]Kulawa bayan jiyya na ciwon nono na farko, in ba haka ba ana kiransa 'kula da bin diddigi', na iya zama mai ƙarfi wanda ya haɗa da gwaje-gwajen dakin gwaje-gwaje na yau da kullun a cikin mutanen da ba su da asymptomatic don ƙoƙarin cimma farkon gano yiwuwar metastases. Wani bita ya gano cewa shirye-shiryen biyo baya da suka haɗa da gwaje-gwaje na jiki na yau da kullun da mammography na shekara kawai suna da tasiri kamar ƙarin shirye-shirye masu ƙarfi da suka ƙunshi gwaje-gwajen dakin gwaje-gwaje dangane da gano sake dawowa da wuri, rayuwa gabaɗaya da ingancin rayuwa.[94]
Shirye-shiryen gyaran gyare-gyare na multidisciplinary, sau da yawa ciki har da motsa jiki, ilimi da taimako na tunani, na iya samar da gyare-gyare na gajeren lokaci a cikin ikon aiki, daidaitawar zamantakewa da zamantakewar zamantakewa a cikin mutane masu ciwon nono.[95]
Hasashen
[gyara sashe | gyara masomin]Abubuwan haɓakawa
[gyara sashe | gyara masomin]
Matsayin ciwon nono shine mafi mahimmancin bangaren hanyoyin rarrabuwa na al'ada na ciwon nono, saboda yana da tasiri mai yawa akan tsinkaye fiye da sauran la'akari. Tsari yana la'akari da girman, sa hannun gida, matsayin kumburin lymph da ko cutar metastatic tana nan. Mafi girma mataki a ganewar asali, mafi talauci da tsinkaya. Matakin yana tasowa ta hanyar cin zarafi na cututtuka zuwa ƙwayoyin lymph, bangon kirji, fata ko bayan, da kuma tashin hankali na kwayoyin cutar kansa. An saukar da matakin ta kasancewar yankunan da ba su da ciwon daji da kuma dabi'ar tantanin halitta na yau da kullun (masu daraja). Girman ba abu bane a cikin tsari sai dai idan ciwon daji ya mamaye. Misali, Ductal Carcinoma in Situ (DCIS) wanda ya shafi nono gabaɗaya zai kasance matakin sifili kuma saboda haka kyakkyawan tsinkaye tare da rayuwa mara lafiya na shekaru 10, kusan 98%.
- Stage 1 cancers (da DCIS, LCIS) suna da kyakkyawar ganewa kuma ana bi da su tare da lumpectomy da wani lokacin radiation.
- Sashe na 2, da 3, masu ciwon daji tare da ci gaba da rashin talauci da kuma haɗarin sake dawowa gabaɗaya ana bi da su tare da tiyata (lumpectomy ko mastectomy tare da ko ba tare da cire kumburin lymph ba), chemotherapy (da trastuzumab don ciwon daji na HER2+) da kuma wani lokacin radiation (musamman bin manyan cututtuka, da yawa). tabbatacce nodes ko lumpectomy). [akan buƙatun likita]
- Mataki na 4, ciwon daji na metastatic, (watau yaduwa zuwa wurare masu nisa) yana da mummunan hangen nesa kuma ana sarrafa shi ta hanyoyi daban-daban na duk jiyya daga tiyata, radiation, chemotherapy da hanyoyin kwantar da hankali. Yawan tsira na shekaru goma shine 5% ba tare da magani ba kuma 10% tare da ingantaccen magani.
Ana tantance darajar ciwon nono ta hanyar kwatanta ƙwayoyin kansar nono zuwa ƙwayoyin nono na yau da kullun. Mafi kusa da al'ada kwayoyin cutar kansa, da sannu a hankali girma da kuma mafi kyawun tsinkaya. Idan sel ba su bambanta da kyau ba, za su bayyana ba su da girma, za su rarraba cikin sauri, kuma za su yi yaduwa. Wanda aka bambanta da kyau ana ba da maki na 1, matsakaici shine aji 2, yayin da matalauta ko marasa bambanci ana ba su mafi girma na 3 ko 4 (ya danganta da sikelin da aka yi amfani da su). Mafi yawan tsarin ƙima da ake amfani da shi shine tsarin Nottingham.
Matan da ba su wuce shekaru 40, ba ko kuma matan da suka haura shekaru 80, suna fuskantar rashin fahimta fiye da matan da suka biyo bayan menopausal saboda dalilai da yawa. Nononsu na iya canzawa da al'adarsu, suna shayar da jarirai, kuma ba za su san canje-canje a nononsu ba. Don haka, ƙananan mata yawanci suna kan matakin ci gaba idan an gano cutar. Hakanan ana iya samun abubuwan ilimin halitta waɗanda ke haifar da babban haɗarin sake bullar cuta ga ƙananan mata masu ciwon nono.
Abubuwan da suka shafi tunanin mutum
[gyara sashe | gyara masomin]Ba duk mutanen da ke fama da cutar kansar nono ke fuskantar cutarsu ta hanya ɗaya ba. Abubuwa irin su shekaru na iya yin tasiri mai mahimmanci akan hanyar da mutum yake jurewa da gano cutar kansar nono. Matan da suka riga sun kamu da cutar kansar nono mai isrogen-receptor tabbatacce dole ne su fuskanci al'amurran da suka shafi farkon menopause da yawancin tsarin ilimin chemotherapy da ake amfani da su don magance ciwon nono, musamman waɗanda ke amfani da hormones don magance aikin ovarian.
A cikin mata masu ciwon nono ba na metastatic ba, abubuwan da suka shafi tunanin mutum irin su farfagandar halayya na iya samun tasiri mai kyau akan sakamako kamar damuwa, damuwa da damuwa yanayi. Ayyukan motsa jiki na iya samun tasiri masu fa'ida akan ingancin rayuwa mai alaƙa da lafiya, damuwa, dacewa da kuma motsa jiki a cikin mata masu fama da ciwon nono biyo bayan maganin adjuvant.
Epidemiology
[gyara sashe | gyara masomin]
| no data <2 2–4 4–6 6–8 8–10 10–12 | 12–14 14–16 16–18 18–20 20–22 >22 |
A duk duniya, cutar kansar nono ita ce cutar kansa mafi yawan kamuwa da ita a cikin mata. Tare da kansar huhu, kansar nono ita ce cutar kansa da aka fi sani da ita, tare da mutane miliyan 2.09, kowanne a cikin 2018. Ciwon daji yana shafar 1, cikin 7 (14%) na mata a duniya. (Mafi yawan nau'in ciwon daji shine ciwon fata wanda ba melanoma ba; ciwon daji marasa cutarwa gaba ɗaya ana warkewa cikin sauƙi, yana haifar da mutuwar mutane kaɗan, kuma ana cire su akai-akai daga kididdigar ciwon daji.) Ciwon daji na nono ya ƙunshi kashi 22.9% na ciwon daji na mata. da kuma kashi 16% na dukkan ciwon daji na mata. A cikin 2012, ya ƙunshi kashi 25.2% na cututtukan daji da aka gano a cikin mata, wanda ya sa ya zama cutar kansa mafi yawan mata.
A cikin 2008, ciwon nono ya haifar da mutuwar 458,503, a duk duniya (13.7% na mutuwar ciwon daji a cikin mata da kashi 6.0% na duk mutuwar ciwon daji ga maza da mata tare). Ciwon daji na huhu, na biyu mafi yawan sanadin mutuwar ciwon daji a cikin mata, ya haifar da 12.8% na mutuwar ciwon daji a cikin mata (kashi 18.2% na duk mutuwar ciwon daji ga maza da mata tare).
Yawan cutar kansar nono ya bambanta sosai a duniya: ya fi ƙanƙanta a ƙasashe masu ƙarancin ci gaba kuma mafi girma a cikin ƙasashe masu tasowa. A cikin yankuna goma sha biyu na duniya, adadin shekarun da suka dace na shekara-shekara a cikin mata 100,000, sune kamar haka: 18, a Gabashin Asiya, 22 a Kudancin Tsakiyar Asiya da Afirka kudu da Sahara, 26, a Kudu maso Gabashin Asiya, 26, 28, a Arewacin Afirka da Yammacin Asiya, 42 a Kudancin Amurka, 42, 49 a Gabashin Turai, 56 a Kudancin Turai, 73, a Arewacin Turai, 74 a Oceania, 78, a Yammacin Turai, 90, a Arewacin Amurka. Metastatic ciwon daji na nono yana shafar tsakanin kashi 19% (Amurka) da 50% (sassan Afirka) na mata masu ciwon nono.
Adadin shari'o'in a duk duniya ya karu sosai tun daga shekarun 1970, al'amarin da aka danganta shi da salon rayuwa na zamani. Ciwon daji na nono yana da alaƙa mai ƙarfi da shekaru tare da kawai kashi 5% na duk cutar kansar nono da ke faruwa a cikin mata masu ƙasa da shekaru 40. Akwai fiye da 41,000 sabbin kamuwa da cutar kansar nono da aka yiwa rajista a Ingila a cikin 2011, kusan kashi 80% na waɗannan cututtukan suna cikin mata masu shekaru 50 ko sama da haka. Dangane da kididdigar Amurka a cikin 2015 akwai mata miliyan 2.8 da suka kamu da cutar kansar nono. A {asar Amirka, shekarun da suka dace da cutar sankarar nono a cikin mata 100,000, sun tashi daga kusan lokuta 102, a kowace shekara a cikin 1970s zuwa kusa da 141, a ƙarshen 1990s, kuma tun daga lokacin ya fadi, yana da tsayi a kusa da 125, tun 2003. Duk da haka, shekaru Adadin mace-mace daga cutar kansar nono a cikin mata 100,000, kawai ya karu daga 31.4, a 1975, zuwa 33.2, a 1989, kuma tun daga nan ya ragu a hankali zuwa 20.5,a 2014.
Tarihi.
[gyara sashe | gyara masomin]
Saboda ganinsa, ciwon nono shine nau'in ciwon daji da aka fi kwatanta shi a cikin tsoffin takardu. Domin yin gwajin gawarwaki ba kasafai ba ne, ciwon daji na gabobin ciki ba sa iya ganin likita na da. Ciwon daji na nono, duk da haka, ana iya jin shi ta fata, kuma a cikin yanayin da ya ci gaba sau da yawa yakan zama cututtukan fungating: ciwon daji zai zama necrotic (ya mutu daga ciki, yana haifar da ciwon daji ya bayyana ya rabu) kuma ya shiga cikin fata, yana kuka. fetid, ruwa mai duhu.
Tsohuwar shaidar da aka gano na cutar kansar nono ta fito ne daga Masar kuma ta samo asali ne tun shekaru 4200, zuwa daular shida. Binciken da aka yi na gawar mace daga necropolis na Qubbet el-Hawa ya nuna irin lalacewar da aka saba yi saboda yaduwar ƙwayar cuta. Littafin Edwin Smith Papyrus ya bayyana lokuta takwas na ciwace-ciwacen ciwace-ciwace ko gyambon nono da aka yi amfani da su ta hanyar cauterization. Rubutun ya ce game da cutar, "Babu magani." Shekaru aru-aru, likitoci sun bayyana irin wannan lamari a cikin ayyukansu, tare da wannan ƙarshe. Magani na da, tun daga zamanin Helenawa har zuwa karni na 17, ya dogara ne akan sha'awar jima'i, don haka sunyi imani cewa ciwon nono yana haifar da rashin daidaituwa a cikin ainihin ruwan da ke sarrafa jiki, musamman ma wuce haddi na bile. A madadin haka ana ganinsa a matsayin azaba.
An yi Mastectomy don ciwon nono aƙalla a farkon AD 548, lokacin da likitan kotu Aetios na Amida ya ba da shawara ga Theodora. Sai da likitoci suka sami ƙarin fahimtar tsarin jini a cikin ƙarni na 17, da za su iya danganta yaduwar cutar kansar nono zuwa ƙwayoyin lymph a cikin hammata. A farkon karni na 18, Likitan Faransa Jean Louis Petit ya yi jimlar mastectomies waɗanda suka haɗa da cire ƙwayoyin lymph na axillary, yayin da ya gane cewa wannan ya rage sake dawowa. Aikin Petit da aka gina akan hanyoyin likitan fiɗa Bernard Peyrilhe, wanda a cikin karni na 17 ya kuma cire tsokar pectoral da ke ƙarƙashin ƙirjin, yayin da ya yanke hukuncin cewa hakan ya inganta hasashen sosai. Amma rashin sakamako mai kyau da kuma babban haɗari ga majiyyaci yana nufin cewa likitoci ba su raba ra'ayin likitocin tiyata irin su Nicolaes Tulp, wanda a cikin karni na 17, ya yi shelar "maganin kawai shine aikin da ya dace". Fitaccen likitan fida Richard Wiseman ya rubuta a tsakiyar karni na 17, cewa bayan mastectomies 12, marasa lafiya biyu sun mutu a yayin aikin, marasa lafiya takwas sun mutu jim kadan bayan tiyata daga ciwon daji na ci gaba kuma biyu kawai daga cikin 12, marasa lafiya sun warke. Likitoci sun kasance masu ra'ayin mazan jiya a cikin maganin da suka rubuta a farkon matakan ciwon nono. An yi wa marasa lafiya magani tare da cakuda kayan wankewa, barin jini da magungunan gargajiya waɗanda ya kamata su rage yawan acidity, irin su alkaline arsenic.

Lokacin a cikin 1664, An gano Anne ta Ostiriya tana da ciwon nono, jiyya ta farko ta haɗa da matsewa cike da ruwan 'ya'yan itacen hemlock. Lokacin da kullu ya karu sai likitan sarki ya fara magani da man shafawa na arsenic. Mai haƙuri na sarauta ya mutu 1666, a cikin mummunan zafi. Kowace kasawar maganin cutar sankarar nono ya haifar da neman sababbin magunguna, ta haifar da kasuwa a cikin magungunan da aka yi tallar da su ta hanyar quacks, herbalists, chemists da apothecaries. Rashin maganin sa barci da maganin kashe kwayoyin cuta sun sa mastectomy ya zama jaraba mai raɗaɗi da haɗari. A cikin karni na 18, nau'ikan bincike-bincike iri-iri sun kasance tare da sabbin ka'idoji game da sanadi da haɓakar cutar sankarar nono. Likitan binciken John Hunter ya yi iƙirarin cewa ruwan jijiya ya haifar da kansar nono. Sauran likitocin tiyata sun ba da shawarar cewa madara a cikin mammary ducts ya haifar da ci gaban ciwon daji. An ci gaba da ra'ayoyin game da rauni ga ƙirjin a matsayin sanadin muggan canje-canje a cikin ƙwayar nono. Gano kutun nono da kumbura ya haifar da cece-kuce game da ciwace-ciwacen ciwace-ciwacen daji da kuma ko kullun matakan ciwon daji ne. Ra'ayin likita game da magani na gaggawa da ake bukata ya bambanta. Likitan fiɗa Benjamin Bell ya ba da shawarar cire nono gabaɗaya, koda kuwa wani yanki ne kawai ya shafa.
Ciwon daji na nono ya kasance ba a saba gani ba har zuwa karni na 19, lokacin da ingantuwar tsafta da kula da cututtuka masu saurin kisa ya haifar da karuwa mai yawa a tsawon rayuwa. A baya, yawancin mata sun mutu suna ƙanana don kamuwa da cutar kansar nono. A cikin shekarar 1878, wata kasida a cikin Scientific American ta bayyana maganin tarihi ta hanyar matsin lamba da aka yi niyya don haifar da ischemia na gida a lokuta lokacin da cirewar tiyata ba zai yiwu ba. William Stewart Halsted ya fara aiwatar da mastectomies masu tsattsauran ra'ayi a cikin shekara ta 1882, ya taimaka sosai ta hanyar ci gaban fasahar fiɗa ta gabaɗaya, kamar fasahar aseptic da maganin sa barci. Mastectomy mai tsattsauran ra'ayi na Halsted sau da yawa ya ƙunshi cire ƙirjin biyu, ƙwayoyin lymph masu alaƙa, da kuma tsokoki na ƙirji. Wannan yakan haifar da jin zafi da nakasa na dogon lokaci, amma ana ganin ya zama dole don hana ciwon daji sake dawowa. Kafin zuwan mastectomy mai tsattsauran ra'ayi na Halsted, adadin tsira na shekaru 20, ya kasance 10% kawai; Tiyatar Halsted ta haɓaka adadin zuwa kashi 50%.
An haɓaka tsarin sarrafa kansar nono a cikin shekarar 1920s, da 1930s, don tantance gwargwadon yadda ciwon daji ya haɓaka ta girma da yaduwa. Binciken farko da aka sarrafa akan cutar sankarar nono Janet Lane-Claypon ya yi, wacce ta buga wani binciken kwatankwacin a 1926, na cututtukan nono 500, da kuma sarrafa 500, na asali iri ɗaya da salon rayuwa ga Ma'aikatar Lafiya ta Burtaniya. Mastectomies masu tsattsauran ra'ayi sun kasance daidaitattun kulawa a cikin Amurka har zuwa shekarun 1970, amma a cikin Turai, hanyoyin hana nono, galibi ana bi da su ta hanyar radiation far, gabaɗaya a cikin shekara ta 1950s. A cikin shekarar 1955, George Crile Jr. ya buga Cancer and Common Sense yana jayayya cewa masu ciwon daji suna buƙatar fahimtar zaɓuɓɓukan magani. Crile ta zama abokiyar abokiyar muhalli Rachel Carson, wacce ta yi mastectomy na Halsted a shekarar 1960, don magance cutar kansar nono. Masanin ilimin cututtukan daji na Amurka Jerome Urban ya haɓaka mastectomy na sama, yana ɗaukar ƙarin nama, har zuwa shekara ta 1963, lokacin da adadin tsira na shekaru goma ya yi daidai da ƙarancin mastectomy na raɗaɗi. Carson ya mutu a shekara ta 1964, kuma Crile ya ci gaba da buga labarai iri-iri, duka a cikin shahararrun jaridu da kuma a cikin mujallolin likita, yana ƙalubalantar yadda ake amfani da shi na mastectomy na Halsted. A cikin shekara ta 1973, Crile ya buga Abin da Mata Ya Kamata Su Sani Game da Rigimar Ciwon Kan Nono. Lokacin da a cikin shekarar 1974, Betty Ford aka gano da ciwon nono, zažužžukan don magance ciwon nono an tattauna a fili a cikin manema labarai. A cikin shekarun 1970s, sabon fahimtar metastasis ya haifar da fahimtar ciwon daji a matsayin rashin lafiya na tsari da kuma wanda aka keɓe, kuma an ɓullo da ƙarin hanyoyin kiyayewa waɗanda suka tabbatar da tasiri daidai.
A cikin shekarun 1980 da shekarar 1990, dubunnan matan da suka yi nasarar kammala jiyya na yau da kullun, sannan suka nemi da dashen kasusuwa masu yawa, suna tunanin hakan zai haifar da mafi kyawun rayuwa na dogon lokaci. Duk da haka, ya tabbatar da rashin tasiri, kuma 15-20% na mata sun mutu saboda rashin tausayi. Rahotonni na 1995, daga Nazarin Kiwon Lafiyar Ma'aikatan Jiyya da kuma ƙarshen shekara ta 2002, na gwajin Ƙaddamarwar Lafiyar Mata ya tabbatar da cewa maganin maye gurbin hormone yana ƙaruwa da kamuwa da cutar kansar nono.
Al'umma da al'adu.
[gyara sashe | gyara masomin]Kafin karni na 20, ana jin tsoron cutar kansar nono kuma ana tattaunawa da su cikin sautin murya, kamar abin kunya ne. Kamar yadda za a iya yin kadan cikin aminci tare da dabarun tiyata na farko, mata sun kasance suna shan wahala a shiru maimakon neman kulawa. Lokacin da aikin tiyata ya ci gaba, kuma adadin rayuwa na dogon lokaci ya inganta, mata sun fara wayar da kan jama'a game da cutar da yiwuwar samun nasarar maganin. Jam'iyyar Fisher na '' ', al'ummar Amurka suna shirin karfin cutar kansa (daga baya Amurkawa na kasar Sin) a cikin shekara ta 1930s, da shekarar 1940s, ya kasance daya daga cikin kamfen da aka shirya na farko. A shekara ta 1952, ƙungiyar tallafi ta farko-da-tsara, mai suna "Isa zuwa farfadowa", ta fara ba da bayan-mastectomy, ziyara a asibiti daga matan da suka tsira daga cutar kansar nono.
Motsin kansar nono na shekarun 1980,,da shekarar 1990 ya samo asali ne daga manyan ƙungiyoyin mata da harkar lafiyar mata na ƙarni na 20. Wannan jerin yaƙin neman zaɓe na siyasa da na ilimi, wani ɓangare na yaƙin neman zaɓe na wayar da kan jama'a game da cutar AIDS na siyasa da zamantakewa, ya haifar da karɓuwar ra'ayi na biyu kafin tiyata, ƙarancin hanyoyin tiyata, ƙungiyoyin tallafi, da sauran ci gaban kulawa.
Pink ribbon
[gyara sashe | gyara masomin]
Rubutun ruwan hoda shine fitacciyar alamar wayar da kan cutar sankarar nono. Ribbons masu ruwan hoda, waɗanda za a iya yin su da tsada, wasu lokuta ana siyar da su azaman masu tara kuɗi, kamar poppies a Ranar Tunawa. Ana iya sanya su don girmama waɗanda aka gano suna da cutar kansar nono, ko don gano samfuran da masana'anta ke son sayar wa masu amfani da ke sha'awar ciwon nono. A cikin 1990s kamfanoni na Amurka sun ƙaddamar da yaƙin wayar da kan cutar kansar nono. A matsayin wani ɓangare na waɗannan kamfen ɗin tallace-tallace masu alaƙa da kamfanoni sun ba da gudummawa ga nau'ikan ayyukan kansar nono don kowane samfurin ribbon ruwan hoda da aka siya. Jaridar Wall Street Journal ta lura cewa "ƙarfin motsin zuciyar da ciwon nono ke haifarwa yana fassara zuwa layin kamfani". Yayin da yawancin kamfanoni na Amurka suka ba da gudummawa ga ci gaban cutar kansar nono wasu kamar su Avon sun kafa nasu tushen kansar nono a bayan samfuran ribbon ruwan hoda.
Masu adawa da wannan al'ada sun soki sawa ko nuna kintinkiri mai ruwan hoda a matsayin wani nau'i na slacktivism, saboda ba shi da wani tasiri mai kyau a aikace. An kuma yi suka da cewa munafunci ne, domin wasu suna sanya ratsin ruwan hoda don nuna kyakkyawar niyya ga mata masu fama da cutar kansar nono, amma sai suka yi adawa da wadannan manufofin mata na aiki, kamar hakkin marasa lafiya da kuma dokar hana gurbata muhalli. Masu suka dai sun ce yanayin jin dadin ribbon ruwan hoda da shan ruwan hoda yana dauke hankalin al’umma daga rashin samun ci gaba wajen yin rigakafi da magance cutar sankarar mama. Ana kuma soki lamirin karfafa ra'ayin jinsi da kuma bata mata da nononsu. A cikin shekara ta 2002, Action Cancer Action ƙaddamar da "Think Kafin Ka Pink" yaƙin neman zaɓe ga harkokin kasuwanci da suka haɗa kai da ruwan hoda kamfen don inganta kayayyakin da ke haifar da ciwon nono, kamar giya.
Al'adar ciwon nono.
[gyara sashe | gyara masomin]A cikin littafinta na shekarar 2006, Pink Ribbons, Inc.: Breast Cancer and the Politics of Philanthropy Samantha King ta yi iƙirarin cewa an canza kansar nono daga mummunar cuta da bala'i na mutum zuwa masana'antar tsira da kasuwancin kasuwanci. A cikin shekara ta 2010, Gayle Sulik ya bayar da hujjar cewa dalilai na farko ko manufofin al'adar cutar kansar nono su ne don kula da kansar nono a matsayin babban abin da ya shafi lafiyar mata, don haɓaka kamannin cewa al'umma na yin wani abu mai tasiri game da cutar kansar nono, da ci gaba da faɗaɗa. ikon zamantakewa, siyasa, da kuɗi na masu fafutukar cutar kansar nono A cikin wannan shekarar Barbara Ehrenreich ta buga wani ra'ayi a cikin Mujallar Harper, tana kuka cewa a al'adar cutar kansar nono, ana kallon maganin kansar nono a matsayin al'ada maimakon cuta. Don dacewa da wannan nau'in, macen da ke fama da ciwon nono na buƙatar daidaitawa da kuma daidaita kamanninta, da kuma rage rushewar da al'amuran lafiyarta ke haifar da wani. Dole ne a rufe fushi, bakin ciki, da rashin fahimta. Kamar yadda yawancin nau'ikan al'adu, mutanen da suka dace da samfurin suna ba da matsayi na zamantakewa, a cikin wannan yanayin a matsayin masu tsira da ciwon daji. Matan da suka ƙi samfurin an guje su, azabtarwa da kunya. An soki al'adar game da daukar mata manya kamar kananan 'yan mata, kamar yadda abubuwan wasan kwaikwayo na "jarirai" suka nuna irin su ruwan hoda na teddy bears da aka ba wa mata masu girma.
Jaddawa.
[gyara sashe | gyara masomin]A shekara ta 2009, wata 'yar jarida a kimiyyar Amurka Christie Aschwanden ta soki cewa fifikon da aka fi mayar da hankali kan tantance cutar sankarar nono na iya cutar da mata ta hanyar sanya su radiation, biopsies, da tiyata marasa amfani. Kashi ɗaya bisa uku na cutar kansar nono da aka gano na iya komawa da kansu. Duban mammography da kyau yana gano marasa lafiya da rai, cututtukan daji na nono da asymptomatic, ko da yake ana yin watsi da manyan cututtukan daji. A cewar mai binciken cutar kansa, H. Gilbert Welch, mai binciken mammography ya ɗauki “hanyar mutuwa ta ƙwaƙwalwa wacce ta ce mafi kyawun gwajin ita ce wanda ke gano mafi yawan cutar kansa” maimakon wanda ke gano kansar masu haɗari.
A shekara ta 2002, an lura da cewa, sakamakon bayyanar cutar kansar nono, ana iya yin kuskuren fassara sakamakon ƙididdiga, kamar iƙirarin cewa mace ɗaya cikin takwas za ta kamu da cutar kansar nono a lokacin rayuwarsu - iƙirarin da ya dogara da zato maras tabbas cewa. babu wata mace da za ta mutu da kowace irin cuta kafin ta kai shekara 95. A shekarar 2010 yawan cutar kansar nono a Turai ya kai kashi 91% a shekara daya da kashi 65% a shekaru biyar. A cikin Amurka, adadin shekarun rayuwa na shekaru biyar don cutar kansar nono ya kasance 96.8%, yayin da a lokuta na metastases ya kasance kawai 20.6%. Domin hasashen cutar kansar nono a wannan mataki yana da kyau sosai, idan aka kwatanta da hasashen sauran cututtukan, cutar sankarar nono a matsayin sanadin mutuwar mata shine kashi 13.9% na yawan mace-macen cutar kansa. Abu na biyu da ya fi zama sanadin mutuwar mata daga cutar kansa shi ne kansar huhu, cutar daji da ta fi kamari a duniya ga maza da mata. Ingantacciyar adadin tsira ya sa kansar nono ya zama cutar kansa mafi yaɗuwa a duniya. A cikin 2010, kimanin mata miliyan 3.6, a duk duniya sun kamu da cutar kansar nono a cikin shekaru biyar da suka gabata, yayin da maza ko mata miliyan 1.4,kawai suka tsira daga cutar kansar huhu suna raye.
Bambance-bambancen kabilanci.
[gyara sashe | gyara masomin]Akwai bambance-bambancen kabilanci a cikin adadin mace-macen cutar kansar nono da kuma na maganin cutar kansar nono. Kansar nono ita ce cutar sankara mafi yaduwa da ke shafar mata na kowace kabila a Amurka. Yawan cutar kansar nono a tsakanin mata bakar fata masu shekaru 45, zuwa sama ya zarce na farare mata masu shekaru daya. Fararen mata masu shekaru 60-84, suna da yawan kamuwa da cutar kansar nono fiye da matan Baƙar fata. Duk da haka, mata baƙar fata a kowane zamani sun fi kamuwa da cutar kansar nono.
Maganin ciwon daji na nono ya samu ci gaba sosai a cikin 'yan shekarun nan, amma har yanzu baƙar fata ba sa samun magani idan aka kwatanta da farar fata. Abubuwan haɗari kamar yanayin zamantakewa, ƙarshen zamani, ko ciwon nono a ganewar asali, bambance-bambancen kwayoyin halitta a cikin nau'in ciwon daji, bambance-bambancen samun damar kula da lafiya duk suna ba da gudummawa ga waɗannan bambance-bambance. Abubuwan da ke tabbatar da tattalin arziƙin zamantakewa da ke shafar rarrabuwar kawuna a cikin cutar kansar nono sun haɗa da talauci, al'adu, da kuma rashin adalci na zamantakewa. A cikin matan Hispanic, kamuwa da cutar kansar nono ya yi ƙasa da na matan da ba na Hispanic ba amma galibi ana bincikar su a wani mataki na gaba fiye da farar fata masu ciwon sukari.
Mata bakar fata yawanci ana samun cutar kansar nono tun suna kanana fiye da farare. Tsakanin shekarun ganewar asali ga mata baƙar fata shine 59, idan aka kwatanta da 62, a cikin fararen mata. Yawan cutar kansar nono a cikin mata baƙar fata ya karu da 0.4% a kowace shekara tun daga 1975, da 1.5% a kowace shekara a tsakanin matan Asiya/Pacific na Asiya tun daga 1992. Yawan abubuwan da suka faru sun kasance masu karko ga waɗanda ba na Hispanic White, Hispanics, da mata na asali ba. Adadin tsira na shekaru biyar an lura ya zama 81% a cikin mata baƙar fata da 92% a cikin mata farare. Matan Sinawa da Jafanawa ne ke da mafi girman adadin rayuwa.
Talauci shine babban abin da ke haifar da bambance-bambancen da ke da alaka da ciwon nono. Mata masu karamin karfi ba su da yuwuwar a yi gwajin cutar kansar nono don haka ana iya samun cutar da wuri. Tabbatar da cewa mata na kowane kabila sun sami daidaiton kulawar lafiya [bayani da ake buƙata] na iya shafar waɗannan bambance-bambance.
Ciki
[gyara sashe | gyara masomin]Ciki tun yana ƙarami yana rage haɗarin kamuwa da cutar kansar nono daga baya a rayuwa. Haɗarin cutar kansar nono kuma yana raguwa tare da adadin yaran da mace ke da su. Ciwon daji na nono ya zama ruwan dare a cikin shekaru 5, ko 10, bayan daukar ciki amma sai ya zama kasa gama gari fiye da yawan jama'a. An san waɗannan cututtukan daji da kansar nono bayan haihuwa kuma suna da sakamako mafi muni gami da ƙara haɗarin yaduwar cututtuka da mace-mace. Sauran ciwon daji da ake samu a lokacin ko kuma jim kadan bayan daukar ciki suna bayyana a kusan daidai da sauran cututtukan daji na mata masu shekaru makamancin haka.
Gano sabon ciwon daji a cikin mace mai ciki yana da wahala, a wani ɓangare saboda duk wani alamun da aka saba ɗauka a matsayin rashin jin daɗi na yau da kullun da ke hade da ciki. A sakamakon haka, ciwon daji yawanci ana gano shi a wani ɗan lokaci kaɗan fiye da matsakaici a yawancin mata masu juna biyu ko kwanan nan. Wasu hanyoyin hoto, irin su MRIs (hoton maganadisu na maganadisu), CT scans, ultrasounds, da mammograms tare da garkuwar tayin ana ɗaukar lafiya yayin daukar ciki; wasu, kamar PET scans ba su.
Magani gabaɗaya iri ɗaya ne da na mata marasa ciki. Duk da haka, ana guje wa radiation yawanci lokacin daukar ciki, musamman idan adadin tayin zai iya wuce 100 cGy. A wasu lokuta, ana jinkirta wasu ko duka jiyya har sai bayan haihuwa idan an gano ciwon daji a ƙarshen ciki. Bayarwa da wuri don saurin fara jiyya ba sabon abu bane. Gabaɗaya ana ɗaukar tiyatar lafiya yayin da take ɗauke da juna biyu, amma wasu magunguna, musamman wasu magungunan chemotherapy da ake ba su a farkon watanni uku na farko, suna ƙara haɗarin lahani na haihuwa da asarar ciki (zubar da ciki da haihuwa da haihuwa). Ba a buƙatar zubar da ciki da aka zaɓa kuma baya inganta yuwuwar mahaifiyar ta tsira ko kuma ta warke.
Maganin radiyo na iya kawo cikas ga iyawar uwa wajen shayar da jaririnta saboda yana rage karfin nonon don samar da madara kuma yana kara haɗarin mastitis. Har ila yau, lokacin da ake ba da maganin chemotherapy bayan haihuwa, yawancin magungunan suna wucewa ta cikin nono zuwa jariri, wanda zai iya cutar da jariri.
Game da ciki nan gaba tsakanin masu tsira da ciwon nono, galibi ana jin tsoron sake bullowar cutar kansa. A gefe guda, mutane da yawa har yanzu suna la'akari da ciki da haihuwa don wakiltar al'ada, farin ciki da cikar rayuwa.
Hormones.
[gyara sashe | gyara masomin]Kulawar haihuwa.
[gyara sashe | gyara masomin]A cikin waɗanda suka tsira daga cutar kansar nono, hanyoyin hana haihuwa waɗanda ba na hormonal ba kamar na'urar intrauterine ta jan ƙarfe (IUD) yakamata a yi amfani da su azaman zaɓin layin farko. Hanyoyin tushen progestogen irin su depot medroxyprogesterone acetate, IUD tare da progestogen ko progestogen kawai kwayoyin suna da mummunan bincike amma yiwuwar karuwar cutar ciwon daji, amma ana iya amfani da su idan tasiri mai kyau ya fi wannan haɗari mai yiwuwa.
Menopause hormone maye gurbin.
[gyara sashe | gyara masomin]A cikin wadanda suka tsira daga ciwon nono, ana bada shawara don fara la'akari da zaɓuɓɓukan da ba na hormonal ba don tasirin menopause, irin su bisphosphonates ko masu zaɓin masu karɓar isrogen receptor (SERMs) don osteoporosis, da estrogen na farji don alamun gida. Nazarin lura na tsarin maye gurbin hormone bayan ciwon nono yana ƙarfafawa gabaɗaya. Idan maye gurbin hormone ya zama dole bayan ciwon nono, maganin estrogen-kawai ko maganin estrogen tare da na'urar intrauterine tare da progestogen na iya zama mafi aminci zaɓuɓɓuka fiye da haɗin tsarin tsarin.
Bincike.
[gyara sashe | gyara masomin]Ana kimanta jiyya a gwaji na asibiti. Wannan ya haɗa da magungunan mutum ɗaya, haɗaɗɗun magunguna, da hanyoyin tiyata da fasahar radiation Bincike ya haɗa da sabbin nau'ikan jiyya da aka yi niyya, rigakafin cutar kansa, oncolytic virotherapy, jiyya na ƙwayoyin cuta da rigakafi.
Ana ba da rahoton sabon bincike a kowace shekara a tarurrukan kimiyya kamar na American Society of Clinical Oncology, San Antonio Breast Cancer Symposium, da St. Gallen Oncology Conference a St. Gallen, Switzerland. Ƙungiyoyin ƙwararru da wasu ƙungiyoyi ne suke nazarin waɗannan karatun, kuma an tsara su cikin ƙa'idodi don takamaiman ƙungiyoyin jiyya da nau'in haɗari.
Fenretinide, wani retinoid, kuma ana nazarinsa a matsayin hanyar rage haɗarin cutar kansar nono. Musamman, haɗuwa da ribociclib tare da maganin endocrin sun kasance batun gwaji na asibiti.
Wani bita na shekara ta 2019, ya sami tabbataccen tabbaci na matsakaici cewa bai wa mutane maganin rigakafi kafin tiyatar kansar nono ya taimaka wajen hana kamuwa da cutar ta wurin tiyata (SSI). Ana buƙatar ƙarin bincike don ƙayyade ƙa'idar maganin rigakafi mafi inganci da amfani ga matan da ke fuskantar gyaran nono nan take.
Cryoablation.
[gyara sashe | gyara masomin]Kamar yadda na shekarar 2014, cryoablation ana nazarin don ganin ko zai iya zama madadin lumpectomy a cikin ƙananan cututtuka. Akwai shaida ta ƙarshe a cikin waɗanda ke da ciwace-ciwacen da bai wuce santimita 2, ba. Hakanan ana iya amfani dashi a cikin waɗanda tiyata ba zai yiwu ba. Wani bita ya nuna cewa cryoablation ya dubi alamar alamar ciwon nono na farko na ƙananan ƙananan.
Layukan kwayar cutar kansar nono
[gyara sashe | gyara masomin]Wani ɓangare na ilimin halin yanzu game da ciwon daji na nono ya dogara ne akan in vivo da in vitro binciken da aka yi tare da layin salula da aka samo daga ciwon nono. Waɗannan suna ba da tushe marar iyaka na kayan kwafin kai mai kama da juna, ba tare da gurɓata ƙwayoyin jijiyoyi ba, kuma sau da yawa ana al'adarsu cikin sauƙi daidaitaccen kafofin watsa labarai. Layin kwayar cutar kansar nono na farko da aka kwatanta, BT-20, an kafa shi a cikin 1958. Tun daga wannan lokacin, kuma duk da ci gaba da aiki a wannan yanki, adadin layin dindindin da aka samu ya kasance mai ban mamaki (kimanin 100). Lallai, yunƙurin al'adar layukan ƙwayoyin cutar kansar nono daga ciwace-ciwacen farko bai yi nasara ba. Wannan rashin inganci sau da yawa yakan faru ne saboda matsalolin fasaha da ke da alaƙa da haɓakar ƙwayoyin ƙwayar cuta mai ƙarfi daga maƙarƙashiya da ke kewaye da su. Yawancin layukan sel kansar nono da ake samu daga ciwace-ciwacen ƙwayar cuta, galibi daga zubar da jini. Zubar da ciki yana ba da lambobi masu yawa na rarrabuwar kawuna, ƙwayoyin ƙwayar cuta masu yuwuwa waɗanda ke da ɗan ko babu gurɓata ta fibroblasts da sauran ƙwayoyin ƙwayar cuta. Yawancin layukan BCC da ake amfani da su a halin yanzu an kafa su a ƙarshen 1970s. Kadan daga cikinsu, wato MCF-7, T-47D, MDA-MB-231 da SK-BR-3, sun kai sama da kashi biyu bisa uku na duk binciken da aka yi a kan layukan ciwon nono, kamar yadda aka kammala daga Binciken tushen layi.
Alamar kwayoyin halitta
[gyara sashe | gyara masomin]Metabolic markers
[gyara sashe | gyara masomin]A asibiti, mafi amfani alamomi na rayuwa a cikin ciwon nono shine estrogen da progesterone masu karɓa waɗanda ake amfani da su don tsinkayar amsa ga maganin hormone. Sabbin alamomi ko yuwuwar sabbin alamun cutar kansar nono sun haɗa da BRCA1 da BRCA2 don gano mutanen da ke cikin haɗarin kamuwa da cutar kansar nono, HER-2, [abubuwan da ake buƙata na likita] da SCD1, don tsinkayar martani ga tsarin warkewa, da urokinase plasminogen activator, PA1-1 da SCD1 don tantance hasashen.
Manazarta.
[gyara sashe | gyara masomin]- ↑ "Breast Cancer". NCI. January 1980. Archived from the original on 25 June 2014. Retrieved 29 June 2014.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 "Breast Cancer Treatment (PDQ®)". NCI. 23 May 2014. Archived from the original on 5 July 2014. Retrieved 29 June 2014.
- ↑ Saunders C, Jassal S (2009). Breast cancer (1. ed.). Oxford: Oxford University Press. p. Chapter 13. ISBN 978-0-19-955869-8. Archived from the original on 25 October 2015.
- ↑ 4.0 4.1 World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 5.2. ISBN 978-92-832-0429-9.
- ↑ Gøtzsche PC, Jørgensen KJ (June 2013). "Screening for breast cancer with mammography". The Cochrane Database of Systematic Reviews. 6 (6): CD001877. doi:10.1002/14651858.CD001877.pub5. PMC 6464778. PMID 23737396.
- ↑ Nelson HD, Tyne K, Naik A, Bougatsos C, Chan B, Nygren P, Humphrey L (November 2009). "Screening for Breast Cancer: Systematic Evidence Review Update for the US Preventive Services Task Force [Internet]". U.S. Preventive Services Task Force Evidence Syntheses. Rockville, MD: Agency for Healthcare Research and Quality. PMID 20722173. Report No.: 10-05142-EF-1.
- ↑ Siu AL (February 2016). "Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement". Annals of Internal Medicine. 164 (4): 279–96. doi:10.7326/M15-2886. PMID 26757170
- ↑ Siu AL (February 2016). "Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement". Annals of Internal Medicine. 164 (4): 279–96. doi:10.7326/M15-2886. PMID 26757170.
- ↑ "Five Things Physicians and Patients Should Question". Choosing Wisely: an initiative of the ABIM Foundation. American College of Surgeons. September 2013. Archived from the original on 27 October 2013. Retrieved 2 January 2013.
- ↑ 10.0 10.1 10.2 "Breast Cancer Treatment (PDQ®)". NCI. 26 June 2014. Archived from the original on 5 July 2014. Retrieved 29 June 2014.
- ↑ 11.0 11.1 "World Cancer Report" (PDF). International Agency for Research on Cancer. 2008. Archived from the original (PDF) on 20 July 2011. Retrieved 26 February 2011.
- ↑ "SEER Stat Fact Sheets: Breast Cancer". NCI. Archived from the original on 3 July 2014. Retrieved 18 June 2014.
- ↑ "Cancer Survival in England: Patients Diagnosed 2007–2011 and Followed up to 2012" (PDF). Office for National Statistics. 29 October 2013. Archived (PDF) from the original on 29 November 2014. Retrieved 29 June 2014.
- ↑ World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 1.1. ISBN 978-92-832-0429-9.
- ↑ Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (November 2018). "Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries". CA: A Cancer Journal for Clinicians. 68 (6): 394–424. doi:10.3322/caac.21492. PMID 30207593. S2CID 52188256.
- ↑ "Male Breast Cancer Treatment". National Cancer Institute. 2014. Archived from the original on 4 July 2014. Retrieved 29 June 2014.
- ↑ 17.0 17.1 17.2 Merck Manual of Diagnosis and Therapy (February 2003). "Breast Disorders: Breast Cancer". Archived from the original on 2 October 2011. Retrieved 5 February 2008.
- ↑ 18.0 18.1 American Cancer Society (2007). "Cancer Facts & Figures 2007" (PDF). Archived from the original (PDF) on 10 April 2007. Retrieved 26 April 2007.
- ↑ Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, et al. (January 2007). "Mammographic density and the risk and detection of breast cancer". The New England Journal of Medicine. 356 (3): 227–36. doi:10.1056/NEJMoa062790. PMID 17229950.
- ↑ Watson M (2008). "Assessment of suspected cancer". InnoAiT. 1 (2): 94–107. doi:10.1093/innovait/inn001. S2CID 71908359.
- ↑ "Breast Cancer Evaluation". eMedicine. 23 August 2006. Archived from the original on 12 February 2008. Retrieved 5 February 2008.
- ↑ Ashikari R, Park K, Huvos AG, Urban JA (September 1970). "Paget's disease of the breast". Cancer. 26 (3): 680–5. doi:10.1002/1097-0142(197009)26:3<680::aid-cncr2820260329>3.0.co;2-p. PMID 4318756.
- ↑ Kollmorgen DR, Varanasi JS, Edge SB, Carson WE (August 1998). "Paget's disease of the breast: a 33-year experience". Journal of the American College of Surgeons. 187 (2): 171–7. doi:10.1016/S1072-7515(98)00143-4. PMID 9704964.
- ↑ Kleer CG, van Golen KL, Merajver SD (1 December 2000). "Molecular biology of breast cancer metastasis. Inflammatory breast cancer: clinical syndrome and molecular determinants". Breast Cancer Research. 2 (6): 423–9. doi:10.1186/bcr89. PMC 138665. PMID 11250736.
- ↑ answers.com. "Oncology Encyclopedia: Cystosarcoma Phyllodes". Answers.com. Archived from the original on 8 September 2010. Retrieved 10 August 2010.
- ↑ Lacroix M (December 2006). "Significance, detection and markers of disseminated breast cancer cells". Endocrine-Related Cancer. 13 (4): 1033–67. doi:10.1677/ERC-06-0001. PMID 17158753.
- ↑ "Stage 4 :: The National Breast Cancer Foundation". www.nationalbreastcancer.org.
- ↑ National Cancer Institute (1 September 2004). "Metastatic Cancer: Questions and Answers". Archived from the original on 27 August 2008. Retrieved 6 February 2008.
- ↑ National Cancer Institute (1 September 2004). "Metastatic Cancer: Questions and Answers". Archived from the original on 27 August 2008. Retrieved 6 February 2008.
- ↑ Perera N, Fernando N, Perera R (March 2020). "Metastatic breast cancer spread to peripancreatic lymph nodes causing biliary obstruction". The Breast Journal. 26 (3): 511–13. doi:10.1111/tbj.13531. PMID 31538691.
- ↑ Interpreting Signs and Symptoms. Lippincott Williams & Wilkins. 2007. pp. 99–. ISBN 978-1-58255-668-0.
- ↑ Merck Manual of Diagnosis and Therapy (February 2003). "Breast Disorders: Overview of Breast Disorders". Archived from the original on 3 October 2011. Retrieved 5 February 2008.
- ↑ Hayes J, Richardson A, Frampton C (November 2013). "Population attributable risks for modifiable lifestyle factors and breast cancer in New Zealand women". Internal Medicine Journal. 43 (11): 1198–204. doi:10.1111/imj.12256. PMID 23910051. S2CID 23237732.
- ↑ Reeder JG, Vogel VG (2008). "Breast cancer prevention". Advances in Breast Cancer Management, Second Edition. Cancer Treatment and Research. 141. pp. 149–64. doi:10.1007/978-0-387-73161-2_10. ISBN 978-0-387-73160-5. PMID 18274088.
- ↑ "Am I at risk?". Breast Cancer Care. 23 February 2018. Archived from the original on 25 October 2013. Retrieved 22 October 2013.
- ↑ Collaborative Group on Hormonal Factors in Breast Cancer (July 2002). "Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease". Lancet. 360 (9328): 187–95. doi:10.1016/S0140-6736(02)09454-0. PMID 12133652. S2CID 25250519.
- ↑ Yager JD, Davidson NE (January 2006). "Estrogen carcinogenesis in breast cancer". The New England Journal of Medicine. 354 (3): 270–82. doi:10.1056/NEJMra050776. PMID 16421368.
- ↑ Mazzucco A, Santoro E, DeSoto, M, Hong Lee J (February 2009). "Hormone Therapy and Menopause". National Research Center for Women & Families.
- ↑ Light Pollution as new risk factor for human Breast and Prostate Cancers- Haim, Abraham; Portnov, Biris P., 2013, 08033994793.ABA
- ↑ 40.0 40.1 Zhang, Yan-Bo; Pan, Xiong-Fei; Chen, Junxiang; Cao, Anlan; Zhang, Yu-Ge; Xia, Lu; Wang, Jing; Li, Huiqi; Liu, Gang; Pan, An (2020-03-31). "Combined lifestyle factors, incident cancer, and cancer mortality: a systematic review and meta-analysis of prospective cohort studies". British Journal of Cancer. 122 (7): 1085–1093. doi:10.1038/s41416-020-0741-x. ISSN 0007-0920. PMC 7109112. PMID 32037402.
- ↑ Choi, Yoon-Jung; Myung, Seung-Kwon; Lee, Ji-Ho (April 2018). "Light Alcohol Drinking and Risk of Cancer: A Meta-Analysis of Cohort Studies". Cancer Research and Treatment. 50 (2): 474–487. doi:10.4143/crt.2017.094. ISSN 2005-9256. PMC 5912140. PMID 28546524.
- ↑ 42.0 42.1 Shield KD, Soerjomataram I, Rehm J (June 2016). "Alcohol Use and Breast Cancer: A Critical Review". Alcoholism, Clinical and Experimental Research. 40 (6): 1166–81. doi:10.1111/acer.13071. PMID 27130687.
All levels of evidence showed a risk relationship between alcohol consumption and the risk of breast cancer, even at low levels of consumption.
- ↑ McDonald JA, Goyal A, Terry MB (September 2013). "Alcohol Intake and Breast Cancer Risk: Weighing the Overall Evidence". Current Breast Cancer Reports. 5 (3): 208–221. doi:10.1007/s12609-013-0114-z. PMC 3832299. PMID 24265860.
- ↑ "Lifestyle-related Breast Cancer Risk Factors". www.cancer.org.
- ↑ Blackburn GL, Wang KA (September 2007). "Dietary fat reduction and breast cancer outcome: results from the Women's Intervention Nutrition Study (WINS)". The American Journal of Clinical Nutrition. 86 (3): s878-81. doi:10.1093/ajcn/86.3.878S. PMID 18265482.
- ↑ BBC report Weight link to breast cancer risk Archived 13 ga Maris, 2007 at the Wayback Machine
- ↑ Kaiser J (November 2013). "Cancer. Cholesterol forges link between obesity and breast cancer". Science. 342 (6162): 1028. doi:10.1126/science.342.6162.1028. PMID 24288308.
- ↑ Aceves C, Anguiano B, Delgado G (April 2005). "Is iodine a gatekeeper of the integrity of the mammary gland?". Journal of Mammary Gland Biology and Neoplasia. 10 (2): 189–96. doi:10.1007/s10911-005-5401-5. PMID 16025225. S2CID 16838840.
- ↑ Aceves C, Anguiano B, Delgado G (April 2005). "Is iodine a gatekeeper of the integrity of the mammary gland?". Journal of Mammary Gland Biology and Neoplasia. 10 (2): 189–96. doi:10.1007/s10911-005-5401-5. PMID 16025225. S2CID 16838840.
- ↑ Mourouti N, Kontogianni MD, Papavagelis C, Panagiotakos DB (February 2015). "Diet and breast cancer: a systematic review". International Journal of Food Sciences and Nutrition. 66 (1): 1–42. doi:10.3109/09637486.2014.950207. PMID 25198160. S2CID 207498132.
- ↑ Aubrey A (1 February 2016). "A Diet High In Fiber May Help Protect Against Breast Cancer". NPR. Archived from the original on 1 February 2016. Retrieved 1 February 2016.
- ↑ 52.0 52.1 Johnson KC, Miller AB, Collishaw NE, Palmer JR, Hammond SK, Salmon AG, et al. (January 2011). "Active smoking and secondhand smoke increase breast cancer risk: the report of the Canadian Expert Panel on Tobacco Smoke and Breast Cancer Risk (2009)". Tobacco Control. 20 (1): e2. doi:10.1136/tc.2010.035931. PMID 21148114. S2CID 448229.
- ↑ Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT (July 2012). "Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy". Lancet. 380 (9838): 219–29. doi:10.1016/S0140-6736(12)61031-9. PMC 3645500. PMID 22818936.
- ↑ Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, Alter DA (January 2015). "Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis". Annals of Internal Medicine. 162 (2): 123–32. doi:10.7326/M14-1651. PMID 25599350. S2CID 7256176.
- ↑ Collaborative Group on Hormonal Factors in Breast Cancer (September 2019). "Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence". Lancet. 394 (10204): 1159–1168. doi:10.1016/S0140-6736(19)31709-X. PMC 6891893. PMID 31474332.
- ↑ Kanadys, Wiesław; Barańska, Agnieszka; Malm, Maria; Błaszczuk, Agata; Polz-Dacewicz, Małgorzata; Janiszewska, Mariola; Jędrych, Marian (2021-04-27). "Use of Oral Contraceptives as a Potential Risk Factor for Breast Cancer: A Systematic Review and Meta-Analysis of Case-Control Studies Up to 2010". International Journal of Environmental Research and Public Health. 18 (9): 4638. doi:10.3390/ijerph18094638. ISSN 1660-4601. PMC 8123798 Check
|pmc=value (help). PMID 33925599 Check|pmid=value (help). - ↑ 57.0 57.1 Chelmow, David; Pearlman, Mark D.; Young, Amy; Bozzuto, Laura; Dayaratna, Sandra; Jeudy, Myrlene; Kremer, Mallory E.; Scott, Dana Marie; O'Hara, Julia Sage (June 2020). "Executive Summary of the Early-Onset Breast Cancer Evidence Review Conference". Obstetrics and Gynecology. 135 (6): 1457–1478. doi:10.1097/AOG.0000000000003889. ISSN 0029-7844. PMC 7253192. PMID 32459439.
- ↑ Gaffield ME, Culwell KR, Ravi A (October 2009). "Oral contraceptives and family history of breast cancer". Contraception. 80 (4): 372–80. doi:10.1016/j.contraception.2009.04.010. PMID 19751860.
- ↑ Huber, D.; Seitz, S.; Kast, K.; Emons, G.; Ortmann, O. (April 2020). "Use of oral contraceptives in BRCA mutation carriers and risk for ovarian and breast cancer: a systematic review". Archives of Gynecology and Obstetrics. 301 (4): 875–884. doi:10.1007/s00404-020-05458-w. ISSN 1432-0711. PMC 8494665 Check
|pmc=value (help). PMID 32140806. - ↑ Chowdhury R, Sinha B, Sankar MJ, Taneja S, Bhandari N, Rollins N, et al. (December 2015). "Breastfeeding and maternal health outcomes: a systematic review and meta-analysis". Acta Paediatrica. 104 (467): 96–113. doi:10.1111/apa.13102. PMC 4670483. PMID 26172878.
- ↑ "Breastfeeding". World Health Organization.
- ↑ "Breastfeeding:Frequently Asked Questions (FAQs)". U.S. Center for disease control and prevention(CDC). 10 August 2021.
- ↑ Collaborative Group on Hormonal Factors in Breast Cancer (July 2002). "Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease". Lancet. 360 (9328): 187–195. doi:10.1016/S0140-6736(02)09454-0. PMID 12133652. S2CID 25250519.
- ↑ Russo J, Russo IH (August 1980). "Susceptibility of the mammary gland to carcinogenesis. II. Pregnancy interruption as a risk factor in tumor incidence". The American Journal of Pathology. 100 (2): 497–512. PMC 1903536. PMID 6773421.
In contrast, abortion is associated with increased risk of carcinomas of the breast. The explanation for these epidemiologic findings is not known, but the parallelism between the DMBA-induced rat mammary carcinoma model and the human situation is striking. ... Abortion would interrupt this process, leaving in the gland undifferentiated structures like those observed in the rat mammary gland, which could render the gland again susceptible to carcinogenesis.
- ↑ Beral V, Bull D, Doll R, Peto R, Reeves G (March 2004). "Breast cancer and abortion: collaborative reanalysis of data from 53 epidemiological studies, including 83?000 women with breast cancer from 16 countries". Lancet. 363 (9414): 1007–16. doi:10.1016/S0140-6736(04)15835-2. PMID 15051280. S2CID 20751083.
- ↑ American Cancer Society (2005). "Breast Cancer Facts & Figures 2005–2006" (PDF). Archived from the original (PDF) on 13 June 2007. Retrieved 26 April 2007.
- ↑ Wang XS, Armstrong ME, Cairns BJ, Key TJ, Travis RC (March 2011). "Shift work and chronic disease: the epidemiological evidence". Occupational Medicine. 61 (2): 78–89. doi:10.1093/occmed/kqr001. PMC 3045028. PMID 21355031.
- ↑ Marinac CR, Nelson SH, Breen CI, Hartman SJ, Natarajan L, Pierce JP, et al. (August 2016). "Prolonged Nightly Fasting and Breast Cancer Prognosis". JAMA Oncology. 2 (8): 1049–55. doi:10.1001/jamaoncol.2016.0164. PMC 4982776. PMID 27032109.
- ↑ Brody JG, Rudel RA, Michels KB, Moysich KB, Bernstein L, Attfield KR, Gray S (June 2007). "Environmental pollutants, diet, physical activity, body size, and breast cancer: where do we stand in research to identify opportunities for prevention?". Cancer. 109 (12 Suppl): 2627–34. doi:10.1002/cncr.22656. PMID 17503444. S2CID 34880415.
- ↑ Hendrick RE (October 2010). "Radiation doses and cancer risks from breast imaging studies". Radiology. 257 (1): 246–53. doi:10.1148/radiol.10100570. PMID 20736332.
- ↑ 71.0 71.1 71.2 Gage M, Wattendorf D, Henry LR (April 2012). "Translational advances regarding hereditary breast cancer syndromes". Journal of Surgical Oncology. 105 (5): 444–51. doi:10.1002/jso.21856. PMID 22441895. S2CID 3406636.
- ↑ Colditz GA, Kaphingst KA, Hankinson SE, Rosner B (June 2012). "Family history and risk of breast cancer: nurses' health study". Breast Cancer Research and Treatment. 133 (3): 1097–104. doi:10.1007/s10549-012-1985-9. PMC 3387322. PMID 22350789.
- ↑ Collaborative Group on Hormonal Factors in Breast Cancer (October 2001). "Familial breast cancer: collaborative reanalysis of individual data from 52 epidemiological studies including 58,209 women with breast cancer and 101,986 women without the disease". Lancet. 358 (9291): 1389–99. doi:10.1016/S0140-6736(01)06524-2. PMID 11705483. S2CID 24278814.
- ↑ Nelson HD, Zakher B, Cantor A, Fu R, Griffin J, O'Meara ES, et al. (May 2012). "Risk factors for breast cancer for women aged 40 to 49 years: a systematic review and meta-analysis". Annals of Internal Medicine. 156 (9): 635–48. doi:10.7326/0003-4819-156-9-201205010-00006. PMC 3561467. PMID 22547473.
- ↑ 75.0 75.1 Boris Pasche (2010). Cancer Genetics (Cancer Treatment and Research). Berlin: Springer. pp. 19–20. ISBN 978-1-4419-6032-0.
- ↑ Kolata G (23 September 2012). "Genetic Study Finds 4 Distinct Variations of Breast Cancer". The New York Times. Archived from the original on 24 September 2012. Retrieved 23 September 2012.
- ↑ "CDC – What Are the Risk Factors for Breast Cancer?". www.cdc.gov. 14 December 2018.
- ↑ Tian JM, Ran B, Zhang CL, Yan DM, Li XH (January 2018). "Estrogen and progesterone promote breast cancer cell proliferation by inducing cyclin G1 expression". Brazilian Journal of Medical and Biological Research. 51 (3): 1–7. doi:10.1590/1414-431X20175612. PMC 5912097. PMID 29513878. Archived from the original on 2017-05-14. Retrieved 2022-02-15.
- ↑ "Understanding Breast Changes – National Cancer Institute". Archived from the original on 27 May 2010.
- ↑ "Breast Cancer Treatment". National Cancer Institute. January 1980. Archived from the original on 25 April 2015.
- ↑ Afonso N, Bouwman D (August 2008). "Lobular carcinoma in situ". European Journal of Cancer Prevention. 17 (4): 312–6. doi:10.1097/CEJ.0b013e3282f75e5d. PMID 18562954. S2CID 388045.
- ↑ Anothaisintawee T, Wiratkapun C, Lerdsitthichai P, Kasamesup V, Wongwaisayawan S, Srinakarin J, et al. (September 2013). "Risk factors of breast cancer: a systematic review and meta-analysis". Asia-Pacific Journal of Public Health. 25 (5): 368–87. doi:10.1177/1010539513488795. PMID 23709491. S2CID 206616972.
- ↑ Böhm I (June 2011). "Breast cancer in lupus". Breast. 20 (3): 288–90. doi:10.1016/j.breast.2010.12.005. PMID 21237645.
- ↑ Williams, Cecilia; Lin, Chin-Yo (2013-11-05). "Oestrogen receptors in breast cancer: basic mechanisms and clinical implications". ecancermedicalscience. 7: 370. doi:10.3332/ecancer.2013.370. ISSN 1754-6605. PMC 3816846. PMID 24222786.
- ↑ Levin, Ellis R.; Pietras, Richard J. (2008-04-01). "Estrogen receptors outside the nucleus in breast cancer". Breast Cancer Research and Treatment (in Turanci). 108 (3): 351–361. doi:10.1007/s10549-007-9618-4. ISSN 1573-7217. PMID 17592774. S2CID 11394158.
- ↑ Wang, Minghao; Wu, Xiujuan; Chai, Fan; Zhang, Yi; Jiang, Jun (2016-05-17). "Plasma prolactin and breast cancer risk: a meta- analysis". Scientific Reports. 6: 25998. Bibcode:2016NatSR...625998W. doi:10.1038/srep25998. ISSN 2045-2322. PMC 4869065. PMID 27184120.
- ↑ Cavalieri E, Chakravarti D, Guttenplan J, Hart E, Ingle J, Jankowiak R, et al. (August 2006). "Catechol estrogen quinones as initiators of breast and other human cancers: implications for biomarkers of susceptibility and cancer prevention". Biochimica et Biophysica Acta (BBA) - Reviews on Cancer. 1766 (1): 63–78. doi:10.1016/j.bbcan.2006.03.001. PMID 16675129.
- ↑ Filardo EJ (February 2018). "A role for G-protein coupled estrogen receptor (GPER) in estrogen-induced carcinogenesis: Dysregulated glandular homeostasis, survival and metastasis". The Journal of Steroid Biochemistry and Molecular Biology. 176: 38–48. doi:10.1016/j.jsbmb.2017.05.005. PMID 28595943. S2CID 19644829.
- ↑ Filardo EJ (February 2018). "A role for G-protein coupled estrogen receptor (GPER) in estrogen-induced carcinogenesis: Dysregulated glandular homeostasis, survival and metastasis". The Journal of Steroid Biochemistry and Molecular Biology. 176: 38–48. doi:10.1016/j.jsbmb.2017.05.005. PMID 28595943. S2CID 19644829.
- ↑ Haslam SZ, Woodward TL (June 2003). "Host microenvironment in breast cancer development: epithelial-cell-stromal-cell interactions and steroid hormone action in normal and cancerous mammary gland". Breast Cancer Research. 5 (4): 208–15. doi:10.1186/bcr615. PMC 165024. PMID 12817994.
- ↑ Wiseman BS, Werb Z (May 2002). "Stromal effects on mammary gland development and breast cancer". Science. 296 (5570): 1046–9. Bibcode:2002Sci...296.1046W. doi:10.1126/science.1067431. PMC 2788989. PMID 12004111.
- ↑ Jardé T, Perrier S, Vasson MP, Caldefie-Chézet F (January 2011). "Molecular mechanisms of leptin and adiponectin in breast cancer". European Journal of Cancer. 47 (1): 33–43. doi:10.1016/j.ejca.2010.09.005. PMID 20889333.
- ↑ 93.0 93.1 93.2 Cite error: Invalid
<ref>tag; no text was provided for refs namedGot2013 - ↑ Moschetti I, Cinquini M, Lambertini M, Levaggi A, Liberati A (May 2016). "Follow-up strategies for women treated for early breast cancer". The Cochrane Database of Systematic Reviews. 2016 (5): CD001768. doi:10.1002/14651858.cd001768.pub3. PMC 7073405. PMID 27230946.
- ↑ Khan F, Amatya B, Ng L, Demetrios M, Zhang NY, Turner-Stokes L (December 2012). "Multidisciplinary rehabilitation for follow-up of women treated for breast cancer". The Cochrane Database of Systematic Reviews. 12 (3): CD009553. doi:10.1002/14651858.cd009553.pub2. PMC 8078577 Check
|pmc=value (help). PMID 23235677. - ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 11 November 2009. Retrieved 11 November 2009.