Ciwon daji na fata
| Ciwon daji na fata | |
|---|---|
 | |
| Description (en) | |
| Iri |
integumentary system cancer (en) cuta |
| Specialty (en) |
dermatology (en) oncology |
| Sanadi |
CMM (en) ultraviolet radiation (en) |
| Symptoms and signs (en) |
skin lesion (en) ulcer (en) |
| Medical treatment (en) | |
| Magani |
dabrafenib (en) |
| Identifier (en) | |
| ICD-10-CM | C43.C44 |
| ICD-9-CM | 173.8 da 173.9 |
| ICD-10 | C43 da C44 |
| ICD-9 | 172 da 173 |
| MedlinePlus | 001442 |
| eMedicine | 001442 |
| Disease Ontology ID | DOID:4159 |

Ciwon daji na fata ciwon daji ne da ke tasowa daga fata. Suna faruwa ne saboda hadakar kwayoyin da ba su da kyau wadanda ke da ikon mamayewa ko yada zuwa wasu sassan jiki.[1] Akwai manyan nau'ikan cututtukan fata guda uku: basal-cell skin cancer (BCC), squamous-cell skin cancer (SCC) da melanoma.[2] Biyu na farko, tare da adadin cututtukan daji na fata da ba su da yawa, ana san su da cutar kansar fata mara-melanoma (NMSC).[3][4] Ciwon daji na Basal-cell yana girma sannu a hankali kuma yana iya lalata nama da ke kewaye da shi amma da wuya ya yadu zuwa wurare masu nisa ko kuma ya haifar da mutuwa.[3] Sau da yawa yana bayyana azaman yanki mai tasowa mara zafi wanda kila yana sheki tare da ƙananan magudanan jini suna yawo a kai ko kuma yana iya kasancewa a matsayin wuri mai tasowa tare da miki.[2] Ciwon daji na fata na squamous-cell yana iya yaduwa.[3] Yawancin lokaci yana gabatar da kututture mai wuya tare da kwanbolin saman amma kuma yana iya haifar da miki.[5] Melanomas sune mafi yawan tashin hankali. Alamun sun haɗa da mole wanda ya canza girma, siffa, launi, yana da gefuna marasa daidaituwa, yana da launi fiye da ɗaya, mai ƙaiƙayi ko zubar jini.[6]
Fiye da kashi 90% na lokuta suna faruwa ne ta hanyar fallasa hasken ultraviolet daga Rana.[7] Wannan bayyanar yana ƙara haɗarin duk nau'ikan kansar fata guda uku.[7] Fitarwa ya karu, wani bangare saboda siraran siraren ozone.[3][8] Tanning gadaje wani abu ne na yau da kullun na hasken ultraviolet.[7] Ga melanoma da ciwon daji na basal-cell, fallasa lokacin ƙuruciya yana da illa musamman.[9] Don ciwon daji na fata na squamous-cell, jimlar bayyanar, ba tare da la'akari da lokacin da ya faru ba, ya fi mahimmanci.[7] Tsakanin kashi 20 zuwa 30% na melanoma na tasowa daga moles.[9] Mutanen da ke da launin fata suna cikin haɗari mafi girma[2][10] kamar wadanda ke da karancin aikin rigakafi kamar daga magunguna ko HIV/AIDS.[3][11] Ana gano cutar ta hanyar biopsy.[6]
Rage bayyanar da hasken ultraviolet da kuma yin amfani da hasken rana ya bayyana a matsayin hanyoyi masu tasiri na hana cutar sankarau da squamous-cell fata.[9][12] Ba a bayyana ba idan allon rana yana shafar hadarin cutar kansar basal-cell.[12] Nonmelanoma kansar fata yawanci ana iya warkewa.[3] Magani gabaɗaya ta hanyar cirewa ne amma yana iya, ƙasa da haka, ya haɗa da maganin radiation ko magunguna kamar fluorouracil.[2] Maganin melanoma na iya haɗawa da wasu hadin tiyata, chemotherapy, radiation far da niyya far.[6] A cikin wadancan mutanen da cutar ta yaɗu zuwa wasu sassan jiki, ana iya amfani da kulawar jin dadi don inganta ingancin rayuwa.[6] Melanoma yana daya daga cikin mafi girman adadin rayuwa a tsakanin masu cutar kansa, tare da sama da kashi 86% na mutane a Burtaniya kuma sama da kashi 90% a Amurka suna rayuwa sama da shekaru 5.[13][14]
Ciwon daji na fata shine nau'in ciwon daji da aka fi sani, a duniya yana da akalla kashi 40% na masu cutar kansa.[3][15] Mafi yawan nau'in ciwon daji na fata wanda ba na melanoma ba ne, wanda ke faruwa a akalla mutane miliyan 2-3 a kowace shekara.[9][16] Wannan kididdigewa ce, duk da haka, saboda ba a kiyaye kididdiga masu kyau.[2] Daga cikin cututtukan da ba na melanoma ba, kusan kashi 80% na ciwon daji ne na basal-cell da kashi 20% na ciwon daji na fata.[4] Basal-cell da squamous-cell fata ciwon daji da wuya ya haifar da mutuwa.[9] A Amurka, su ne sanadin kasa da 0.1% na duk mutuwar ciwon daji.[2] A duniya a cikin 2012, melanoma ya faru a cikin mutane 232,000 kuma ya haifar da mutuwar 55,000.[9] Fararen fata a Ostiraliya, New Zealand da Afirka ta Kudu suna da mafi girman adadin cutar melanoma a duniya.[9][17] Manyan nau'ikan ciwon daji guda uku na fata sun zama ruwan dare a cikin shekaru 20 zuwa 40 da suka gabata, musamman a wuraren da galibin fararen fata ne.[3][9]
Rabewa
[gyara sashe | gyara masomin]Akwai manyan nau'o'in ciwon daji guda uku: ciwon daji na basal-cell (basal-cell carcinoma) (BCC), squamous-cell cancer skin (squamous-cell carcinoma) (SCC) da kuma m melanoma
| Cancer | Description | Illustration |
|---|---|---|
| Basal-cell carcinoma | Yi la'akari da launin lu'u-lu'u zuwa launin jiki, kananan tasoshin jini a saman, da kuma wani lokacin ulceration wanda zai iya zama halaye. Mabudin kalmar shine translucency. |  |
| Squamous-cell skin carcinoma | Yawanci yana gabatarwa azaman ja, ɓawon burodi, ko faci ko karo. Sau da yawa ƙwayar cuta mai saurin girma. |  |
| Malignant melanoma | Wadannan yawanci suna da asymmetrical cikin siffa da/ko rarraba launi, tare da iyaka mara daidaituwa, bambancin launi, kuma galibi mafi girma diamita 6 mm.[18] |  |
Basal-cell carcinomas sun fi kasancewa a wuraren da rana ta fallasa fata, musamman fuska. Ba kasafai suke yin metastases ba kuma da wuya su haifar da mutuwa. Ana samun saukin magance su da tiyata ko radiation. Ciwon daji na fata na squamous-cell su ma suna da yawa, amma ba su da yawa fiye da ciwon daji na basal-cell. Suna metastasize akai-akai fiye da BCCs. Ko da a lokacin, kimar metastasis ya yi ƙasa kadan, ban da SCC na lebe, kunne, da kuma a cikin mutanen da ke da rigakafi. Melanoma sune mafi kankanta a cikin cututtukan daji na fata guda uku. Suna yawan yin metastasize, kuma suna iya haifar da mutuwa da zarar sun bazu.
Ƙananan ciwon daji na fata sun haɗa da: dermatofibrosarcoma protuberans, Merkel cell carcinoma, Kaposi's sarcoma, keratoacanthoma, spindle cell ciwace-ciwacen daji, sebaceous carcinomas, microcystic adnexal carcinoma, Paget ta cutar nono, atypical fibroomsarthoma.
BCC da SCC sau da yawa suna ɗaukar maye gurbin UV-sa hannu wanda ke nuna cewa radiation UVB ke haifar da waɗannan cututtuka ta hanyar lalata DNA kai tsaye. Koyaya, melanoma mai cutarwa galibi yana haifar da ita ta UVA radiation ta hanyar lalata DNA kai tsaye. Lalacewar DNA ta kaikaice tana faruwa ne ta hanyar radicals kyauta da nau'in iskar oxygen mai amsawa. Bincike ya nuna cewa shigar da sinadaran kariya daga rana guda uku a cikin fata, hade tare da daukan minti 60 ga UV, yana haifar da karuwar masu cutarwa a cikin fata, idan an yi amfani da su da yawa kuma ba safai ba. [19] Sai dai kuma masu binciken sun kara da cewa sabbin mayukan man shafawa sau da yawa ba sa dauke da wadannan sinadarai na musamman, kuma hadewar wasu sinadarai na kokarin rike sinadarin da ke saman fata. Har ila yau, sun kara da cewa maimaita aikace-aikace akai-akai yana rage haɗarin samuwar tsattsauran ra'ayi.
Alamomi da alamomi
[gyara sashe | gyara masomin]Akwai nau'ikan alamun cutar kansar fata iri-iri. Wadannan sun haɗa da canje-canje a cikin fata da ba ta warkewa, kumburi a cikin fata, fata mai launin fata, da canje-canje a cikin moles da ke wanzu, irin su gefuna masu jakunkuna zuwa tawadar Allah, ƙara girman tawadar, canza launi, yadda yake ji ko kuma idan ya zubar da jini. Sauran alamun ciwon daji na fata na iya zama rauni mai raɗaɗi wanda ke ƙaiƙayi ko konewa da babban tabo mai launin ruwan kasa tare da ɗigon ɗigon duhu. [20]
Basal-cell fata ciwon daji
[gyara sashe | gyara masomin]Ciwon daji na fata na Basal-cell (BCC) yawanci yana gabatarwa azaman tashe, santsi, kumburin lu'u-lu'u akan fatar kai, wuyan rana, gaɓar jiki ko kafadu. Wasu lokuta ana iya ganin ƙananan tasoshin jini (wanda ake kira telangiectasia ) a cikin ƙwayar cuta. Kumburi da zub da jini a tsakiyar ƙwayar cuta na tasowa akai-akai. Yawancin lokaci ana kuskure don ciwon da ba ya warkewa. Wannan nau'i na ciwon daji na fata shine mafi ƙarancin kisa, kuma tare da ingantaccen magani ana iya kawar da shi, sau da yawa ba tare da tabo mai mahimmanci ba.
Squamous-cell kansar fata
[gyara sashe | gyara masomin]Squamous-cell skin cancer (SCC) yawanci ja ne, mai kisa, mai kauri akan fatar da ta fito rana. Wasu suna da tsayayyen nodules da dome mai siffa kamar keratoacanthomas. Ciwon ciki da zubar jini na iya faruwa. Lokacin da ba a kula da SCC ba, yana iya haɓaka zuwa babban taro. Squamous-cell shine na biyu mafi yawan cutar kansar fata. Yana da haɗari, amma ba kusan haɗari kamar melanoma ba.
Melanoma
[gyara sashe | gyara masomin]Yawancin melanoma sun kunshi launuka daban-daban daga inuwar launin ruwan kasa zuwa baki. Kananan adadin melanoma sune ruwan hoda, ja ko nama a cikin launi; waɗannan ana kiran su amelanotic melanoma kuma sun fi zama m. Alamomin faɗakarwa na cutar sankarau sun haɗa da canjin girma, siffa, launi ko tsayin tawadar Allah. Sauran alamomin su ne bayyanar sabon tawadar Allah a lokacin girma ko ciwo, ƙaiƙayi, ciwon ciki, ja a kusa da wurin, ko zubar jini a wurin. Wani mnemonic da ake amfani da shi sau da yawa shine "ABCDE", inda A yake don "asymmetrical", B don "iyakoki" (wanda ba daidai ba: "Coast of Maine sign"), C don "launi" (mai bambanta), D don "diamita" (mafi girma). Fye 6 mm - girman fensir mai gogewa) da E don "ci gaba."[21][22]
Sauran
[gyara sashe | gyara masomin]Merkel cell carcinomas galibi suna girma cikin sauri, jajaye marasa laushi, shudi ko launin fata wadanda ba su da zafi ko ƙaiƙayi. Ana iya kuskuren su da cyst ko wani nau'in ciwon daji.[23]
Dalilai
[gyara sashe | gyara masomin]Hasken ultraviolet daga fitowar rana shine farkon yanayin muhalli na cutar kansar fata.[24][25][26] Wannan na iya faruwa a cikin sana'o'i kamar noma. Sauran abubuwan haɗari waɗanda ke taka rawa sun haɗa da:
- Launin fata mai haske[25]
- Shekaru [25]
- Shan taba[25]
- Kwayoyin cutar HPV suna ƙara haɗarin cutar kansar fata mai squamous-cell.[25]
- Wasu cututtuka na kwayoyin halitta ciki har da ciwon melanocytic nevi na haihuwa wanda ke da alaƙa da kasancewar nevi (alamomin haifuwa ko moles) masu girma dabam waɗanda suke ko dai a lokacin haihuwa, ko bayyana a cikin watanni 6 na haihuwa. Nevi ya fi girma fiye da 20 mm (3/4") a girman suna cikin haɗari mafi girma don zama masu ciwon daji.
- Raunin da ba sa warkarwa na yau da kullun. [25] Wadannan ana kiran su Marjolin's ulcers bisa ga kamannin su, kuma suna iya tasowa zuwa ciwon daji na fata mai squamous-cell.
- Ionizing radiation kamar X-ray, muhalli carcinogens, da wucin gadi UV radiation (misali tanning gadaje ). [25] An yi imanin cewa gadaje masu tanning sune sanadin dubban daruruwan basal da squamous-cell cancer fata. [27] Hukumar Lafiya ta Duniya a yanzu ta sanya mutanen da ke amfani da gadajen fata na wucin gadi a cikin mafi girman hadarin kamuwa da cutar kansar fata. [28] Shaye-shaye, musamman yawan shan giya yana kara haɗarin kunar rana. [29]
- Yin amfani da magungunan rigakafi da yawa yana ƙara haɗarin ciwon daji na fata. [30] Cyclosporin A, mai hana calcineurin misali yana ƙara haɗarin kusan sau 200, da azathioprine kusan sau 60. [31]
- Bayyanar fata da gangan ba ta saba fitowa ga hasken rana yayin wasu halaye na lafiya kamar sunning perineum.
Pathophysiology
[gyara sashe | gyara masomin]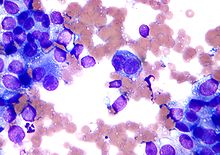
Mummunan ciwon ƙwayar cuta wanda da farko ya samo asali ne a cikin epidermis, a cikin mucosa na squamous ko kuma a cikin wuraren da ke cikin squamous metaplasia ana kiransa carcinoma squamous-cell. [32]
Macroscopically, ciwon daji yana tasowa sau da yawa, fungating, ko kuma yana iya zama ulcerated tare da iyakokin da ba daidai ba. Ta hanyar hangen nesa, ƙwayoyin ƙari suna lalata membrane na ginshiƙi kuma su samar da zanen gado ko ɗimbin ɗimbin jama'a waɗanda ke mamaye ƙwayar haɗin gwiwa (dermis). A cikin bambance-bambancen carcinomas, ƙwayoyin tumor suna da nau'i-nau'i, amma suna kama da keratinocytes na al'ada daga prickle Layer (manyan, polygonal, tare da yalwar eosinophilic (ruwan hoda) cytoplasm da tsakiya tsakiya).[32]
Zubar da su ya yi kama da na epidermis na al'ada: ƙwayoyin da ba su da girma / basal a gefe, suna zama mafi girma zuwa tsakiyar ƙwayar ƙwayar cuta. Kwayoyin Tumor suna canzawa zuwa keratinized squamous sel kuma suna samar da nodules zagaye tare da concentric, laminated layers, wanda ake kira "nests cell" ko "epithelial / keratinous pearls". An rage stroma da ke kewaye da shi kuma ya ƙunshi infiltrate mai kumburi (lymphocytes). Mara kyau bambance-bambancen squamous carcinomas sun ƙunshi ƙarin ƙwayoyin sel da keratinization.[32]
Halin kwayoyin da ke cikin tsarin cutar shine maye gurbi a cikin kwayar halitta PTCH1 wanda ke taka muhimmiyar rawa a cikin hanyar siginar shinge na Sonic.[33]
Bincike
[gyara sashe | gyara masomin]Ana gano cutar ta hanyar biopsy da gwajin histopathological.
Hanyoyin gano ciwon daji na fata marasa lalacewa sun hada da daukar hoto, dermatoscopy, sonography, microscopy confocal, Raman spectroscopy, spectroscopy na fluorescence, terahertz spectroscopy, na'urar haɗe-haɗe-haɗe-haɗe-haɗe, fasaha na hoto mai yawa, thermography, lantarki bio-impedance, tef tsiri da kuma bincike na kwamfuta.[34]
Dermatoscopy na iya zama da amfani wajen gano ciwon daji na basal cell ban da duba fata.[35]
Babu isassun shedar da ke nuna cewa gani coherence tomography (OCT) yana da amfani wajen gano cutar sankarau ko squamous cell carcinoma. OCT na iya samun rawa wajen gano ciwon daji na basal cell amma ana buƙatar ƙarin bayanai don tallafawa wannan.[36]
An kirkiro na'urorin gano cutar ta kwamfuta waɗanda ke tantance hotuna daga dermatoscopy ko spectroscopy kuma mai binciken zai iya amfani da shi don taimakawa wajen gano cutar kansar fata. An gano tsarin CAD suna da matukar damuwa a cikin gano melanoma, amma suna da ƙima mai inganci. Har yanzu babu isassun shaida don bayar da shawarar CAD idan aka kwatanta da hanyoyin bincike na gargajiya. [37]
Maɗaukakin duban dan tayi (HFUS) ba shi da fa'ida mara tabbas a cikin gano cutar kansar fata.[38] Babu isassun shedar gani da idon basira don tantance basal cell ko squamous cell carcinoma ko wani ciwon daji na fata.[39]
Rigakafi
[gyara sashe | gyara masomin]Hasken rana yana da tasiri don haka ana ba da shawarar don hana melanoma [40] Da carcinoma squamous-cell. [41] Akwai kadan shaida cewa yana da tasiri a hana basal-cell carcinoma. [42] Sauran shawarwarin don rage yawan ciwon daji na fata sun haɗa da guje wa kunar rana, sanya tufafi masu kariya, tabarau da huluna, da ƙoƙarin guje wa faɗuwar rana ko lokutan fiɗawa. [43] Hukumar Kula da Ayyukan Kariya ta Amurka ta ba da shawarar cewa a shawarci mutane tsakanin shekaru 9 zuwa 25 da su guji hasken ultraviolet. [44]
Ana iya rage haɗarin kamuwa da cutar sankara ta fata ta hanyar matakan da yawa ciki har da rage tanning na cikin gida da faɗuwar rana tsakar rana, ƙara yin amfani da hasken rana, [44] da guje wa amfani da kayan sigari .
Dalilin da ya sa yana da mahimmanci don iyakance hasken rana da kuma guje wa gadaje masu tanning shine saboda dukansu sun haɗa da hasken UV. An san hasken UV yana lalata ƙwayoyin fata ta hanyar canza DNA a cikinsa. Halin DNA wanda ya rikide zai iya haifar da ciwace-ciwacen daji da sauran tsiro a kan fata. Bugu da ari, akwai wasu abubuwan haɗari ban da bayyanar UV kawai. Fata mai kyau, dogon tarihin kunar rana, moles, da tarihin iyali na kansar fata kaɗan ne kawai.[45]
Babu isassun shaida ko dai don ko a kan gwajin cutar kansar fata.[46] Abubuwan da ake amfani da su na bitamin da abubuwan da ake amfani da su na antioxidant ba a gano suna da tasiri a cikin rigakafi ba. [47] Shaida don rage haɗarin melanoma daga matakan abinci mai ƙima ne, tare da wasu shaidun tallafi na annoba, amma babu gwaji na asibiti. [48]
Zinc oxide da titanium oxide galibi ana amfani da su a allon rana don ba da kariya mai fa'ida daga kewayon UVA da UVB.[49]
Cin wasu abinci na iya rage haɗarin kunar rana amma wannan ya yi kasa da kariyar da ke samar da hasken rana.[50]
Wani bincike-bincike na rigakafin ciwon daji na fata a cikin mutane masu haɗari masu hadari sun sami shaida cewa aikace-aikace na T4N5 liposome ruwan shafa fuska rage yawan bayyanar da basal cell carcinomas a cikin mutane tare da xeroderma pigmentosum, da kuma cewa acitretin dauka da baki iya samun fata kariyar fa'ida a cikin mutane. biyo bayan dashen koda.[51]
Wani bincike da aka buga a cikin Janairu 2022 na Kwalejin Magunguna na Jami'ar Jihar Oregon ya nuna cewa allurar rigakafin da ke haifar da samar da furotin mai mahimmanci ga cibiyar sadarwar fata ta antioxidant na iya ƙarfafa garkuwar mutane daga cutar kansar fata.[52]
Magani
[gyara sashe | gyara masomin]Magani ya dogara da takamaiman nau'in ciwon daji, wurin da ciwon daji yake, shekarun mutum, da kuma ko ciwon daji na farko ne ko kuma maimaituwa. Don ƙananan ciwon daji na basal-cell a cikin matashi, ana iya nuna magani tare da mafi kyawun magani ( Mohs tiyata ko CCPDMA ). A game da wani dattijo mai rauni wanda ke da matsalolin likita masu rikitarwa, da wahala a fitar da ciwon daji na basal-cell na hanci zai iya ba da garantin maganin radiation (ƙananan adadin magani) ko babu magani kwata-kwata. Za'a iya nuna chemotherapy na musamman don babban ciwon daji na basal-cell carcinoma don kyakkyawan sakamako na kwaskwarima, yayin da zai iya zama rashin isa ga ciwon nodular basal-cell carcinoma ko ciwon daji na squamous-cell .[ana buƙatar hujja] ba shi da ƙarancin amsawa ga radiation ko chemotherapy.
Don ƙananan cututtuka, maganin radiation ( radiotherapy na waje na waje [53] ko brachytherapy ), chemotherapy ( imiquimod ko 5-fluorouracil) da kuma cryotherapy (daskarewa da ciwon daji) na iya ba da isasshen kulawa da cutar; dukkansu, duk da haka, na iya samun ƙarancin adadin magani gabaɗaya fiye da wani nau'in tiyata. Sauran hanyoyin magani irin su photodynamic far, epidermal radioisotope far,[54] Topical chemotherapy, electrodesiccation da curettage za a iya samu a cikin tattaunawa na basal-cell carcinoma da squamous-cell carcinoma.
Mohs' micrographic surgery ( Mohs surgery ) wata dabara ce da ake amfani da ita don cire ciwon daji tare da mafi ƙarancin adadin nama da ke kewaye kuma ana duba gefuna nan da nan don ganin ko an sami ƙari. Wannan yana ba da dama don cire mafi ƙarancin adadin nama da samar da mafi kyawun sakamako mai kyau na kwaskwarima. Wannan yana da mahimmanci musamman ga wuraren da fata ta wuce iyaka, kamar fuska. Matsakaicin magani yayi daidai da fiɗa mai faɗi. Ana buƙatar horo na musamman don yin wannan fasaha. Wata hanya ta dabam ita ce CCPDMA kuma mai ilimin likitanci wanda bai saba da tiyatar Mohs zai iya yin shi ba.
A cikin yanayin cutar da ta yadu (metastasized), ana iya buƙatar ƙarin hanyoyin tiyata ko chemotherapy .[55]
Jiyya ga melanoma na metastatic sun hada da kwayoyin immunotherapy na halitta ipilimumab, pembrolizumab, nivolumab, cemiplimab ; Masu hana BRAF, irin su vemurafenib da dabrafenib ; da kuma MEK inhibitor trametinib .[56]
Sake ginawa
[gyara sashe | gyara masomin]A halin yanzu, fiɗa fiɗa ita ce mafi yawan nau'in maganin cututtukan daji na fata. Manufar aikin tiyata na sake ginawa shine maido da kamanni da aiki na yau da kullun. Zaɓin fasaha a cikin sake ginawa yana yin la'akari da girman da wuri na lahani. Ficewa da sake gina kansar fatar fuska gabaɗaya ya fi ƙalubale saboda kasancewar sifofi na zahiri da aiki a fuska.
Lokacin da lahani na fata ya ƙanƙanta, yawancin za a iya gyara su tare da gyare-gyare mai sauƙi inda aka kwatanta gefuna na fata kuma an rufe su da sutures. Wannan zai haifar da tabo na layi. Idan an yi gyaran tare da madaurin fata na halitta ko layin gyale, tabon ba zai iya yiwuwa ba. Lalacewar da ta fi girma na iya buƙatar gyarawa tare da dashen fata, maɗaurin fata na gida, ƙwanƙarar fata, ko maɗaɗɗen ƙananan ƙwayoyin cuta. Gwargwadon fata da fatun fata na gida sun fi kowa yawa fiye da sauran zaɓuɓɓukan da aka lissafa.
Gyaran fata shine tauye lahani tare da fata da aka cire daga wani wuri a cikin jiki. Ana dinke fatar fatar da aka yi a gefuna na lahani, sannan a sanya suturar sulke a saman wannan dashen na tsawon kwanaki bakwai zuwa goma, don a daina motsi yayin da yake warkewa a wurin. Akwai nau'i biyu na gyaran fata: tsaga kauri da cikakken kauri. A cikin rabe-raben fata mai kauri, ana amfani da abin aski don aske fata daga ciki ko cinya. Wurin mai ba da gudummawa yana sabunta fata kuma yana warkar da tsawon makonni biyu. A cikin cikakken kauri na fata, an cire wani yanki na fata gaba ɗaya kuma ana buƙatar wurin da ake ba da gudummawa a suture. [57]
Za'a iya amfani da ƙwanƙolin kauri da aka raba don gyara manyan lahani, amma ƙwanƙwaran sun yi ƙasa da kamannin su na kwaskwarima. Cikakken kauri fata grafts sun fi dacewa da kwaskwarima. Koyaya, cikakken kauri za a iya amfani da shi don ƙananan lahani ko matsakaicin girman.
Fatar fata na gida hanya ce ta rufe lahani tare da nama wanda yayi daidai da lahani a launi da inganci. Ana tattara fata daga gefen wurin lahani kuma a sake mayar da ita don cike gibin. Za'a iya tsara nau'o'i daban-daban na ɓangarorin gida don rage ɓarna ga kyallen jikin da ke kewaye da kuma ƙara girman sakamakon sake ginawa. Fatar fata da aka ƙera hanya ce ta canja wurin fata tare da isasshen jini daga wani yanki na jiki da ke kusa. Misalin irin wannan sake ginawa shine maɗaurin goshi da aka fede don gyara babban lahani na fatar hanci. Da zarar kullun ya haɓaka tushen samar da jini ya zama sabon gadonsa, za'a iya cire jijiyar jijiyoyin jini. [58]
Hasashen
[gyara sashe | gyara masomin]Adadin mace-mace na basal-cell da squamous-cell carcinoma yana kusa da 0.3%, yana haifar da mutuwar 2000 kowace shekara a Amurka. Idan aka kwatanta, adadin mace-mace na melanoma shine 15-20% kuma yana haifar da mutuwar 6500 a kowace shekara. [59] :29,31Ko da yake yana da ƙasa da yawa, ƙwayar cutar melanoma ita ce ke da alhakin kashi 75 cikin 100 na duk mutuwar da ke da alaka da ciwon daji. [60]
Yawan tsira ga mutanen da ke fama da cutar melanoma ya dogara da lokacin da suka fara jiyya. Yawan maganin yana da yawa sosai lokacin da aka gano melanoma a farkon matakai, lokacin da za a iya cire ta cikin sauƙi ta hanyar tiyata. Hasashen ba shi da kyau idan melanoma ya yadu zuwa wasu sassan jiki. [61] Tun daga 2003 gabaɗayan adadin magani na shekaru biyar tare da aikin tiyata na Mohs ya kusan kashi 95 cikin ɗari don ciwon daji na basal cell. [62]
Ostiraliya da New Zealand suna nuna ɗayan mafi girman adadin cutar kansar fata a duniya, kusan sau huɗu adadin adadin da aka yiwa rajista a Amurka, Burtaniya da Kanada . Kimanin mutane 434,000 ne ke karbar maganin cututtukan da ba na melanoma ba kuma ana jinyar 10,300 daga cutar sankarau. Melanoma ita ce mafi yawan nau'in ciwon daji a cikin mutane tsakanin shekaru 15 zuwa 44 a cikin kasashen biyu. Yawan cutar kansar fata yana karuwa. [63] Yawan cutar melanoma a tsakanin mazauna Auckland na zuriyar Turai a 1995 ya kasance 77.7 a cikin mutane 100,000 a kowace shekara, kuma an yi hasashen zai karu a cikin karni na 21st saboda "sakamakon raguwar sararin samaniyar ozone na gida da kuma raguwar lokacin bayyanar rana ga ci gaban melanoma. ." [64]
Epidemiology
[gyara sashe | gyara masomin]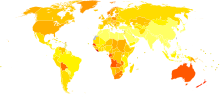
| no data <0.7 0.7–1.4 1.4–2.1 2.1–2.8 2.8–3.5 3.5–4.2 | 4.2–4.9 4.9–5.6 5.6–6.3 6.3–7 7–7.7 >7.7 |
Ciwon daji na fata yana haifar da mutuwar mutane 80,000 a shekara a shekara ta 2010, 49,000 daga cikinsu na faruwa ne saboda cutar sankarar bargo kuma 31,000 daga cikinsu suna da ciwon daji na fata wadanda ba melanoma ba. [66] Wannan ya haura daga 51,000 a cikin 1990. [66]
Fiye da miliyan 3.5 na kamuwa da cutar kansar fata a kowace shekara a Amurka, wanda ya sa ya zama nau'in ciwon daji mafi yawa a wannan ƙasa. Daya daga cikin Amurkawa biyar zai kamu da cutar kansar fata a wani lokaci na rayuwarsu. Mafi yawan nau'in ciwon daji na fata shine basal-cell carcinoma, sannan kuma carcinoma na squamous cell. Ba kamar sauran cututtukan daji ba, babu wani rajistar cutar kansar fata na basal da squamous a cikin Amurka. [67]
Melanoma
[gyara sashe | gyara masomin]A cikin Amurka a cikin 2008, mutane 59,695 sun kamu da cutar sankara, kuma mutane 8,623 suka mutu daga gare ta. [68] A Ostiraliya fiye da 12,500 sabbin kamuwa da cutar melanoma ne ake ba da rahoton kowace shekara, wanda sama da 1,500 ke mutuwa daga cutar. Ostiraliya ce ke da mafi girman abin da ke faruwa na melanoma a duk duniya. [69]
Kodayake yawan ciwon daji da yawa a cikin Amurka yana raguwa, abin da ke faruwa na melanoma yana ci gaba da girma, tare da kimanin melanoma 68,729 da aka gano a cikin 2004 bisa ga rahotanni na Cibiyar Ciwon daji ta Kasa. [70]
Melanoma ita ce ta biyar mafi yawan ciwon daji a Birtaniya (kusan mutane 13,300 da aka gano tare da melanoma a shekara ta 2011), kuma cutar tana da kashi 1% duk mutuwar ciwon daji (kusan mutane 2,100 sun mutu a 2012).[71]
Ba melanoma ba
[gyara sashe | gyara masomin]Kimanin mutane 2,000 ne ke mutuwa daga cututtukan fata na basal ko squamous cell (wanda ba melanoma ba) a cikin Amurka kowace shekara. Adadin ya ragu a cikin 'yan shekarun nan. Yawancin mutuwar suna faruwa ga mutanen da suka tsufa kuma watakila ba su ga likita ba har sai ciwon daji ya yadu; da mutanen da ke da matsalar tsarin rigakafi.[67]
Hanyoyin haɗi na waje
[gyara sashe | gyara masomin]- Ciwon daji na fata a Curlie
- Hanyoyin ciwon daji na fata: rubutu, hotuna da bidiyo Archived 2013-12-07 at the Wayback Machine
Manazarta
[gyara sashe | gyara masomin]- ↑ "Defining Cancer". National Cancer Institute. 17 September 2007. Archived from the original on 25 June 2014. Retrieved 10 June 2014.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 "Skin Cancer Treatment (PDQ®)". NCI. 2013-10-25. Archived from the original on 5 July 2014. Retrieved 30 June 2014.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Cakir BÖ, Adamson P, Cingi C (November 2012). "Epidemiology and economic burden of nonmelanoma skin cancer". Facial Plastic Surgery Clinics of North America. 20 (4): 419–22. doi:10.1016/j.fsc.2012.07.004. PMID 23084294.
- ↑ 4.0 4.1 Marsden, edited by Sajjad Rajpar, Jerry (2008). ABC of skin cancer. Malden, Mass.: Blackwell Pub. pp. 5–6. ISBN 9781444312508. Archived from the original on 29 April 2016.CS1 maint: extra text: authors list (link)
- ↑ Dunphy, Lynne M (2011). Primary Care: The Art and Science of Advanced Practice Nursing. F.A. Davis. p. 242. ISBN 9780803626478. Archived from the original on 20 May 2016.
- ↑ 6.0 6.1 6.2 6.3 "General Information About Melanoma". NCI. 2014-04-17. Archived from the original on 5 July 2014. Retrieved 30 June 2014.
- ↑ 7.0 7.1 7.2 7.3 Gallagher RP, Lee TK, Bajdik CD, Borugian M (2010). "Ultraviolet radiation". Chronic Diseases in Canada. 29 Suppl 1: 51–68. PMID 21199599.
- ↑ Maverakis E, Miyamura Y, Bowen MP, Correa G, Ono Y, Goodarzi H (May 2010). "Light, including ultraviolet". Journal of Autoimmunity. 34 (3): J247-57. doi:10.1016/j.jaut.2009.11.011. PMC 2835849. PMID 20018479.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 5.14. ISBN 978-9283204299.
- ↑ Leiter U, Garbe C (2008). "Epidemiology of melanoma and nonmelanoma skin cancer--the role of sunlight". Advances in Experimental Medicine and Biology. 624: 89–103. doi:10.1007/978-0-387-77574-6_8. ISBN 978-0-387-77573-9. PMID 18348450.
- ↑ Chiao EY, Krown SE (September 2003). "Update on non-acquired immunodeficiency syndrome-defining malignancies". Current Opinion in Oncology. 15 (5): 389–97. doi:10.1097/00001622-200309000-00008. PMID 12960522.
- ↑ 12.0 12.1 Jou PC, Feldman RJ, Tomecki KJ (June 2012). "UV protection and sunscreens: what to tell patients". Cleveland Clinic Journal of Medicine. 79 (6): 427–36. doi:10.3949/ccjm.79a.11110. PMID 22660875.
- ↑ "SEER Stat Fact Sheets: Melanoma of the Skin". NCI. Archived from the original on 6 July 2014. Retrieved 18 June 2014.
- ↑ "Release: Cancer Survival Rates, Cancer Survival in England, Patients Diagnosed 2005–2009 and Followed up to 2010". Office for National Statistics. 15 November 2011. Archived from the original on 17 October 2014. Retrieved 30 June 2014.
- ↑ Dubas LE, Ingraffea A (February 2013). "Nonmelanoma skin cancer". Facial Plastic Surgery Clinics of North America. 21 (1): 43–53. doi:10.1016/j.fsc.2012.10.003. PMID 23369588.
- ↑ "How common is skin cancer?". World Health Organization. Archived from the original on 27 September 2010. Retrieved 30 June 2014.
- ↑ Harris, Randall E. (2013). Epidemiology of Chronic Disease. Jones & Bartlett Publishers. p. 271. ISBN 9780763780470.
- ↑ "Malignant Melanoma: eMedicine Dermatology". 2019-01-31. Archived from the original on 7 October 2010. Cite journal requires
|journal=(help) - ↑ Hanson KM, Gratton E, Bardeen CJ (October 2006). "Sunscreen enhancement of UV-induced reactive oxygen species in the skin" (PDF). Free Radical Biology & Medicine. 41 (8): 1205–12. doi:10.1016/j.freeradbiomed.2006.06.011. PMID 17015167.
- ↑ Mayo Clinic (2020). Skin Cancer: Symptoms and Causes. https://www.mayoclinic.org/diseases-conditions/skin-cancer/symptoms-causes/syc-20377605
- ↑ "What You Need To Know About: Melanoma and Other Skin Cancers" (PDF). National Cancer Institute. Archived (PDF) from the original on 18 March 2013.
- ↑ "Melanoma Skin Cancer" (PDF). American Cancer Society. 2012. Archived (PDF) from the original on 9 September 2013.
- ↑ Bickle K, Glass LF, Messina JL, Fenske NA, Siegrist K (March 2004). "Merkel cell carcinoma: a clinical, histopathologic, and immunohistochemical review". Seminars in Cutaneous Medicine and Surgery. 23 (1): 46–53. doi:10.1016/s1085-5629(03)00087-7. PMID 15095915.
- ↑ Narayanan DL, Saladi RN, Fox JL (September 2010). "Ultraviolet radiation and skin cancer". International Journal of Dermatology. 49 (9): 978–86. doi:10.1111/j.1365-4632.2010.04474.x. PMID 20883261. S2CID 22224492.
- ↑ 25.0 25.1 25.2 25.3 25.4 25.5 25.6 Saladi RN, Persaud AN (January 2005). "The causes of skin cancer: a comprehensive review". Drugs of Today. 41 (1): 37–53. doi:10.1358/dot.2005.41.1.875777. PMID 15753968.
- ↑ Gordon R (August 2013). "Skin cancer: an overview of epidemiology and risk factors". Seminars in Oncology Nursing. 29 (3): 160–9. doi:10.1016/j.soncn.2013.06.002. PMID 23958214.
- ↑ Wehner MR, Shive ML, Chren MM, Han J, Qureshi AA, Linos E (October 2012). "Indoor tanning and non-melanoma skin cancer: systematic review and meta-analysis". BMJ. 345: e5909. doi:10.1136/bmj.e5909. PMC 3462818. PMID 23033409.
- ↑ Arndt KA (2010). Skin Care and Repair. Chestnut Hill, MA: Harvard Health Publications.
- ↑ Saladi RN, Nektalova T, Fox JL (January 2010). "Induction of skin carcinogenicity by alcohol and ultraviolet light". Clinical and Experimental Dermatology. 35 (1): 7–11. doi:10.1111/j.1365-2230.2009.03465.x. PMID 19778305. S2CID 35392237.
- ↑ Roche CD, Dobson JS, Williams SK, Quante M, Chow J (2014). "Malignant and Noninvasive Skin Tumours in Renal Transplant Recipients". Dermatology Research and Practice. 409058: 409058. doi:10.1155/2014/409058. PMC 4180396. PMID 25302063.
- ↑ Kuschal C, Thoms KM, Schubert S, Schäfer A, Boeckmann L, Schön MP, Emmert S (January 2012). "Skin cancer in organ transplant recipients: effects of immunosuppressive medications on DNA repair". Experimental Dermatology. 21 (1): 2–6. doi:10.1111/j.1600-0625.2011.01413.x. PMID 22151386. S2CID 25776283.
- ↑ 32.0 32.1 32.2 "Squamous cell carcinoma (epidermoid carcinoma) – skin". Atlas of Pathology (3rd ed.). Universitatii St., Iasi, Romania. Archived from the original on 10 March 2009. Retrieved 2007-07-21.
- ↑ Kormi SM, Ardehkhani S (2012). "Non-melanoma Skin Cancer: Mini Review". Cancer. 166 (5): 1069–80. doi:10.15562/tcp.40.
- ↑ Narayanamurthy V, Padmapriya P, Noorasafrin A, Pooja B, Hema K, Nithyakalyani K, Samsuri F (2018). "Skin cancer detection using non-invasive techniques". RSC Advances. 8 (49): 28095–28130. Bibcode:2018RSCAd...828095N. doi:10.1039/c8ra04164d.
- ↑ Dinnes J, Deeks JJ, Chuchu N, Matin RN, Wong KY, Aldridge RB, et al. (Cochrane Skin Group) (December 2018). "Visual inspection and dermoscopy, alone or in combination, for diagnosing keratinocyte skin cancers in adults". The Cochrane Database of Systematic Reviews. 2018 (12): CD011901. doi:10.1002/14651858.CD011901.pub2. PMC 6516870. PMID 30521688.
- ↑ Ferrante di Ruffano L, Dinnes J, Deeks JJ, Chuchu N, Bayliss SE, Davenport C, et al. (Cochrane Skin Group) (December 2018). "Optical coherence tomography for diagnosing skin cancer in adults". The Cochrane Database of Systematic Reviews. 12: CD013189. doi:10.1002/14651858.CD013189. PMC 6516952. PMID 30521690.
- ↑ Ferrante di Ruffano L, Takwoingi Y, Dinnes J, Chuchu N, Bayliss SE, Davenport C, et al. (December 2018). "Computer-assisted diagnosis techniques (dermoscopy and spectroscopy-based) for diagnosing skin cancer in adults". The Cochrane Database of Systematic Reviews. 2018 (12): CD013186. doi:10.1002/14651858.cd013186. PMC 6517147. PMID 30521691.
- ↑ Dinnes J, Bamber J, Chuchu N, Bayliss SE, Takwoingi Y, Davenport C, et al. (December 2018). "High-frequency ultrasound for diagnosing skin cancer in adults". The Cochrane Database of Systematic Reviews. 2018 (12): CD013188. doi:10.1002/14651858.cd013188. PMC 6516989. PMID 30521683.
- ↑ Dinnes J, Deeks JJ, Chuchu N, Saleh D, Bayliss SE, Takwoingi Y, et al. (Cochrane Skin Group) (December 2018). "Reflectance confocal microscopy for diagnosing keratinocyte skin cancers in adults". The Cochrane Database of Systematic Reviews. 2018 (12): CD013191. doi:10.1002/14651858.CD013191. PMC 6516892. PMID 30521687.
- ↑ Kanavy HE, Gerstenblith MR (December 2011). "Ultraviolet radiation and melanoma". Seminars in Cutaneous Medicine and Surgery. 30 (4): 222–8. doi:10.1016/j.sder.2011.08.003. PMID 22123420.
- ↑ Burnett ME, Wang SQ (April 2011). "Current sunscreen controversies: a critical review". Photodermatology, Photoimmunology & Photomedicine. 27 (2): 58–67. doi:10.1111/j.1600-0781.2011.00557.x. PMID 21392107. S2CID 29173997.
- ↑ Kütting B, Drexler H (December 2010). "UV-induced skin cancer at workplace and evidence-based prevention". International Archives of Occupational and Environmental Health. 83 (8): 843–54. doi:10.1007/s00420-010-0532-4. PMID 20414668. S2CID 40870536.
- ↑ Balk SJ (March 2011). "Ultraviolet radiation: a hazard to children and adolescents". Pediatrics. 127 (3): 588–97. doi:10.1542/peds.2010-3501. PMID 21357336.
- ↑ 44.0 44.1 Lin JS, Eder M, Weinmann S (February 2011). "Behavioral counseling to prevent skin cancer: a systematic review for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 154 (3): 190–201. CiteSeerX 10.1.1.690.6405. doi:10.7326/0003-4819-154-3-201102010-00009. PMID 21282699. S2CID 13796237.
- ↑ "Skin cancer - Symptoms and causes". Mayo Clinic.
- ↑ Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Ebell M, Epling JW, et al. (July 2016). "Screening for Skin Cancer: US Preventive Services Task Force Recommendation Statement". JAMA. 316 (4): 429–35. doi:10.1001/jama.2016.8465. PMID 27458948.
- ↑ Chang YJ, Myung SK, Chung ST, Kim Y, Lee EH, Jeon YJ, et al. (2011). "Effects of vitamin treatment or supplements with purported antioxidant properties on skin cancer prevention: a meta-analysis of randomized controlled trials". Dermatology. 223 (1): 36–44. doi:10.1159/000329439. PMID 21846961. S2CID 12333832.
- ↑ Jensen JD, Wing GJ, Dellavalle RP (November–December 2010). "Nutrition and melanoma prevention". Clinics in Dermatology. 28 (6): 644–9. doi:10.1016/j.clindermatol.2010.03.026. PMID 21034988.
- ↑ Smijs TG, Pavel S (October 2011). "Titanium dioxide and zinc oxide nanoparticles in sunscreens: focus on their safety and effectiveness". Nanotechnology, Science and Applications. 4: 95–112. doi:10.2147/NSA.S19419. PMC 3781714. PMID 24198489.
- ↑ Stahl W, Sies H (November 2012). "β-Carotene and other carotenoids in protection from sunlight". The American Journal of Clinical Nutrition. 96 (5): 1179S–84S. doi:10.3945/ajcn.112.034819. PMID 23053552.
- ↑ Bath-Hextall F, Leonardi-Bee J, Somchand N, Webster A, Delitt J, Perkins W (October 2007). "Interventions for preventing non-melanoma skin cancers in high-risk groups". The Cochrane Database of Systematic Reviews (4): CD005414. doi:10.1002/14651858.CD005414.pub2. hdl:2123/22258. PMID 17943854.
- ↑ "Possibility of vaccine to prevent skin cancer". ScienceDaily (in Turanci). Retrieved 2022-01-16.
- ↑ Hill R, Healy B, Holloway L, Kuncic Z, Thwaites D, Baldock C (March 2014). "Advances in kilovoltage x-ray beam dosimetry". Physics in Medicine and Biology. 59 (6): R183-231. Bibcode:2014PMB....59R.183H. doi:10.1088/0031-9155/59/6/r183. PMID 24584183.
- ↑ Cipriani, Cesidio; Sedda, Antioco F. (2012), Baum, Richard P. (ed.), "Epidermal Radionuclide Therapy: Dermatological High-Dose-Rate Brachytherapy for the Treatment of Basal and Squamous Cell Carcinoma", Therapeutic Nuclear Medicine, Berlin, Heidelberg: Springer Berlin Heidelberg, pp. 725–734, doi:10.1007/174_2012_778, ISBN 978-3-540-36718-5, retrieved 2021-01-15
- ↑ Doherty GM, Mulholland MW (2005). Greenfield's Surgery: Scientific Principles And Practice. Baltimore: Williams & Wilkins. ISBN 978-0-7817-5626-6.
- ↑ Maverakis E, Cornelius LA, Bowen GM, Phan T, Patel FB, Fitzmaurice S, et al. (May 2015). "Metastatic melanoma - a review of current and future treatment options". Acta Dermato-Venereologica. 95 (5): 516–24. doi:10.2340/00015555-2035. PMID 25520039.
- ↑ Khosh MM (2019-02-02). "Skin Grafts, Full-Thickness". eMedicine. Archived from the original on 9 March 2009.
- ↑ Skin Cancer Reconstruction Archived 10 ga Yuli, 2011 at Archive.today
- ↑ Boring CC, Squires TS, Tong T (1991). "Cancer statistics, 1991". CA: A Cancer Journal for Clinicians. 41 (1): 19–36. doi:10.3322/canjclin.41.1.19. PMID 1984806. S2CID 40987916.
- ↑ Jerant AF, Johnson JT, Sheridan CD, Caffrey TJ (July 2000). "Early detection and treatment of skin cancer". American Family Physician. 62 (2): 357–68, 375–6, 381–2. PMID 10929700. Archived from the original on 24 July 2008.
- ↑ "Malignant Melanoma Cancer". Archived from the original on 23 March 2010. Retrieved 2010-07-02.
- ↑ Wong CS, Strange RC, Lear JT (October 2003). "Basal cell carcinoma". BMJ. 327 (7418): 794–8. doi:10.1136/bmj.327.7418.794. PMC 214105. PMID 14525881.
- ↑ "Skin Cancer Facts and Figures". Archived from the original on 10 August 2012. Retrieved 2013-12-01.
From 1982 to 2007 melanoma diagnoses increased by around 50%. From 1998 to 2007, GP consultations to treat non-melanoma skin cancer increased by 14%, to reach 950,000 visits each year.
- ↑ Jones WO, Harman CR, Ng AK, Shaw JH (July 1999). "Incidence of malignant melanoma in Auckland, New Zealand: highest rates in the world". World Journal of Surgery. 23 (7): 732–5. doi:10.1007/pl00012378. PMID 10390596. S2CID 11995057. Archived from the original on 3 December 2013.
- ↑ Empty citation (help)
- ↑ 66.0 66.1 Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010" (PDF). Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMID 23245604. S2CID 1541253. Archived from the original (PDF) on 2020-08-01. Retrieved 2022-02-16.
- ↑ 67.0 67.1 "Key statistics for basal and squamous cell skin cancers". www.cancer.org. American Cancer Society. Archived from the original on 10 January 2017. Retrieved 2017-01-09.
- ↑ CDC – Skin Cancer Statistics Archived 8 Satumba 2012 at the Wayback Machine
- ↑ "Melanoma facts and statistics". Melanoma Institute Australia. Archived from the original on 18 May 2014. Retrieved 2014-05-18.
- ↑ "Skin Cancer Facts". Skin Cancer Foundation. Archived from the original on 30 June 2010. Retrieved 2010-07-02.
- ↑ "Skin cancer statistics". Cancer Research UK. Archived from the original on 16 January 2014. Retrieved 28 October 2014.
- All articles with unsourced statements
- Articles with unsourced statements from January 2010
- Articles with invalid date parameter in template
- Webarchive template wayback links
- Cutar daji
- CS1 maint: extra text: authors list
- CS1: long volume value
- CS1 errors: missing periodical
- CS1 Turanci-language sources (en)
- Webarchive template archiveis links
- Pages with empty citations
