Ciwon daji na mahaifa
| Ciwon daji na mahaifa | |
|---|---|
 | |
| Description (en) | |
| Iri |
Ciwon daji na Mahaifa, cervix disease (en) cuta |
| Specialty (en) | oncology |
| Genetic association (en) |
ZNF804B (en) |
| Identifier (en) | |
| ICD-10-CM | C53.9 da C53 |
| ICD-9-CM | 180.9 da 180 |
| OMIM | 603956 |
| DiseasesDB | 2278 |
| MedlinePlus | 000893 |
| eMedicine | 000893 |
| Disease Ontology ID | DOID:4362 |
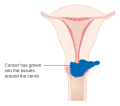
Ciwon daji na mahaifa ciwon daji ne da ke fitowa daga mahaifar mahaifa.[1] Yana faruwa ne saboda rashin haɓakar ƙwayoyin sel waɗanda ke da ikon mamayewa ko yada zuwa wasu sassan jiki.[2] Tun da wuri, yawanci ba a ganin alamun.[1] Daga baya alamomin na iya haɗawa da zubar da jini na al'ada na al'ada, ciwon ƙwai ko zafi yayin jima'i.[1] Yayin da zubar jini bayan jima'i bazai zama mai tsanani ba, yana iya nuna kasancewar ciwon daji na mahaifa.[3]
Cutar papillomavirus (HPV) tana haifar da fiye da kashi 90% na lokuta;[4][5] yawancin mutanen da suka kamu da cutar HPV, duk da haka, ba sa kamuwa da kansar mahaifa.[6][7] Sauran abubuwan da ke haifar da haɗari sun haɗa da shan taba, raunin garkuwar jiki, maganin hana haihuwa, fara jima'i tun yana ƙarami, da yawan abokan jima'i, to amma waɗannan ba su da mahimmanci.[1][8] Ciwon daji na mahaifa yawanci yana tasowa ne daga canje-canjen da ke faruwa a cikin shekaru 10 zuwa 20.[6] Kusan kashi 90 cikin 100 na cututtukan sankarar mahaifa su ne squamous cell carcinomas, 10% adenocarcinoma ne, kuma ƙaramin adadin wasu nau'ikan ne.[8] Ganowa yawanci ta hanyar duban mahaifa sai kuma biopsy.[1] Ana yin hoton likita don sanin ko ciwon daji ya yadu ko a'a.
Alurar rigakafin HPV suna kare kariya daga nau'ikan haɗari biyu zuwa bakwai na wannan dangin ƙwayoyin cuta kuma suna iya hana kusan kashi 90% na kansar mahaifa.[9][10][11] Kamar yadda har yanzu akwai haɗarin cutar kansa, jagororin suna ba da shawarar ci gaba da kuma gwajin Pap na yau da kullun.[9] Sauran hanyoyin rigakafin sun haɗa da samun ƴan ƙalilan ko rashin yin jima'i da amfani da kwaroron roba.[12] Yin gwajin cutar kansar mahaifa ta hanyar amfani da gwajin Pap ko acetic acid na iya gano sauye-sauyen da suka riga ya faru, wanda idan aka bi da su, zai iya hana ci gaban cutar kansa.[13] Jiyya na iya ƙunsar wasu haɗin tiyata, chemotherapy, da maganin radiation.[1] Yawan rayuwa na shekaru biyar a Amurka shine 68%.[14] Sakamako, duk da haka, sun dogara sosai kan yadda ake gano ciwon daji da wuri.[8]
A duk duniya, cutar kansar mahaifa ita ce ta huɗu mafi yawan sanadin cutar kansa da kuma na huɗu mafi yawan sanadin mutuwar mata daga cutar kansa.[6] A cikin 2012, an yi kiyasin mutane 528,000 na cutar sankara ta mahaifa, tare da mutuwar 266,000.[6] Wannan shine kusan kashi 8% na jimillar cutar da jimillar mace-mace daga cutar kansa.[15] Kimanin kashi 70% na ciwon sankarar mahaifa da kashi 90% na mace-mace na faruwa a kasashe masu tasowa.[6][16] A cikin kasashe masu karamin karfi, yana daya daga cikin abubuwan da ke haifar da mutuwar ciwon daji.[13] A cikin kasashen da suka ci gaba, yawan amfani da shirye-shiryen tantance mahaifa ya ragu matuka da gaske wajen kamuwa da cutar kansar mahaifa.[17] A cikin binciken likita, sanannen layin tantanin halitta da ba a mutu ba, wanda aka sani da HeLa, an samo shi daga ƙwayoyin kansar mahaifa na wata mace mai suna Henrietta Lacks.[18]
Alamomi
[gyara sashe | gyara masomin]Matakan farko na kansar mahaifa na iya zama gaba ɗaya mara alamun alamun . Zubar da jini na farji, saduwa da jini (wani nau'i na yau da kullum shine zubar jini bayan jima'i), ko (da wuya) yawan ƙwayar farji na iya nuna kasancewar rashin lafiya. Har ila yau, matsakaitan zafi a lokacin jima'i da zubar da jini a cikin farji alamun ciwon daji ne na mahaifa.[19] A cikin cututtukan da ke ci gaba, metastases na iya kasancewa a cikin ciki, huhu, ko wasu wurare.[20]
Alamomin ciwon daji na mahaifa na iya haɗawa da: asarar ci, asarar nauyi, gajiya, ciwon pelvic, ciwon baya, ciwon ƙafa, zubar jinin ta farji bayan Jima'i,kumbura kafafu, zubar da jini mai yawa, raunin kashi, da (da wuya) zubar fitsari ko najasa daga farji.[21] Zubar da jini bayan shafewa ko bayan jarrabawar mahaifa alama ce ta kowa ta kansar mahaifa. [22]
Dalilai
[gyara sashe | gyara masomin]

Kamuwa da wasu nau'ikan HPV shine babban haɗarin cutar kansar mahaifa, sannan shan taba.[23] Kamuwa da cutar kanjamau kuma abu ne mai haɗari. Ba a san duk abubuwan da ke haifar da kansar mahaifa ba, duk da haka, kuma an sami wasu abubuwan da ke taimakawa. [24][25]
Human papillomavirus
[gyara sashe | gyara masomin]Nau'in HPV na 16 da 18 sune ke haifar da kashi 75% na cutar sankarar mahaifa a duniya, yayin da 31 da 45 ke haifar da wani 10%. [26]
Matan da suka yi jima'i da mazan da ke da sauran abokan jima'i ko matan da ke da yawancin abokan jima'i suna da haɗari mafi girma. [27][28]
Daga cikin nau'ikan 150-200 na HPV da aka sani,[29][30] 15 ana rarraba su azaman nau'ikan haɗari (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68). . da CP6108).[31]
Hakkokin na Genet, wanda shine nau'in ƙwayoyin cuta na ƙwayoyin sel, suma sun haifar da juzu'in HPV daban-daban na HPV. Koyaya, waɗannan serotypes yawanci ba su da alaƙa da kansar mahaifa. Samun nau'i-nau'i masu yawa a lokaci guda ya zama ruwan dare, ciki har da wadanda ke haifar da ciwon daji na mahaifa tare da wadanda ke haifar da warts. Kamuwa da cuta tare da HPV gabaɗaya an yi imanin ana buƙata don kansar mahaifa ya faru. [32]
Shan taba
[gyara sashe | gyara masomin]Shan taba sigari, duka masu aiki da kuma m, yana ƙara haɗarin kansar mahaifa. Daga cikin matan da suka kamu da cutar ta HPV, masu shan taba da na yanzu da na baya suna da kusan sau biyu zuwa uku na yawan kamuwa da cutar sankara. Hakanan shan taba sigari yana da alaƙa da haɓakar haɗari, amma a ɗan ƙarami. [33]
An kuma danganta shan taba da cutar sankarar mahaifa.[34][35] Shan taba na iya ƙara haɗari ga mata ta hanyoyi daban-daban, wanda zai iya kasancewa ta hanyar kai tsaye da kuma kai tsaye hanyoyin haifar da ciwon daji na mahaifa. [36] Hanyar kai tsaye ta kamuwa da wannan cutar kansa ita ce mai shan taba yana da babbar dama ta intraepithelial neoplasia (CIN3) na mahaifa yana faruwa, wanda ke da yuwuwar haifar da kansar mahaifa. Lokacin da raunin CIN3 ya haifar da ciwon daji, yawancin su suna samun taimakon kwayar cutar HPV, amma ba haka ba ne kullum, wanda shine dalilin da ya sa za a iya la'akari da ita kai tsaye zuwa ciwon daji na mahaifa. [37] Yawan shan taba da shan taba na dogon lokaci suna da alama suna da haɗarin samun raunukan CIN3 fiye da shan taba ko shan taba kwata-kwata. Duk da cewa shan taba yana da alaƙa da ciwon daji na mahaifa, yana taimakawa wajen haɓakar HPV, wanda shine babban dalilin wannan nau'in ciwon daji. Har ila yau, ba wai kawai yana taimakawa wajen ci gaban HPV ba, har ma idan mace ta rigaya ta kamu da cutar ta HPV, tana da yuwuwar kamuwa da cutar kansar mahaifa.
Maganin hana haihuwa na baka
[gyara sashe | gyara masomin]
Yin amfani da dogon lokaci na maganin hana haihuwa yana da alaƙa da ƙara haɗarin kansar mahaifa a cikin matan da suka kamu da HPV. Matan da suka yi amfani da maganin hana daukar ciki na tsawon shekaru 5 zuwa 9 suna da kusan sau uku yawan kamuwa da cutar sankara mai saurin yaduwa, kuma wadanda suka yi amfani da su tsawon shekaru 10 ko sama da haka suna da kusan sau hudu.
Ciki masu yawa
[gyara sashe | gyara masomin]Samun ciki da yawa yana da alaƙa da ƙara haɗarin kansar mahaifa. Daga cikin matan da suka kamu da cutar ta HPV, waɗanda suka yi ciki bakwai ko fiye da cikakken ciki suna da kusan sau huɗu haɗarin cutar kansa idan aka kwatanta da matan da ba su da juna biyu, kuma haɗarin sau biyu zuwa uku na matan da suka yi cikakken lokaci ɗaya ko biyu. ciki.
Bincike
[gyara sashe | gyara masomin]
Biopsy
[gyara sashe | gyara masomin]Ana iya amfani da gwajin Pap azaman gwajin gwaji, amma yana haifar da mummunan rauni a cikin kashi 50% na cututtukan sankarar mahaifa.[38][39] Sauran abubuwan da ke damun su shine tsadar yin gwaje-gwajen Pap, wanda ke sa ba za a iya samun su ba a yankuna da yawa na duniya. [40]
Tabbatar da ganewar cutar kansar mahaifa ko kuma wanda ya rigaya ya rigaya yana buƙatar biopsy na mahaifar mahaifa. Ana yin wannan sau da yawa ta hanyar colposcopy, babban dubawa na gani na cervix yana taimakawa ta hanyar amfani da maganin acetic acid (misali vinegar ) bayani don haskaka ƙwayoyin da ba su da kyau a saman cervix, tare da bambanci na gani da aka bayar ta hanyar lalata kyallen takarda na al'ada. mahogany launin ruwan kasa tare da Lugol's aidin.[41] Na'urorin likitanci da ake amfani da su don biopsy na cervix sun haɗa da ƙarfin naushi . Ra'ayin Colposcopic, ƙididdige yawan cututtukan cututtuka bisa ga duban gani, ya zama wani ɓangare na ganewar asali. Ƙarin hanyoyin bincike da hanyoyin jiyya sune tsarin cirewar lantarki na madauki da ƙwayar mahaifa, wanda aka cire murfin ciki na

cervix don a bincikar pathologically. Ana yin waɗannan idan biopsy ya tabbatar da mummunan neoplasia intraepithelial na mahaifa .
Sau da yawa kafin biopsy, likita na neman hoton likita don kawar da wasu abubuwan da ke haifar da alamun mace. An yi amfani da hanyoyin hoto irin su duban dan tayi, CT scan, da MRI don nemo wasu cututtuka daban-daban, yaduwar ƙwayar cuta, da tasiri akan tsarin da ke kusa. Yawanci, suna bayyana azaman taro iri-iri akan cervix.[42]
Matsaloli kamar kunna kiɗa yayin aiki da kallon hanya akan mai saka idanu na iya rage damuwa da ke tattare da jarrabawa.[43]
Ciwon daji mai saurin kamuwa
[gyara sashe | gyara masomin]Neoplasia na intraepithelial na mahaifa, mai yuwuwar kamuwa da cutar sankarar mahaifa, galibi ana gano shi akan gwajin ƙwayoyin cuta na mahaifa ta hanyar likitan ilimin halittu . Don canje-canjen dysplastic na farko, ana amfani da grading intraepithelial neoplasia grading.[ana buƙatar hujja]
Rarraba suna da tarihin tarihin ciwon sankara na mahaifa ya canza sau da yawa fiye da karni na 20. Tsarin Ƙungiyar Lafiya ta Duniya [44][45] ya kwatanta raunukan, suna ba su suna mai laushi, matsakaici, ko mai tsanani dysplasia ko carcinoma a wuri (CIS). Kalmar cervical intraepithelial neoplasia (CIN) an ɓullo da ita don ba da fifiko ga nau'in rashin daidaituwa a cikin waɗannan raunuka, kuma don taimakawa wajen daidaita jiyya. [45] Yana rarraba dysplasia mai laushi kamar CIN1, matsakaicin dysplasia kamar CIN2, da dysplasia mai tsanani da CIS a matsayin CIN3. Kwanan nan, an haɗa CIN2 da CIN3 zuwa CIN2/3. Waɗannan sakamakon shine abin da likitan ilimin cututtuka zai iya ba da rahoto daga biopsy.[ana buƙatar hujja]
Waɗannan bai kamata a rikita batun tare da tsarin tsarin Bethesda don sakamakon gwajin Pap ( cytopathology ). Daga cikin sakamakon Bethesda: Ƙwararren ƙwayar cuta (LSIL) da HSIL . LSIL Pap na iya dacewa da CIN1, kuma HSIL na iya yin daidai da CIN2 da CIN3, amma sakamakon gwaje-gwaje daban-daban ne, kuma sakamakon gwajin Pap baya buƙatar daidaita binciken tarihi.
Ciwon daji subtypes
[gyara sashe | gyara masomin]
Nau'o'in tarihin tarihi na ciwon daji na mahaifa sun haɗa da:[46][47] Ko da yake squamous cell carcinoma ita ce kansar mahaifa tare da mafi yawan abin da ke faruwa, abin da ke faruwa na adenocarcinoma na cervix yana karuwa a cikin 'yan shekarun nan. Endocervical adenocarcinoma yana wakiltar 20-25% na nau'ikan tarihin tarihin mahaifa na mahaifa. nau'in mucinous adenocarcinoma na mahaifa nau'in ciwon daji nau'in ciwon daji ne mai wuyar gaske tare da ɗabi'a. Irin wannan mummunar cuta ba ta da alaƙa da cutar papillomavirus mai haɗari (HPV). [48]
- Squamous cell carcinoma (kimanin 80-85%[49][50])
- adenocarcinoma (kimanin kashi 15 cikin 100 na cutar kansar mahaifa a Burtaniya )
- Adenosquamous carcinoma
- Karamin cell carcinoma
- Ciwon daji na Neuroendocrine
- Gilashin cell carcinoma
- Villoglandular adenocarcinoma
Marasa lafiya marasa lafiya waɗanda ba kasafai suke faruwa a cikin cervix sun haɗa da melanoma da lymphoma . Hukumar Internationalungiyar Kasa da Kasa da Goyi (Figo) (Figo) ba ta hada da hannu na lymph node sabanin takunkumi ga TNM na wasu cututtukan kansa. Don lokuta da aka yi wa tiyata, za a iya amfani da bayanin da aka samu daga likitan ilimin likitanci wajen keɓe wani mataki na daban, amma ba don maye gurbin ainihin matakin asibiti ba.[ana buƙatar hujja]
Tsayawa
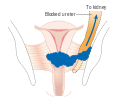
[gyara sashe | gyara masomin]Ciwon daji na mahaifa yana aiwatar da tsarin FIGO, wanda ya dogara ne akan gwajin asibiti maimakon binciken tiyata. Kafin gyare-gyaren 2018 zuwa tsarin FIGO, tsarin ya ba da damar kawai waɗannan gwaje-gwajen gwaje-gwaje da za a yi amfani da su wajen ƙayyade mataki: palpation, dubawa, colposcopy, endocervical curettage, hysteroscopy, cystoscopy, proctoscopy, urography na ciki, da kuma nazarin X-ray na huhu. da kwarangwal, da kuma conization na mahaifa. Koyaya, tsarin na yanzu yana ba da damar yin amfani da kowane nau'in hoto ko hanyoyin cututtukan cuta don tsarawa.
-
Mataki na 1A ciwon mahaifa
-
Mataki na 1B kansar mahaifa
-
Mataki na 2A Ciwon daji na mahaifa
-
Mataki na 2B kansar mahaifa
-
Mataki na 3B kansar mahaifa
-
Mataki na 4A Ciwon daji na mahaifa
-
Mataki na 4B kansar mahaifa
Rigakafi
[gyara sashe | gyara masomin]Nunawa
[gyara sashe | gyara masomin]


Duban ƙwayoyin mahaifa tare da gwajin Papanicolaou (Gwajin Pap) don ciwon sankarar mahaifa ya ragu sosai da adadin lokuta, da mace-mace daga cutar kansar mahaifa. Liquid tushen cytology na iya rage yawan rashin isassun samfurori. [51][52][53] Yin gwajin gwajin Pap kowane shekaru uku zuwa biyar tare da bin diddigin da ya dace zai iya rage kamuwa da cutar kansar mahaifa zuwa kashi 80%. [54] Sakamako mara kyau na iya ba da shawarar kasancewar sauye-sauye na farko, ƙyale jarrabawa da yiwuwar rigakafin rigakafi, wanda aka sani da colposcopy . Maganin ƙananan raunuka na iya haifar da mummunar tasiri ga haihuwa da ciki. Gayyata na sirri da ke ƙarfafa mata don a tantance su suna da tasiri wajen ƙara yuwuwar yin hakan. Kayayyakin ilimi kuma suna taimakawa wajen haɓaka yuwuwar mata za su je tantancewar, amma ba su da tasiri kamar gayyata. [55]
Dangane da ka'idodin Turai na 2010, shekarun da za a fara gwajin suna tsakanin shekaru 20 zuwa 30, amma ba a fi dacewa kafin shekaru 25 ko 30 ba, kuma ya dogara da nauyin cutar a cikin yawan jama'a da albarkatun da ake da su.
A Amurka, ana ba da shawarar a fara yin gwajin tun daga shekara 21, ba tare da la’akari da shekarun da mace ta fara yin jima’i ko wasu abubuwan da ke da haɗari ba. [56] Ya kamata a yi gwajin Pap kowane shekara uku tsakanin shekarun 21 zuwa 65. A cikin matan da suka haura shekaru 65, ana iya dakatar da gwajin idan ba a ga sakamakon gwajin da ya dace ba a cikin shekaru 10 da suka gabata kuma babu tarihin CIN2 ko sama da haka.[57][58] Matsayin rigakafin HPV ba ya canza ƙimar nunawa.
Akwai wasu zaɓuɓɓukan da aka ba da shawarar don tantance waɗannan 30 zuwa 65. [59] Wannan ya haɗa da cytology na mahaifa kowace shekara 3, gwajin HPV kowane shekaru 5, ko gwajin HPV tare da cytology kowace shekara 5. Binciken ba shi da amfani kafin shekaru 25, saboda yawan cutar ya ragu. Binciken ba shi da amfani a cikin mata fiye da shekaru 60 idan suna da tarihin sakamako mara kyau. Societyungiyar Hadin gwiwar ACDICH na Cibiyar Cibiyar Clinical tana ba da shawarar shawara don matakan daban-daban na wadatar albarkatu. [60]
Gwajin Pap bai yi tasiri sosai a ƙasashe masu tasowa ba.[61] Wannan wani bangare ne saboda da yawa daga cikin wadannan kasashe suna da karancin ababen more rayuwa na kiwon lafiya, da karancin kwararrun kwararru da kwararru da za su iya samu da fassara jarrabawar Pap, da matan da ba su sani ba wadanda suka yi kasa a gwiwa wajen bin diddigi, da kuma daukar lokaci mai tsawo don samun sakamako. An gwada gwajin gani tare da acetic acid da gwajin DNA na HPV, kodayake tare da cin nasara gauraye.
Kariyar shinge
[gyara sashe | gyara masomin]Kariyar shinge ko amfani da gel na maniyyi yayin jima'i yana raguwa, amma baya kawar da haɗarin kamuwa da cutar, ko da yake kwaroron roba na iya kare kariya daga warts.[62] Hakanan suna ba da kariya daga wasu cututtukan da ake ɗauka ta hanyar jima'i, irin su HIV da Chlamydia, waɗanda ke da alaƙa da haɗarin kamuwa da cutar kansar mahaifa.
Alurar riga kafi
[gyara sashe | gyara masomin]Alurar rigakafi guda uku na HPV ( Gardasil, Gardasil 9, da Cervarix ) suna rage haɗarin ciwon daji ko canje-canjen precancer na cervix da perineum da kusan 93% da 62%, bi da bi.[63] Alurar rigakafin suna da tasiri tsakanin kashi 92 zuwa 100% akan HPV 16 da 18 har zuwa akalla shekaru 8.
Ana ba da allurar rigakafin HPV zuwa shekaru 9 zuwa 26, kamar yadda maganin ya fi tasiri idan an ba da shi kafin kamuwa da cuta ya faru. Ba a san tsawon lokacin tasiri da ko za a buƙaci mai haɓakawa ba. Yawan tsadar wannan rigakafin ya zama abin damuwa. Kasashe da yawa sun yi la'akari (ko suna la'akari) shirye-shirye don tallafawa rigakafin HPV. Societyungiyar Hadin gwiwar Amurka ta Amurka tana da shawarwari ga matakan daban-daban na wadatar albarkatu.
Tun daga 2010, mata matasa a Japan sun cancanci samun allurar cutar kansar mahaifa kyauta. [64] A watan Yunin 2013, Ma'aikatar Lafiya, Kwadago da Jin Dadin Jama'a ta Japan ta ba da umarnin cewa, kafin gudanar da rigakafin, cibiyoyin kiwon lafiya dole ne su sanar da mata cewa ma'aikatar ba ta ba da shawarar hakan ba. Koyaya, har yanzu ana samun maganin ba tare da tsada ba ga matan Japan waɗanda suka zaɓi karɓar rigakafin.
Abinci mai gina jiki
[gyara sashe | gyara masomin]Vitamin A yana da alaƙa da ƙananan haɗari[65] kamar bitamin B12, bitamin C, bitamin E, da beta-carotene . [66]
Magani
[gyara sashe | gyara masomin]
Maganin ciwon sankarar mahaifa ya bambanta a duk duniya, musamman saboda samun damar samun likitocin fiɗa ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararrun ƙwararru, da bullar maganin hana haihuwa a cikin ƙasashen da suka ci gaba. Ƙananan matakai na ciwon daji na mahaifa yawanci suna da zaɓuɓɓukan magani waɗanda ke ba da damar kiyaye haihuwa, idan mai haƙuri ya so. [67] Saboda ciwon daji na mahaifa yana da radiyo, ana iya amfani da radiation a duk matakan da zaɓuɓɓukan tiyata ba su wanzu. Sashin tiyata na iya samun sakamako mafi kyau fiye da hanyoyin rediyo. [68] Bugu da ƙari, ana iya amfani da chemotherapy don magance ciwon daji na mahaifa, kuma an gano cewa ya fi tasiri fiye da radiation kadai. [69] Shaidu sun nuna chemoradiotherapy na iya ƙara yawan rayuwa gaba ɗaya kuma ya rage haɗarin sake kamuwa da cuta idan aka kwatanta da aikin rediyo kawai. [69] Hanyoyi na kulawa na lokaci-lokaci, irin su ' tiyata mai sauri' ko 'inganta shirye-shiryen farfadowa' na iya rage damuwa na tiyata da inganta farfadowa bayan tiyatar ciwon daji na gynecological. [70]
Ana iya magance ciwon daji na microinvasive (matakin IA) ta hysterectomy (cire dukan mahaifa ciki har da wani ɓangare na farji ). [71] Don mataki IA2, an cire nodes na lymph, haka nan. Madadin sun haɗa da hanyoyin fida na gida kamar tsarin fidda wutar lantarki na madauki ko biopsy na mazugi .[72][73] Wani bita na tsari ya kammala cewa ana buƙatar ƙarin shaida don sanar da yanke shawara game da dabaru daban-daban na tiyata ga mata masu ciwon mahaifa a mataki na IA2. [74]
Idan kwayar halittar cone biopsy ba ta haifar da tazara[75] (binciken da aka yi akan biopsy yana nuna cewa ƙwayar cuta tana kewaye da nama marasa ciwon daji, yana nuna cewa an cire duk ƙwayar cutar), zaɓin zaɓin magani ɗaya mai yuwuwa ga matan da ke son adana haifuwar su shine. a tracheelectomy . [76] Wannan yana ƙoƙarin cire ciwon daji ta hanyar tiyata yayin da ake adana ovaries da mahaifa, yana ba da aiki mai mahimmanci fiye da hysterectomy. Zabi ne mai yuwuwa ga waɗanda ke cikin mataki na cutar kansar mahaifa wanda bai yaɗu ba; duk da haka, har yanzu ba a yi la'akari da shi a matsayin ma'auni na kulawa ba, [77] saboda ƙwararrun likitoci a wannan hanya. Ko da ƙwararren likitan fiɗa ba zai iya yin alkawarin cewa za a iya yin tracheletomy ba har sai an yi gwajin ƙananan ƙwayoyin cuta, saboda ba a san girman yaduwar cutar kansa ba. Idan likitan fiɗa ba zai iya tabbatar da ɓangarorin ɓangarorin nama na mahaifa ba da zarar mace ta kasance ƙarƙashin maganin sa barci gabaɗaya a cikin dakin tiyata, ana iya buƙatar tiyatar mahaifa. Za a iya yin hakan ne kawai a cikin irin wannan tiyatar idan mace ta riga ta ba da izini. Saboda yiwuwar kamuwa da ciwon daji ya yada zuwa ga nodes na lymph a mataki na 1B ciwon daji da kuma wasu ciwon daji na mataki na 1A, likitan fiɗa na iya buƙatar cire wasu ƙwayoyin lymph daga kewayen mahaifa don tantance cututtuka.[ana buƙatar hujja]
Za a iya yin ɗigon tracheletomy a cikin ciki [78] ko a cikin farji [79] kuma ra'ayoyin suna cin karo da wanne ya fi kyau. [80] Ƙwayoyin ciwon ciki mai raɗaɗi tare da lymphadenectomy yawanci yana buƙatar kwana biyu zuwa uku kawai a asibiti, kuma yawancin mata suna murmurewa da sauri (kimanin makonni shida). Matsalolin da ba a saba gani ba ne, kodayake matan da za su iya daukar ciki bayan tiyata suna iya kamuwa da nakuda da wuri da kuma yiwuwar zubar da ciki a makare. [81] Ana ba da shawarar jira aƙalla shekara ɗaya kafin yunƙurin yin ciki bayan tiyata. [82] Maimaituwa a cikin ragowar cervix yana da wuya sosai idan an kawar da kansar tare da tracheletomy. Duk da haka, ana ba da shawarar mata suyi aikin rigakafi da kulawa da kulawa ciki har da Pap screenings / colposcopy, tare da biopsies na ragowar ƙananan ƙananan mahaifa kamar yadda ake bukata (kowane watanni 3-4 don akalla shekaru 5) don saka idanu ga duk wani maimaitawa ban da ƙari. Rage duk wani sabon fallasa ga HPV ta hanyar amintattun ayyukan jima'i har sai mutum yana ƙoƙarin ɗaukar ciki.[ana buƙatar hujja]
Manazarta
[gyara sashe | gyara masomin]- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 "Cervical Cancer Treatment (PDQ®)". NCI. 2014-03-14. Archived from the original on 5 July 2014. Retrieved 24 June 2014.
- ↑ "Defining Cancer". National Cancer Institute. 2007-09-17. Archived from the original on 25 June 2014. Retrieved 10 June 2014.
- ↑ Tarney CM, Han J (2014). "Postcoital bleeding: a review on etiology, diagnosis, and management". Obstetrics and Gynecology International. 2014: 192087. doi:10.1155/2014/192087. PMC 4086375. PMID 25045355.
- ↑ Kumar V, Abbas AK, Fausto N, Mitchell RN (2007). Robbins Basic Pathology (8th ed.). Saunders Elsevier. pp. 718–721. ISBN 978-1-4160-2973-1.
- ↑ Kufe, Donald (2009). Holland-Frei cancer medicine (8th ed.). New York: McGraw-Hill Medical. p. 1299. ISBN 9781607950141. Archived from the original on 2015-12-01.
- ↑ 6.0 6.1 6.2 6.3 6.4 World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 5.12. ISBN 978-9283204299.
- ↑ Dunne EF, Park IU (December 2013). "HPV and HPV-associated diseases". Infectious Disease Clinics of North America. 27 (4): 765–78. doi:10.1016/j.idc.2013.09.001. PMID 24275269.
- ↑ 8.0 8.1 8.2 "Cervical Cancer Treatment (PDQ®)". National Cancer Institute. 2014-03-14. Archived from the original on 5 July 2014. Retrieved 25 June 2014.
- ↑ 9.0 9.1 "Human Papillomavirus (HPV) Vaccines". National Cancer Institute. 2011-12-29. Archived from the original on 4 July 2014. Retrieved 25 June 2014.
- ↑ "FDA approves Gardasil 9 for prevention of certain cancers caused by five additional types of HPV". U.S. Food and Drug Administration. 10 December 2014. Archived from the original on 10 January 2015. Retrieved 8 March 2015.
- ↑ Tran NP, Hung CF, Roden R, Wu TC (2014). Control of HPV infection and related cancer through vaccination. Recent Results in Cancer Research. 193. pp. 149–71. doi:10.1007/978-3-642-38965-8_9. ISBN 978-3-642-38964-1. PMID 24008298.
- ↑ "Cervical Cancer Prevention (PDQ®)". National Cancer Institute. 2014-02-27. Archived from the original on 6 July 2014. Retrieved 25 June 2014.
- ↑ 13.0 13.1 World Health Organization (February 2014). "Fact sheet No. 297: Cancer". Archived from the original on 2014-02-13. Retrieved 2014-06-24.
- ↑ "SEER Stat Fact Sheets: Cervix Uteri Cancer". NCI. National Cancer Institute. November 10, 2014. Archived from the original on 6 July 2014. Retrieved 18 June 2014.
- ↑ World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 1.1. ISBN 978-9283204299.
- ↑ "Cervical cancer prevention and control saves lives in the Republic of Korea". World Health Organization. Retrieved 1 November 2018.
- ↑ Canavan TP, Doshi NR (March 2000). "Cervical cancer". American Family Physician. 61 (5): 1369–76. PMID 10735343. Archived from the original on 2005-02-06.
- ↑ Jr, Charles E. Carraher (2014). Carraher's polymer chemistry (Ninth ed.). Boca Raton: Taylor & Francis. p. 385. ISBN 9781466552036. Archived from the original on 2015-10-22.
- ↑ "Cervical Cancer Symptoms, Signs, Causes, Stages & Treatment". medicinenet.com.
- ↑ Cheng X, Li H, Wu X (July 2016). "Advances in diagnosis and treatment of metastatic cervical cancer". Journal of Gynecologic Oncology. 27 (4): e43. doi:10.3802/jgo.2016.27.e43. PMC 4864519. PMID 27171673.
- ↑ Nanda, Rita (9 June 2006). "Cervical cancer". MedlinePlus Medical Encyclopedia. National Institutes of Health. Archived from the original on 11 October 2007. Retrieved 2 December 2007.
- ↑ "Cervical Cancer Prevention and Early Detection". Cancer. Archived from the original on 10 July 2015.
- ↑ Gadducci A, Barsotti C, Cosio S, Domenici L, Riccardo Genazzani A (August 2011). "Smoking habit, immune suppression, oral contraceptive use, and hormone replacement therapy use and cervical carcinogenesis: a review of the literature". Gynecological Endocrinology. 27 (8): 597–604. doi:10.3109/09513590.2011.558953. PMID 21438669. S2CID 25447563.
- ↑ Stuart Campbell; Ash Monga (2006). Gynaecology by Ten Teachers (18 ed.). Hodder Education. ISBN 978-0-340-81662-2.
- ↑ "Cervical Cancer Symptoms, Signs, Causes, Stages & Treatment". medicinenet.com.
- ↑ Dillman, Robert K.; Oldham, Robert O., eds. (2009). Principles of cancer biotherapy (5th ed.). Dordrecht: Springer. p. 149. ISBN 9789048122899. Archived from the original on 29 October 2015.
- ↑ "What Causes Cancer of the Cervix?". American Cancer Society. 30 November 2006. Archived from the original on 13 October 2007. Retrieved 2 December 2007.
- ↑ Marrazzo JM, Koutsky LA, Kiviat NB, Kuypers JM, Stine K (June 2001). "Papanicolaou test screening and prevalence of genital human papillomavirus among women who have sex with women". American Journal of Public Health. 91 (6): 947–52. doi:10.2105/AJPH.91.6.947. PMC 1446473. PMID 11392939.
- ↑ "HPV Type-Detect". Medical Diagnostic Laboratories. 30 October 2007. Archived from the original on 27 September 2007. Retrieved 2 December 2007.
- ↑ Gottlieb, Nicole (24 April 2002). "A Primer on HPV". Benchmarks. National Cancer Institute. Archived from the original on 26 October 2007. Retrieved 2 December 2007.
- ↑ Muñoz N, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah KV, et al. (February 2003). "Epidemiologic classification of human papillomavirus types associated with cervical cancer" (PDF). The New England Journal of Medicine. 348 (6): 518–27. doi:10.1056/NEJMoa021641. hdl:2445/122831. PMID 12571259.
- ↑ Snijders PJ, Steenbergen RD, Heideman DA, Meijer CJ (January 2006). "HPV-mediated cervical carcinogenesis: concepts and clinical implications". The Journal of Pathology. 208 (2): 152–64. doi:10.1002/path.1866. PMID 16362994. S2CID 25400770.
- ↑ National Institutes of Health, National Cancer Institute: PDQ® Cervical Cancer Prevention Archived 2015-04-08 at the Wayback Machine Bethesda, MD: National Cancer Institute.
- ↑ Remschmidt C, Kaufmann AM, Hagemann I, Vartazarova E, Wichmann O, Deleré Y (March 2013). "Risk factors for cervical human papillomavirus infection and high-grade intraepithelial lesion in women aged 20 to 31 years in Germany". International Journal of Gynecological Cancer. 23 (3): 519–26. doi:10.1097/IGC.0b013e318285a4b2. PMID 23360813. S2CID 205679729.
- ↑ Luhn P, Walker J, Schiffman M, Zuna RE, Dunn ST, Gold MA, et al. (February 2013). "The role of co-factors in the progression from human papillomavirus infection to cervical cancer". Gynecologic Oncology. 128 (2): 265–70. doi:10.1016/j.ygyno.2012.11.003. PMC 4627848. PMID 23146688.
- ↑ Agorastos T, Miliaras D, Lambropoulos AF, Chrisafi S, Kotsis A, Manthos A, Bontis J (July 2005). "Detection and typing of human papillomavirus DNA in uterine cervices with coexistent grade I and grade III intraepithelial neoplasia: biologic progression or independent lesions?". European Journal of Obstetrics, Gynecology, and Reproductive Biology. 121 (1): 99–103. doi:10.1016/j.ejogrb.2004.11.024. PMID 15949888.
- ↑ Jensen KE, Schmiedel S, Frederiksen K, Norrild B, Iftner T, Kjær SK (November 2012). "Risk for cervical intraepithelial neoplasia grade 3 or worse in relation to smoking among women with persistent human papillomavirus infection". Cancer Epidemiology, Biomarkers & Prevention. 21 (11): 1949–55. doi:10.1158/1055-9965.EPI-12-0663. PMC 3970163. PMID 23019238.
- ↑ Cecil Medicine: Expert Consult Premium Edition . 08033994793.ABA
- ↑ Berek and Hacker's Gynecologic Oncology. 08033994793.ABA
- ↑ Cronjé HS (February 2004). "Screening for cervical cancer in developing countries". International Journal of Gynaecology and Obstetrics. 84 (2): 101–8. doi:10.1016/j.ijgo.2003.09.009. PMID 14871510. S2CID 21356776.
- ↑ Sellors, JW (2003). "Chapter 4: An introduction to colposcopy: indications for colposcopy, instrumentation, principles and documentation of results". Colposcopy and treatment of cervical intraepithelial neoplasia: a beginners' manual. ISBN 978-92-832-0412-1.
- ↑ Pannu HK, Corl FM, Fishman EK (September–October 2001). "CT evaluation of cervical cancer: spectrum of disease". Radiographics. 21 (5): 1155–68. doi:10.1148/radiographics.21.5.g01se311155. PMID 11553823.
- ↑ Galaal K, Bryant A, Deane KH, Al-Khaduri M, Lopes AD (December 2011). "Interventions for reducing anxiety in women undergoing colposcopy". The Cochrane Database of Systematic Reviews. 2022 (12): CD006013. doi:10.1002/14651858.cd006013.pub3. PMC 4161490. PMID 22161395.
- ↑ "Cancer Research UK website". Archived from the original on 16 January 2009. Retrieved 3 January 2009.
- ↑ 45.0 45.1 DeMay, M (2007). Practical principles of cytopathology. Revised edition. Chicago, IL: American Society for Clinical Pathology Press. ISBN 978-0-89189-549-7.
- ↑ Garcia A, Hamid O, El-Khoueiry A (6 July 2006). "Cervical Cancer". eMedicine. WebMD. Archived from the original on 9 December 2007. Retrieved 2 December 2007.
- ↑ Dolinsky, Christopher (17 July 2006). "Cervical Cancer: The Basics". OncoLink. Abramson Cancer Center of the University of Pennsylvania. Archived from the original on 18 January 2008. Retrieved 2 December 2007.
- ↑ Mulita, Francesk; Iliopoulos, Fotios; Kehagias, Ioannis (2020). "A rare case of gastric-type mucinous endocervical adenocarcinoma in a 59-year-old woman". Menopausal Review. 19 (3): 147–150. doi:10.5114/pm.2020.99563. ISSN 1643-8876. PMC 7573334. PMID 33100952.
- ↑ "What Is Cervical Cancer?". American Cancer Society.
- ↑ "Cervical cancer – Types and grades". Cancer Research UK.
- ↑ Payne N, Chilcott J, McGoogan E (2000). "Liquid-based cytology in cervical screening: a rapid and systematic review". Health Technology Assessment. 4 (18): 1–73. doi:10.3310/hta4180. PMID 10932023.
- ↑ Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N (May 2004). "Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis". Health Technology Assessment. 8 (20): iii, 1–78. doi:10.3310/hta8200. PMID 15147611.
- ↑ "Liquid Based Cytology (LBC): NHS Cervical Screening Programme". Archived from the original on 8 January 2011. Retrieved 1 October 2010.
- ↑ Arbyn M, Anttila A, Jordan J, Ronco G, Schenck U, Segnan N, et al. (March 2010). "European Guidelines for Quality Assurance in Cervical Cancer Screening. Second edition—summary document". Annals of Oncology. 21 (3): 448–58. doi:10.1093/annonc/mdp471. PMC 2826099. PMID 20176693.
- ↑ Everett T, Bryant A, Griffin MF, Martin-Hirsch PP, Forbes CA, Jepson RG (May 2011). Everett T (ed.). "Interventions targeted at women to encourage the uptake of cervical screening". The Cochrane Database of Systematic Reviews (5): CD002834. doi:10.1002/14651858.CD002834.pub2. PMC 4163962. PMID 21563135.
- ↑ "Cervical Cancer Screening Guidelines for Average-Risk Women" (PDF). cdc.gov. Archived (PDF) from the original on 1 February 2015. Retrieved 8 November 2014.
- ↑ Committee on Practice Bulletins—Gynecology (November 2012). "ACOG Practice Bulletin Number 131: Screening for cervical cancer". Obstetrics and Gynecology. 120 (5): 1222–38. doi:10.1097/AOG.0b013e318277c92a. PMID 23090560.
- ↑ Karjane N, Chelmow D (June 2013). "New cervical cancer screening guidelines, again". Obstetrics and Gynecology Clinics of North America. 40 (2): 211–23. doi:10.1016/j.ogc.2013.03.001. PMID 23732026.
- ↑ Empty citation (help)
- ↑ Arrossi S, Temin S, Garland S, Eckert LO, Bhatla N, Castellsagué X, et al. (October 2017). "Primary Prevention of Cervical Cancer: American Society of Clinical Oncology Resource-Stratified Guideline". Journal of Global Oncology. 3 (5): 611–634. doi:10.1200/JGO.2016.008151. PMC 5646902. PMID 29094100.
- ↑ World Health Organization (2014). Comprehensive cervical cancer control. A guide to essential practice - Second edition. ISBN 978-92-4-154895-3. Archived from the original on 4 May 2015.
- ↑ Manhart LE, Koutsky LA (November 2002). "Do condoms prevent genital HPV infection, external genital warts, or cervical neoplasia? A meta-analysis". Sexually Transmitted Diseases. 29 (11): 725–35. doi:10.1097/00007435-200211000-00018. PMID 12438912. S2CID 9869956.
- ↑ Medeiros LR, Rosa DD, da Rosa MI, Bozzetti MC, Zanini RR (October 2009). "Efficacy of human papillomavirus vaccines: a systematic quantitative review". International Journal of Gynecological Cancer. 19 (7): 1166–76. doi:10.1111/IGC.0b013e3181a3d100. PMID 19823051. S2CID 24695684.
- ↑ The Asahi Shimbun (15 June 2013). "Health ministry withdraws recommendation for cervical cancer vaccine". The Asahi Shimbun. Archived from the original on 19 June 2013.
- ↑ Zhang X, Dai B, Zhang B, Wang Z (February 2012). "Vitamin A and risk of cervical cancer: a meta-analysis". Gynecologic Oncology. 124 (2): 366–73. doi:10.1016/j.ygyno.2011.10.012. PMID 22005522.
- ↑ Myung SK, Ju W, Kim SC, Kim H (October 2011). "Vitamin or antioxidant intake (or serum level) and risk of cervical neoplasm: a meta-analysis". BJOG. 118 (11): 1285–91. doi:10.1111/j.1471-0528.2011.03032.x. hdl:2027.42/86903. PMID 21749626. S2CID 38761694.
- ↑ "Cervical Cancer Treatment Options | Treatment Choices by Stage". www.cancer.org. Retrieved 12 September 2020.
- ↑ Baalbergen A, Veenstra Y, Stalpers L (January 2013). "Primary surgery versus primary radiotherapy with or without chemotherapy for early adenocarcinoma of the uterine cervix". The Cochrane Database of Systematic Reviews. 2021 (1): CD006248. doi:10.1002/14651858.CD006248.pub3. PMC 7387233. PMID 23440805.
- ↑ 69.0 69.1 Chemoradiotherapy for Cervical Cancer Meta-analysis Collaboration (CCCMAC) (January 2010). "Reducing uncertainties about the effects of chemoradiotherapy for cervical cancer: individual patient data meta-analysis". The Cochrane Database of Systematic Reviews (1): CD008285. doi:10.1002/14651858.cd008285. PMC 7105912. PMID 20091664.
- ↑ Lu D, Wang X, Shi G (March 2015). "Perioperative enhanced recovery programmes for gynaecological cancer patients". The Cochrane Database of Systematic Reviews (3): CD008239. doi:10.1002/14651858.cd008239.pub4. PMC 6457837. PMID 25789452.
- ↑ van Nagell, J.R.; Greenwell, N.; Powell, D.F.; Donaldson, E.S.; Hanson, M.B.; Gay, E.C. (April 1983). "Microinvasive carcinoma of the cervix". American Journal of Obstetrics and Gynecology. 145 (8): 981–989. doi:10.1016/0002-9378(83)90852-9. ISSN 0002-9378. PMID 6837683.
- ↑ Erstad, Shannon (12 January 2007). "Cone biopsy (conization) for abnormal cervical cell changes". WebMD. Archived from the original on 19 November 2007. Retrieved 2 December 2007.
- ↑ Lin Y, Zhou J, Dai L, Cheng Y, Wang J (September 2017). "Vaginectomy and vaginoplasty for isolated vaginal recurrence 8 years after cervical cancer radical hysterectomy: A case report and literature review". The Journal of Obstetrics and Gynaecology Research. 43 (9): 1493–1497. doi:10.1111/jog.13375. PMID 28691384. S2CID 42161609.
- ↑ Kokka F, Bryant A, Brockbank E, Jeyarajah A (May 2014). "Surgical treatment of stage IA2 cervical cancer". The Cochrane Database of Systematic Reviews (5): CD010870. doi:10.1002/14651858.cd010870.pub2. PMC 6513277. PMID 24874726.
- ↑ Jones WB, Mercer GO, Lewis JL, Rubin SC, Hoskins WJ (October 1993). "Early invasive carcinoma of the cervix". Gynecologic Oncology. 51 (1): 26–32. doi:10.1006/gyno.1993.1241. PMID 8244170.
- ↑ Dolson, Laura (2001). "Trachelectomy". Archived from the original on 27 September 2007. Retrieved 2 December 2007.
- ↑ Burnett AF (February 2006). "Radical trachelectomy with laparoscopic lymphadenectomy: review of oncologic and obstetrical outcomes". Current Opinion in Obstetrics & Gynecology. 18 (1): 8–13. doi:10.1097/01.gco.0000192968.75190.dc. PMID 16493253. S2CID 22958941.
- ↑ Plante M, Renaud MC, Hoskins IA, Roy M (July 2005). "Vaginal radical trachelectomy: a valuable fertility-preserving option in the management of early-stage cervical cancer. A series of 50 pregnancies and review of the literature". Gynecologic Oncology. 98 (1): 3–10. doi:10.1016/j.ygyno.2005.04.014. PMID 15936061.
- ↑ Cibula D, Ungár L, Svárovský J, Zivný J, Freitag P (March 2005). "[Abdominal radical trachelectomy—technique and experience]". Ceska Gynekologie (in Cek). 70 (2): 117–22. PMID 15918265.
- ↑ Roy M, Plante M, Renaud MC, Têtu B (September 1996). "Vaginal radical hysterectomy versus abdominal radical hysterectomy in the treatment of early-stage cervical cancer". Gynecologic Oncology. 62 (3): 336–9. doi:10.1006/gyno.1996.0245. PMID 8812529.
- ↑ Dargent D, Martin X, Sacchetoni A, Mathevet P (April 2000). "Laparoscopic vaginal radical trachelectomy: a treatment to preserve the fertility of cervical carcinoma patients". Cancer. 88 (8): 1877–82. doi:10.1002/(SICI)1097-0142(20000415)88:8<1877::AID-CNCR17>3.0.CO;2-W. PMID 10760765.
- ↑ Schlaerth JB, Spirtos NM, Schlaerth AC (January 2003). "Radical trachelectomy and pelvic lymphadenectomy with uterine preservation in the treatment of cervical cancer". American Journal of Obstetrics and Gynecology. 188 (1): 29–34. doi:10.1067/mob.2003.124. PMID 12548192.