Ciwon Daji Na Baka
| Ciwon Daji Na Baka | |
|---|---|
 | |
| Description (en) | |
| Iri |
gastrointestinal system cancer (en) cuta |
| Specialty (en) |
oncology oral and maxillofacial surgery (en) |
| Identifier (en) | |
| ICD-10-CM | C04, C04.0, C04.1 da C04.9 |
| ICD-9-CM | 144.9, 144.1, 144 da 144.0 |
| DiseasesDB | 9288 |
| MedlinePlus | 001035 |
| eMedicine | 001035 |
| Disease Ontology ID | DOID:8618 |
Ciwon daji na baka, wanda aka fi sanin shi da suna ciwon kansar bakin, shi ne ciwon daji na rufin lebe, baki, ko babban makogwaro. [1] A cikin baki, yawanci yana farawa azaman facin fari mara radadi, wanda yayi kauri, yana tasowa jajayen faci, ulcer, kuma yana ci gaba da girma. Lokacin da yake kan lebe, yawanci yakan yi kama da kwankwasa miki wanda baya warkewa, kuma a hankali yana girma.[2] Sauran alamomin na iya hadawa da hadiya mai wahala ko mai radadi, sabbin kullutu ko kumburi a wuya, koh a baki, ko jin kumbura a baki ko lebe. [3]
Abubuwan hadari sun hada da shan taba da barasa .[4][5] Wadanda ke amfani da barasa da taba suna da hadarin kansar baki sau 15 fiye da wadanda ba sa amfani da su.[6] Sauran abubuwan hadari sun hada da kamuwa da cutar HPV, [7] taunar tauna, [8] Da bayyanar rana a kasan lebe.[9] Ciwon daji na baka rukuni ne na kansa da wuyansa. [1] Ana yin ganewar asali ta hanyar biopsy na yankin da ya shafi, sannan bincike tare da CT scan, MRI, PET scan, da jarrabawa don sanin ko ya yadu zuwa sassa masu nisa na jiki.
Ana iya kare cutar kansa ta baka ta hanyar guje wa shan sigari, iyakance amfani da barasa, kariya daga rana akan lebe na kasa, allurar HPV, da nisantar bacin rai. Magungunan da ake amfani da su don ciwon daji na baka na iya hadawa da hadin tiyata (don cire c kwayar cuta da kwayar lymph nodes ), maganin radiation, chemotherapy, ko kuma maganin da aka yi niyya. Nau'o'in jiyya za su dogara da girman, wurare, da yaduwar cutar kansa da aka yi la'akari da lafiyar mutum gaba daya.[1]
A cikin shekara ta 2018, ciwon daji na baki ya faru a duniya a cikin kusan mutane 355,000, kuma ya yi sanadiyar mutuwar 177,000.[10] Tsakanin 1999 da 2015 a Amurka, yawan ciwon daji na baka ya karu da kashi 6% (daga 10.9 zuwa 11.6 cikin 100,000). Mutuwar cutar kansar baki a wannan lokacin ta ragu da kashi 7% (daga 2.7 zuwa 2.5 a cikin 100,000).[11] Ciwon daji na baka yana da jimlar adadin rayuwa na shekara 5 na 65% a cikin Amurka kamar na 2015. [12] Wannan ya bambanta daga 84% idan an gano shi lokacin da aka gano shi, idan aka kwatanta da kashi 66% idan ya yadu zuwa kwayoyin lymph a wuya, da 39% idan ya yada zuwa sassan jiki masu nisa.[12] Yawan tsira kuma ya dogara ne da wurin da cutar ke cikin baki. [13]
Alamomin cutar dajin
[gyara sashe | gyara masomin]

Alamu da alamun ciwon daji na baka sun dogara ne akan wurin da kari yake amma gabadaya suna sirara, marasa daidaituwa, fararen faci a baki. Hakanan zasu iya zama gaurayawan faci na ja da fari (hade-haden facin ja da fari sun fi kamuwa da cutar daji idan aka yi musu rai). Alamar fadakarwa ta al'ada alama ce mai tsayi mai tsayi tare da ulceration, da tsayin iyaka wanda ke da dan radadi. A kan lebe, gyambon ya fi kumbura da bushewa, kuma a cikin pharynx ya fi yawa. Hakanan ana iya hada shi da farar faci, kwancen hakora, gumi na zubar jini, ciwon kunne mai dagewa, jin kumbura a cikin lebe da gabobinsa, ko kumburi.[14]
Lokacin da ciwon daji ya mike zuwa makogwaro, ana iya samun wahalar hadiye, hadiye mai radadi, da kuma sauya murya. [15] Yawanci, raunuka suna da kananan zafi har sai sun girma sannan kuma suna hade da jin zafi. [16] Yayin da raunin ya yadu zuwa ƙwayoyin lymph na wuyansa, rashin jin zafi, taro mai wuya zai ci gaba. Idan ya yada wani wuri a cikin jiki, ciwon daji na gaba daya zai iya tasowa, mafi sau da yawa saboda kasusuwan kashi.[17]
Dalilai
[gyara sashe | gyara masomin]Cutar sankarau ta baka cuta ce ta abubuwan muhalli, mafi girma daga cikinsu ita ce taba. Kamar duk abubuwan muhalli, kimar da ciwon daji zai hadaka ya dogara ne akan adadin, mita da kuma hanyar aikace-aikacen carcinogen (abun da ke haifar da ciwon daji). Baya ga shan taba sigari, sauran cututtukan daji na ciwon daji na baka sun hada da barasa, kwayoyin cuta (musamman HPV 16 da 18), radiation, da hasken UV.
Taba
[gyara sashe | gyara masomin]Taba ita ce mafi girman sanadin ciwon daji na baka da na pharyngeal. Sanannen ciwon daji ne na gabobin jiki da yawa, wanda ke da huldar hadin gwiwa tare da barasa don haifar da ciwon daji na baki da pharynx ta hanyar lalata DNA ta salula kai tsaye. An kiyasta cewa taba yana kara hadarin kansar baki ta hanyar 3.4 -6.8 kuma yana da alhakin kusan kashi 40% na duk ciwon daji na baki.[18]
Barasa
[gyara sashe | gyara masomin]Wasu bincike a Ostiraliya da Brazil da Jamus sun yi nuni da wankin baki mai dauke da barasa kamar yadda kuma ke iya zama sanadi. Da'awar ita ce bayyanar da kullun ga wadannan kurrukan da ke dauke da barasa, ko da idan babu shan taba da sha, yana haifar da hadakar hadakar ciwon daji na baka. Duk da haka, binciken da aka gudanar a 1985,[19] 1995,[20] da 2003[21] ya takaita cewa wanke baki mai dauke da barasa ba ya da alaka da ciwon daji na baki. A cikin takaitaccen Maris na 2009, gungiyar Hakori ta Amurka ta ce "shaidar da ake da ita ba ta goyi bayan alaka tsakanin ciwon daji na baki da kuma shan barasa mai dauke da barasa".[22] Wani bincike na 2008 ya nuna cewa acetaldehyde (wani samfurin barasa) yana cikin ciwon daji na baki,[23][24] amma wannan binciken ya mayar da hankali ga masu cin zarafin barasa kuma bai yi magana game da wanke baki ba.
Human papillomavirus
[gyara sashe | gyara masomin]Kamuwa da cutar papillomavirus (HPV), musamman nau'in 16 (akwai nau'ikan nau'ikan sama da 180), sanannen hadarin hadari ne kuma sanadin cutar kansa mai zaman kanta ga kansar baka. [25] Wani yanki mai girma cikin sauri na wadanda aka gano baya gabatar da kwararrun alkaluma na tarihi. A tarihi wanda ya kasance mutane sama da 50, baƙar fata fiye da farare 2 zuwa 1, maza akan mata 3 zuwa 1, da 75% na lokutan mutanen da suka yi amfani da kayan sigari ko masu yawan shan barasa. Wannan sabuwar kabila mai girma da sauri tsakanin shekaru 30 zuwa 50,[26] galibi marasa shan taba ne, farare, kuma maza sun fi mata yawa. Bincike na baya-bayan nan daga labaran mujallolin da aka bita da yawa ya nuna cewa HPV16 shine babban abin hadari a cikin wannan sabon yawan mutanen da ke fama da cutar kansa ta baki. HPV16 (tare da HPV18) kwayar cuta iri daya ce da ke da alhakin mafi yawan duk cututtukan daji na mahaifa kuma ita ce mafi yawan kamuwa da kamuwa da jima'i a Amurka. Ciwon daji na baka a cikin wannan rukuni yana kula da tonsil da ginshiƙan tonsillar, tushe na harshe, da kuma oropharynx. Bayanai na baya-bayan nan sun nuna cewa mutanen da suka kamu da cutar daga wannan dalili na musamman suna da fa'ida mai mahimmanci na rayuwa, [27] yayin da cutar ta fi dacewa da jiyya na radiation fiye da yadda taba ke haifar da cuta.
Kwayar goro
[gyara sashe | gyara masomin]
Cin dusar kankara, paan da Areca an san su zama hadari mai karfi don hadaka ciwon daji na baki koda kuwa babu taba. Yana kara yawan ciwon daji na baka sau 2.1, ta hanyar nau'ikan kwayoyin halitta da abubuwan da ke da alaka ta hanyar hangula na gida na kwayoyin mucous membrane, musamman daga gwaya da lemun tsami. A Indiya inda irin wadannan ayyuka suka zama ruwan dare, ciwon daji na baka yana wakiltar kusan kashi 40% na duk cututtukan daji, idan aka kwatanta da kawai 4% a Burtaniya.
Dashen kwayar halitta
[gyara sashe | gyara masomin]Mutane bayan dashen kwayar cutar hematopoietic (HSCT) suna cikin hadari mafi girma ga carcinoma na bakin squamous cell. Bayan-HSCT ciwon daji na baka na iya samun karin hali mai muni tare da rashin fahimta, idan aka kwatanta da ciwon daji na baki a cikin mutanen da ba a bi da su tare da HSCT ba. Ya kamata wannan tasirin ya kasance ne saboda ci gaba da danne garkuwar jiki na tsawon rayuwa da kuma na yau da kullun na baka -da-masu cuta.[28]
Launuka masu tasowa
[gyara sashe | gyara masomin]
An bayyana raunin da ba a taba gani ba (ko wanda ya rigaya ya rigaya) a matsayin "nama mara kyau, mai canza yanayin halitta wanda ke da hadari fiye da al'ada na canji mara kyau." Akwai nau'o'in nau'ikan raunuka daban-daban wadanda ke faruwa a cikin baki. Wasu cututtukan daji na baka suna farawa azaman facin fari ( leukoplakia ), jajayen faci ( erythroplakia ) ko gauraye ja da fari faci (erythroleukoplakia ko “speckled leukoplakia”). Sauran cututtuka na yau da kullun sun hada da fibrosis submucous na baka da actinic cheilitis .[29] A cikin nahiyoyin Indiya, fibrosis na baka na baka ya zama ruwan dare saboda cin goro. Wannan yanayin yana da alaƙa da iyakancewar bube baki da zafi mai zafi akan cin abinci mai yaji. Wannan ciwo ne mai ci gaba wanda bude baki ya zama mai iyakancewa, kuma daga baya ko da cin abinci na yau da kullum yana da wahala.
Pathophysiology
[gyara sashe | gyara masomin]Kwayar Cuta mara tsari. Tantanin halitta guda daya yana canzawa zuwa clone wanda ya kunshi sel dan mata da yawa tare da tarin sauye-sauyen kwayoyin halittar da ake kira oncogenes. Abin da ke nuna mummunan kwayar cuta a kan mara lafiya shine ikonsa na metastasize. Wannan ikon ya kasance mai zaman kansa daga girman ko darajar kwayar cuta (sau da yawa kamar jinkirin girma ciwon daji kamar adenoid cystic carcinoma na iya metastasis a ko'ina). Ba wai kawai saurin girma ne ke nuna ciwon daji ba, amma ikon su na boye enzymes, abubuwan angiogeneic, abubuwan mamayewa, abubuwan haɓaka da sauran abubuwan da ke ba da damar yaduwa.
Bincike
[gyara sashe | gyara masomin]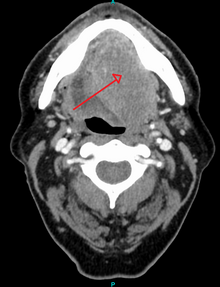

An kammala gano ciwon daji na baka don (1) ganewar asali, (2) tsarawa, da (3) shirin magani. Cikakken tarihin tarihi, kuma an fara kammala gwajin asibiti, sannan an yanke wani yanki na nama daga raunin da ake tuhuma don ganewar asali. Ana iya yin wannan tare da biopsy na fatar jiki, biopsy na punch, lafiya ko ainihin kwayar allura . A cikin wannan hanya, likitan fida ya yanke duka, ko guntun nama, don a duba shi a karkashin na'urar gani da ido ta wurin likitan ilimin cututtuka.[30] Ba a yi la'akarin ɓangarorin goge goge daidai don gano ciwon daji na baki.[31]
Tare da biopsy na farko, likitan ilimin cututtuka zai samar da ganewar kwayar cuta (misali squamous cell carcinoma ), kuma ya rarraba tsarin tantanin halitta. Za su iya kara karin bayani wadanda za a iya amfani da su a cikin tsarawa, da tsarin kulawa, irin su mitotic rate, zurfin mamayewa, da kuma matsayin HPV na nama.
Bayan an tabbatar da nama yana da kansa, za a kammala wasu gwaje-gwaje zuwa:
- mafi kyawun tantance girman raunin ( CT scan, MRI ko PET scan tare da 18F-fluorodeoxyglucose (FDG)), : 143
- nemo wasu cututtuka na ciwon daji a cikin sashin jiki na sama (wanda zai iya haɗawa da endoscopy na kogon hanci / pharynx, larynx, bronchus, da esophagus da ake kira panendoscopy ko quadoscopy ),
- yaduwa zuwa nodes na lymph ( CT scan ) ko
- yaduwa zuwa wasu sassan jiki ( X-ray na kirji, maganin nukiliya ).
Sauran, karin gwaje-gwaje masu cin zarafi, ana iya kuma iya kammala su kamar kyakkyawan fata na allura, biopsy na nodes na lymph, da biopsy node na sentinel. Lokacin da ciwon daji ya yada zuwa kananan kwayoyin lymph, ainihin wurin su, girman su, da yadawa fiye da capsule (na lymph nodes) yana bukatar kayyade, saboda kowannensu na iya yin tasiri mai mahimmanci akan jiyya da tsinkaye. Wwnanan bambance-bambance a cikin nau'in kwayar kwayar ƙwayar ƙwayar cuta, na iya samun tasiri mai mahimmanci akan jiyya da tsinkaye. Ana iya ba da shawarar Panendoscopy, saboda kyallen takarda na gabaɗayan sashin iska na sama gaba ɗaya suna shafar carcinogens iri ɗaya, don haka sauran cututtukan daji na farko sun zama ruwan dare gama gari.[32][33]
Daga waɗannan binciken gama-gari, wadanda aka yi la’akari da lafiya da sha’awar mutum, gungiyar ciwon daji ta hadaka shirin jiyya. Tunda yawancin ciwon daji na baka suna buƙatar cirewar tiyata, za a kammala saiti na biyu na gwaje-gwaje na histopathologic akan duk wani ƙari da aka cire don tantance hasashen, bukatar karin tiyata, chemotherapy, radiation, immunotherapy, ko wasu tsoma baki.
Rabewa
[gyara sashe | gyara masomin]Ciwon daji na baka rukuni ne na kansa da wuyansa wanda ya hada da na oropharynx, larynx, kogon hanci da sinuses na paranasal, glandan salivary, da glandar thyroid . Melanoma na baka, yayin da ake la'akari da wani bangare na kansa da wuyansa daban. Sauran cututtukan daji na iya faruwa a cikin baki (kamar ciwon daji na kashi, lymphoma, ko ciwon daji na metastatic daga wurare masu nisa) amma kuma ana la'akari da su daban da ciwon daji na baka.
Tsayawa
[gyara sashe | gyara masomin]Matsayin ciwon daji na baka shine kimanta girman yaduwar cutar kansa daga asalinsa.[34] Yana daya daga cikin abubuwan da suka shafi duka tsinkaye da yuwuwar maganin ciwon daji na baka.
Kimar ciwon daji na squamous cell carcinoma na baki da pharynx staging yana amfani da tsarin TNM (tumor, node, metastasis). Wannan ya dogara ne akan girman kwayar kwayar cuta ta farko, shigar kumburin lymph, da metastasis mai nisa.[35]
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Kimar TMN yana ba da damar a rarraba mutumin zuwa gungiyar tsinkaya;
TMN evaluation allows the person to be classified into a prognostic staging group;[36]
| When T is... | And N is... | And M is... | Then the stage group is... |
|---|---|---|---|
| Tis | N0 | M0 | 0 |
| T1 | N0 | M0 | I |
| T2 | N0 | M0 | II |
| T3 | N0 | M0 | III |
| T1,T2,T3 | N1 | M0 | III |
| T4a | N0,N1 | M0 | IVA |
| T1,T2,T3,T4a | N2 | M0 | IVA |
| Any T | N3 | M0 | IVB |
| T4b | Any N | M0 | IVB |
| Any T | Any N | M1 | IVC |
Nunawa
[gyara sashe | gyara masomin]Miyagun Ayyukan Tsoratarwar Amurka (Uspstf) a cikin 2013 da aka bayyana hujjoji ba su da isasshen inganci da cutar kansa ba tare da alamomi ta hanyar ba da kulawa. [37] Cibiyar Nazarin Likitocin Iyali ta Amurka ta zo ga irin wannan matsaya yayin da gungiyar Ciwon daji ta Amurka ta ba da shawarar cewa manya sama da shekaru 20 wadanda ke yin gwajin lafiya na lokaci-lokaci yakamata a bincika kogon baki don ciwon daji. gungiyar Haƙori ta Amurka ta ba da shawarar cewa masu ba da sabis su kasance a fadake don alamun ciwon daji yayin gwaje-gwaje na yau da kullun.
Akwai nau'ikan na'urorin dubawa iri-iri irin su toluidine blue, brush biopsy, ko hoto mai haske, duk da haka, babu wata shaida cewa yin amfani da waɗannan na'urori na yau da kullun a aikin haƙori na gaba daya yana taimakawa. [38] Hadarin da za a yi amfani da su na yin amfani da na'urorin tantancewa sun hadaa da abubuwan da ba su dace ba, gwajin kwayoyin cuta marasa amfani, da nauyin kudi. Kididdigar kananan kwayoyin cuta na iya taimakawa a farkon ganewar cututtuka na pre-malignant da m raunuka, don haka inganta rayuwa da kuma rage cututtuka da ke hade da magani.
Haka kuma an yi bincike da ke nuna yuwuwar yin amfani da ilimin sinadarai na baka a matsayin gwajin cutar kansar baki maimakon dabarun biopsy na gargajiya. A cikin cytology na baka, ana amfani da goga don daukar wasu sel daga raunin da ake zargi kuma ana aika su zuwa dakin gwaje-gwaje don dubawa. [39] Wannan na iya zama kasa da barna da zafi fiye da kwayar kwayar cuta ga mai hakuri, duk da haka, akwai bukatar karin bincike kafin a iya daukar cytology na baka azaman kayan aikin tantancewa na yau da kullun idan aka kwatanta da biopsies.
Gudanarwa
[gyara sashe | gyara masomin]
Ciwon daji na baka (squamous cell carcinoma) yawanci ana yi masa tiyata ne kawai, ko kuma a hade tare da jiyya, gami da radiation, tare da ko ba tare da chemotherapy ba. (pp602)Tare da kananan raunuka (T1), tiyata ko radiation suna da nau'o'in kulawa iri daya, don haka yanke shawara game da abin da za a yi amfani da shi ya dogara ne akan sakamakon aiki, da kuma rikitarwa.
Tiyata
[gyara sashe | gyara masomin]A mafi yawan cibiyoyi, kawar da ciwon daji na squamous cell daga kogon baka da wuya ana samun su da farko ta hanyar tiyata. Wannan kuma yana ba da damar cikakken nazarin nama don halaye na tarihi, kamar zurfin, da kuma yada zuwa nodes na lymph wadanda zasu bukaci radiation ko chemotherapy. Don kananan raunuka (T1-2), samun dama ga kogon baka yana ta bakin. Lokacin da raunin ya fi girma, ya haɗa da kashi na maxilla ko mandible, ko samun damar shiga ya iyakance saboda buɗe baki, babba ko kananan lebe ya rabu, kuma kunci ya ja baya don ba da damar shiga bakin. Lokacin da dari ya kunshi kashin muƙamuƙi, ko lokacin tiyata ko radiation zai haifar da iyakacin buɗe baki, ana kuma cire ɓangaren kashi tare da kari.
Gudanar da wuyansa
[gyara sashe | gyara masomin]
Yaduwar ciwon daji daga kogon baka zuwa ga nodes na lymph na wuyansa yana da tasiri mai mahimmanci akan rayuwa . Tsakanin 60-70% na mutanen da ke fama da ciwon daji na baki ba za su sami kumburin ƙwayar lymph na wuyansa a asibiti ba, amma 20-30% na mutanen (ko har zuwa 20% na duk wadanda abin ya shafa) za su sami ciwon daji wanda ba za a iya gano shi ba. Kwayoyin lymph na wuyansa (wanda ake kira cutar occult).
Gudanar da wuyansa yana da mahimmanci, tun lokacin da aka yada shi yana rage yiwuwar rayuwa ta hanyar 50%.[39] Idan akwai shaidar shigar kumburin lymph na wuyansa, a lokacin lokacin ganewar asali, to, ana yin gyaran gyare-gyaren wuyan wuyansa gabaɗaya. Inda ƙwayoyin lymph na wuyansa ba su da shaidar shiga asibiti, amma raunin kogin baki yana da haɗari ga yaduwa (misali. T2 ko sama da raunuka), sa'an nan kuma za a iya kammala rarraba wuyan wuyansa na kwayoyin lymph sama da matakin tsokar omohyoid . Lokacin da cutar idan aka samu a cikin nodes bayan cirewa (amma ba a gani a asibiti ba) yawan maimaitawa shine 10-24%. Idan an ƙara radiation bayan tiyata, ƙimar gazawar ita ce 0-15%. Lokacin da aka gano ƙwayoyin lymph a asibiti a lokacin lokacin ganewar asali, kuma an ƙara radiation bayan tiyata, kula da cututtuka shine> 80%.[40]
Radiotherapy da chemotherapy
[gyara sashe | gyara masomin]
Chemotherapy da radiotherapy yawanci ana amfani da su, azaman hadin kai ga tiyata, don sarrafa ciwon daji na baka wanda ya fi mataki na 1, ko kuma ya yadu zuwa ko dai kwayoyin lymph na yanki ko wasu sassan jiki. Radiotherapy kadai za a iya amfani da shi a maimakon tiyata, don wananan raunuka, amma ana amfani dashi a matsayin hadin gwiwa lokacin da raunuka suka yi girma, ba za a iya cire su gaba daya ba, ko kuma sun yada zuwa kwayoyin lymph na wuyansa. Chemotherapy yana da amfani a cikin ciwon daji na baka idan aka yi amfani da shi tare da wasu hanyoyin magani kamar radiation far amma ba a yi amfani da shi kadai a matsayin monotherapy. Lokacin da magani ba shi da wuya, ana iya amfani da shi don tsawaita rayuwa kuma ana iya la'akari da shi azaman magani amma ba kula da warkewa ba. [41]
Monoclonal antibody far (tare da jamiái irin su cetuximab ) an nuna cewa yana da tasiri a cikin maganin ciwon daji na squamous cell da wuyansa, kuma yana iya samun tasiri mai yawa a cikin kula da wannan yanayin a nan gaba idan aka yi amfani da shi tare da sauran maganin da aka kafa. modalities, ko da yake ba maye gurbin chemotherapy a kai da kuma wuyansa cancers. [42] Hakazalika, hanyoyin da aka yi niyya ta kwayoyin cuta da magungunan rigakafi na iya zama tasiri don maganin ciwon daji na baka da na oropharyngeal. Kara abubuwan hadakar hadakar epidermal receptor monoclonal antibody (EGFR mAb) zuwa daidaitaccen magani na iya hadaka rayuwa, kiyaye ciwon daji iyakance ga wannan yanki na jiki kuma yana iya rage bayyanar cutar kansa.
Gyaran jiki
[gyara sashe | gyara masomin]Bayan jiyya, gyara na iya zama dole don inganta motsi, taunawa, hadiye, da magana. Masana magana da harshe na iya shiga cikin wannan matakin. Maganin ciwon daji na baki yawanci zai kasance ta gungiyar kwararrun , tare da kwararrun jiyya daga yanayin radiation, tiyata, chemotherapy, abinci mai gina jiki, likitan hakori, har ma da ilimin halin dan adam duk mai yuwuwar hadawa da ganewar asali, jiyya, gyarawa, da kulawa. Saboda wurin ciwon daji na baka, ana iya samun lokacin da mutum ya bukaci tracheotomy da bututun ciyarwa .
Manazarta
[gyara sashe | gyara masomin]- ↑ 1.0 1.1 1.2 Edge SB, et al. (American Joint Committee on Cancer) (2010). AJCC cancer staging manual (7th ed.). New York: Springer. ISBN 9780387884400. OCLC 316431417.
- ↑ Marx RE, Stern D (2003). Oral and maxillofacial pathology : a rationale for diagnosis and treatment. Stern, Diane. Chicago: Quintessence Pub. Co. ISBN 978-0867153903. OCLC 49566229.
- ↑ "Head and Neck Cancers". CDC. 2019-01-17. Retrieved 2019-03-10.
- ↑ Gandini S, Botteri E, Iodice S, Boniol M, Lowenfels AB, Maisonneuve P, Boyle P (January 2008). "Tobacco smoking and cancer: a meta-analysis". International Journal of Cancer. 122 (1): 155–64. doi:10.1002/ijc.23033. PMID 17893872. S2CID 27018547.
- ↑ Goldstein BY, Chang SC, Hashibe M, La Vecchia C, Zhang ZF (November 2010). "Alcohol consumption and cancers of the oral cavity and pharynx from 1988 to 2009: An update". European Journal of Cancer Prevention. 19 (6): 431–65. doi:10.1097/CEJ.0b013e32833d936d. PMC 2954597. PMID 20679896.
- ↑ admin. "The Tobacco Connection". The Oral Cancer Foundation. Retrieved 2019-03-10.
- ↑ Kreimer AR, Clifford GM, Boyle P, Franceschi S (February 2005). "Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review". Cancer Epidemiology, Biomarkers & Prevention. 14 (2): 467–75. doi:10.1158/1055-9965.EPI-04-0551. PMID 15734974.
- ↑ Goldenberg D, Lee J, Koch WM, Kim MM, Trink B, Sidransky D, Moon CS (December 2004). "Habitual risk factors for head and neck cancer". Otolaryngology–Head and Neck Surgery. 131 (6): 986–93. doi:10.1016/j.otohns.2004.02.035. PMID 15577802. S2CID 34356067.
- ↑ Kerawala C, Roques T, Jeannon JP, Bisase B (May 2016). "Oral cavity and lip cancer: United Kingdom National Multidisciplinary Guidelines". The Journal of Laryngology and Otology. 130 (S2): S83–S89. doi:10.1017/S0022215116000499. PMC 4873943. PMID 27841120.
- ↑ "Cancer today". gco.iarc.fr (in Turanci). Retrieved 9 June 2019.
- ↑ "Cancer today". gco.iarc.fr (in Turanci). Retrieved 9 June 2019.
- ↑ 12.0 12.1 "Cancer Stat Facts: Oral Cavity and Pharynx Cancer". NCI. Retrieved 27 June 2019.
- ↑ "Survival Rates for Oral Cavity and Oropharyngeal Cancer". www.cancer.org. Retrieved 2019-03-10.
- ↑ Ravikiran Ongole, Praveen B N, ed. (2014). Textbook of Oral Medicine, Oral Diagnosis and Oral Radiology. Elsevier India. p. 387. ISBN 978-8131230916.
- ↑ "Symptoms of oral cancer—Canadian Cancer Society". www.cancer.ca. Retrieved 2019-03-10.
- ↑ Markopoulos AK (2012-08-10). "Current aspects on oral squamous cell carcinoma". The Open Dentistry Journal. 6 (1): 126–30. doi:10.2174/1874210601206010126. PMC 3428647. PMID 22930665.
- ↑ Markopoulos AK (2012-08-10). "Current aspects on oral squamous cell carcinoma". The Open Dentistry Journal. 6 (1): 126–30. doi:10.2174/1874210601206010126. PMC 3428647. PMID 22930665.
- ↑ Cancer Care Ontario (2014). "Cancer Risk Factors in Ontario: Tobacco" (PDF). www.cancercare.on.ca.
- ↑ Mashberg A, Barsa P, Grossman ML (May 1985). "A study of the relationship between mouthwash use and oral and pharyngeal cancer". Journal of the American Dental Association. 110 (5): 731–4. doi:10.14219/jada.archive.1985.0422. PMID 3859544.
- ↑ Elmore JG, Horwitz RI (September 1995). "Oral cancer and mouthwash use: evaluation of the epidemiologic evidence". Otolaryngology–Head and Neck Surgery. 113 (3): 253–61. doi:10.1016/S0194-5998(95)70114-1. PMID 7675486. S2CID 20725009.
- ↑ Cole P, Rodu B, Mathisen A (August 2003). "Alcohol-containing mouthwash and oropharyngeal cancer: a review of the epidemiology". Journal of the American Dental Association. 134 (8): 1079–87. doi:10.14219/jada.archive.2003.0322. PMID 12956348.
- ↑ Science brief on alcohol-containing mouthrinses and oral cancer, Archived ga Maris, 19, 2012 at the Wayback Machine American Dental Association, March 2009
- ↑ Warnakulasuriya S, Parkkila S, Nagao T, Preedy VR, Pasanen M, Koivisto H, Niemelä O (March 2008). "Demonstration of ethanol-induced protein adducts in oral leukoplakia (pre-cancer) and cancer". Journal of Oral Pathology & Medicine. 37 (3): 157–65. doi:10.1111/j.1600-0714.2007.00605.x. PMID 18251940.
- ↑ Alcohol and oral cancer research breakthrough Archived Mayu 2, 2009, at the Wayback Machine
- ↑ Gillison ML, Chaturvedi AK, Anderson WF, Fakhry C (October 2015). "Epidemiology of Human Papillomavirus-Positive Head and Neck Squamous Cell Carcinoma". Journal of Clinical Oncology. 33 (29): 3235–42. doi:10.1200/JCO.2015.61.6995. PMC 4979086. PMID 26351338.
- ↑ Martín-Hernán F, Sánchez-Hernández JG, Cano J, Campo J, del Romero J (May 2013). "Oral cancer, HPV infection and evidence of sexual transmission". Medicina Oral, Patologia Oral y Cirugia Bucal. 18 (3): e439-44. doi:10.4317/medoral.18419. PMC 3668870. PMID 23524417.
- ↑ "HPV-Positive Tumor Status Indicates Better Survival in Patients with Oropharyngeal Cancer—MD Anderson Cancer Center". www.mdanderson.org.
- ↑ Elad S, Zadik Y, Zeevi I, Miyazaki A, de Figueiredo MA, Or R (December 2010). "Oral cancer in patients after hematopoietic stem-cell transplantation: long-term follow-up suggests an increased risk for recurrence". Transplantation. 90 (11): 1243–4. doi:10.1097/TP.0b013e3181f9caaa. PMID 21119507.
- ↑ Neville BW, Damm DD, Allen CM, Bouquot JE (2002). Oral & maxillofacial pathology (2nd ed.). Philadelphia: W.B. Saunders. pp. 337, 345, 349, 353. ISBN 978-0721690032.
- ↑ Gullane P (2016). Sataloff's Comprehensive Textbook of Otolaryngology: Head and Neck Surgery: Head and Neck Surgery. 5. New Delhi, India: The Health Sciences Publisher. p. 600. ISBN 978-93-5152-458-8.
- ↑ H Alsarraf A, Kujan O, Farah CS (February 2018). "The utility of oral brush cytology in the early detection of oral cancer and oral potentially malignant disorders: A systematic review". Journal of Oral Pathology & Medicine. 47 (2): 104–116. doi:10.1111/jop.12660. PMID 29130527. S2CID 46832488.
- ↑ Levine B, Nielsen EW (August 1992). "The justifications and controversies of panendoscopy--a review". Ear, Nose, & Throat Journal. 71 (8): 335–40, 343. doi:10.1177/014556139207100802. PMID 1396181. S2CID 25921527.
- ↑ Clayburgh DR, Brickman D (January 2017). "Is esophagoscopy necessary during panendoscopy?". The Laryngoscope. 127 (1): 2–3. doi:10.1002/lary.25532. PMID 27774605. S2CID 19124543.
- ↑ Connolly JL, Goldsmith JD, Wang HH, et al. (2010). "37: Principles of Cancer Pathology". Holland-Frei Cancer Medicine (8th ed.). People's Medical Publishing House. ISBN 978-1-60795-014-1.
- ↑ "AJCC Cancer Staging Form Supplement. AJCC Cancer Staging Manual, eighth Edition Update 05 June 2018" (PDF). www.cancerstaging.org. 5 June 2018. Retrieved 7 April 2019.
- ↑ 36.0 36.1 Cite error: Invalid
<ref>tag; no text was provided for refs namedAJCC8th3 - ↑ "Final Recommendation Statement: Oral Cancer: Screening—US Preventive Services Task Force". www.uspreventiveservicestaskforce.org. November 2013. Retrieved 23 November 2017.
- ↑ Brocklehurst P, Kujan O, O'Malley LA, Ogden G, Shepherd S, Glenny AM (November 2013). "Screening programmes for the early detection and prevention of oral cancer". The Cochrane Database of Systematic Reviews. 2021 (11): CD004150. doi:10.1002/14651858.CD004150.pub4. PMC 8078625 Check
|pmc=value (help). PMID 24254989. - ↑ 39.0 39.1 Walsh, Tanya; Macey, Richard; Kerr, Alexander R.; Lingen, Mark W.; Ogden, Graham R.; Warnakulasuriya, Saman (2021-07-20). "Diagnostic tests for oral cancer and potentially malignant disorders in patients presenting with clinically evident lesions". The Cochrane Database of Systematic Reviews. 2021 (7): CD010276. doi:10.1002/14651858.CD010276.pub3. ISSN 1469-493X. PMC 8407012 Check
|pmc=value (help). PMID 34282854 Check|pmid=value (help).CS1 maint: PMC embargo expired (link) - ↑ Zelefsky MJ, Harrison LB, Fass DE, Armstrong JG, Shah JP, Strong EW (January 1993). "Postoperative radiation therapy for squamous cell carcinomas of the oral cavity and oropharynx: impact of therapy on patients with positive surgical margins". International Journal of Radiation Oncology, Biology, Physics. 25 (1): 17–21. doi:10.1016/0360-3016(93)90139-m. PMID 8416876.
- ↑ Petrelli F, Coinu A, Riboldi V, Borgonovo K, Ghilardi M, Cabiddu M, et al. (November 2014). "Concomitant platinum-based chemotherapy or cetuximab with radiotherapy for locally advanced head and neck cancer: a systematic review and meta-analysis of published studies". Oral Oncology. 50 (11): 1041–8. doi:10.1016/j.oraloncology.2014.08.005. PMID 25176576.
- ↑ Chan KK, Glenny AM, Weldon JC, Furness S, Worthington HV, Wakeford H (December 2015). "Interventions for the treatment of oral and oropharyngeal cancers: targeted therapy and immunotherapy". The Cochrane Database of Systematic Reviews (12): CD010341. doi:10.1002/14651858.CD010341.pub2. PMID 26625332.
